Abstract
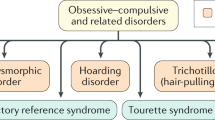
An important challenge in mental health research is to translate findings from cognitive neuroscience and neuroimaging research into effective treatments that target the neurobiological alterations involved in psychiatric symptoms. To address this challenge, in this review we propose a heuristic neurocircuit-based taxonomy to guide the treatment of obsessive–compulsive disorder (OCD). We do this by integrating information from several sources. First, we provide case vignettes in which patients with OCD describe their symptoms and discuss different clinical profiles in the phenotypic expression of the condition. Second, we link variations in these clinical profiles to underlying neurocircuit dysfunctions, drawing on findings from neuropsychological and neuroimaging studies in OCD. Third, we consider behavioral, pharmacological, and neuromodulatory treatments that could target those specific neurocircuit dysfunctions. Finally, we suggest methods of testing this neurocircuit-based taxonomy as well as important limitations to this approach that should be considered in future research.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Association; Arlington, VA 2013.
World Health Organization. The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. World Health Organization; Geneva, Switzerland 1993.
Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Med. 2013;11:126.
Cross-Disorder Group of the Psychiatric Genomics Consortium. Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet. 2013;381:1371–9.
van den Heuvel MP, Sporns O. A cross-disorder connectome landscape of brain dysconnectivity. Nat Rev Neurosci. 2019;20:435–46.
Wang T, Zhang X, Li A, Zhu M, Liu S, Qin W, et al. Polygenic risk for five psychiatric disorders and cross-disorder and disorder-specific neural connectivity in two independent populations. NeuroImage: Clin. 2017;14:441–9.
Williams LM. Precision psychiatry: a neural circuit taxonomy for depression and anxiety. Lancet Psychiatry. 2016;3:472–80.
Wager TD, Woo CW. Imaging biomarkers and biotypes for depression. Nat Med. 2017;23:16–17. https://doi.org/10.1038/nm.4264.
Clementz BA, Sweeney JA, Hamm JP, Ivleva EI, Ethridge LE, Pearlson GD, et al. Identification of distinct psychosis biotypes using brain-based biomarkers. Am J Psychiatry. 2016;173:373–84.
Barth B, Mayer-Carius K, Strehl U, Kelava A, Häußinger FB, Fallgatter AJ, et al. Identification of neurophysiological biotypes in attention deficit hyperactivity disorder. Psychiatry Clin Neurosci. 2018;72:836–48.
Dougherty DD, Brennan BP, Stewart SE, Wilhel S, Widge AS, Rauch SL. Neuroscientifically informed formulation and treatment planning for patients with obsessive-compulsive disorder: a review. JAMA Psychiatry. 2018;75:1081–7.
Graybiel AM, Rauch SL. Toward a neurobiology of obsessive-compulsive disorder. Neuron. 2000;28:343–7.
Milad MR, Rauch SL. Obsessive-compulsive disorder: beyond segregated cortico-striatal pathways. Trends Cogn Sci. 2012;16:43–51.
Stein DJ, Costa DLC, Lochner C, Miguel EC, Reddy YCJ, Shavitt RG, et al. Obsessive–compulsive disorder. Nat Rev Dis Primers. 2019;5:1–26.
Gillan CM, Fineberg NA, Robbins TW. A trans-diagnostic perspective on obsessive-compulsive disorder. Psychol Med. 2017;47:1528–48.
van den Heuvel OA, van Wingend G, Soriano-Mase C, Alonso P, Chamberlain SR, Nakamae T, et al. Brain circuitry of compulsivity. Eur Neuropsychopharmacol. 2016;26:810–27.
Torres AR, Prince MJ, Bebbington PE, Bhugra D, Brugha TS, Farrell M, et al. Obsessive-compulsive disorder: prevalence, comorbidity, impact, and help-seeking in the British National Psychiatric Morbidity survey of 2000. Am J Psychiatry. 2006;163:1978–85.
Bloch MH, Green C, Kichuk SA, Dombrowski PA, Wasylink S, Billingslea E, et al. Long-term outcome in adults with obsessive-compulsive disorder. Depress Anxiety. 2013;30:716–22.
Hollander E, Stein DJ, Kwon JH, Rowland C, Wong CM, Broatch J, et al. Psychosocial function and economic costs of obsessive-compulsive disorder. CNS Spectr. 1997;2:16–25.
Fernández de la Cruz L, Rydell M, Runeson B, D’Onofrio BM, Brander G, Rück C, et al. Suicide in obsessive-compulsive disorder: a population-based study of 36 788 Swedish patients. Mol Psychiatry. 2017;22:1626–32.
Miguel EC, Leckman JF, Rauch S, do Rosario-Campos MC, Hounie AG, Mercadante MT, et al. Obsessive-compulsive disorder phenotypes: implications for genetic studies. Mol Psychiatry. 2005;10:258–75.
Miguel EC, Prado HS, Rauch SL, Coffey BJ, Baer L, Savage CR, et al. Sensory phenomena in obsessive-compulsive disorder and Tourette’s disorder. J Clin Psychiatry. 2000;61:150–6.
Gillan CM, Papmeyer M, Morein-Zamir S, Sahakian BJ, Fineberg NA, Robbins TW, et al. Disruption in the balance between goal-directed behavior and habit learning in obsessive-compulsive disorder. Am J Psychiatry. 2011;168:718–26.
Ferreira GM, Yücel M, Dawson A, Lorenzetti V, Fontenelle LF. Investigating the role of anticipatory reward and habit strength in obsessive-compulsive disorder. CNS Spectr. 2017;22:295–304.
Endrass T, Klawohn J, Schuster F, Kathmann N. Overactive performance monitoring in obsessive-compulsive disorder: ERP evidence from correct and erroneous reactions. Neuropsychologia. 2008;46:1877–87.
de Avila RCS, do Nascimento LG, de Moura Porto RL, Fontenelle L, Miguel Filho EC, Brakoulias V, et al. Level of insight in patients with obsessive–compulsive disorder: an exploratory comparative study between patients with “good insight” and “poor insight”. Front Psychiatry. 2019;10:413.
Mataix-Cols D, Rauch SL, Manzo PA, Jenike MA, Baer L. Use of factor-analyzed symptom dimensions to predict outcome with serotonin reuptake inhibitors and placebo in the treatment of obsessive-compulsive disorder. Am J Psychiatry. 1999;156:1409–16.
Miguel EC, Baer L, Coffey BJ, Rauch SL, Savage CR, O’Sullivan RL, et al. Phenomenological differences appearing with repetitive behaviours in obsessive-compulsive disorder and Gilles de la Tourette’s syndrome. Br J Psychiatry. 1997;170:140–5.
do Rosario-Campos MC, Leckman JF, Mercadante MT, Shavitt RG, Prado HDS, Sada P, et al. Adults with early-onset obsessive-compulsive disorder. Am J Psychiatry. 2001;158:1899–903.
Shavitt RG, Belotto C, Curi M, Hounie AG, Rosário-Campos MC, Diniz JB, et al. Clinical features associated with treatment response in obsessive-compulsive disorder. Compr Psychiatry. 2006;47:276–81.
Lochner C, Hemmings SM, Kinnear CJ, Niehaus DJ, Nel DG, Corfield VA, et al. Cluster analysis of obsessive-compulsive spectrum disorders in patients with obsessive-compulsive disorder: clinical and genetic correlates. Compr Psychiatry. 2005;46:14–9.
Pauls DL, Abramovitch A, Rauch SL, Geller DA. Obsessive–compulsive disorder: an integrative genetic and neurobiological perspective. Nat Rev Neurosci. 2014;15:410–24.
Mataix-Cols D, van den Heuvel OA. Common and distinct neural correlates of obsessive-compulsive and related disorders. Psychiatr Clin. 2006;29:391–410.
Figee M, Luigies J, Goudriaan A, Willuhn I, Denys D. Neurocognitive basis of compulsivity. In: Fontenelle L, Yücel M, editors. A transdiagnostic approach to obsessions, compulsions and related phenomena. Cambridge, UK: Cambridge University Press; 2019. p. 61–73.
Kohn N, Eickhoff SB, Scheller M, Laird AR, Fox PT, Habel U. Neural network of cognitive emotion regulation - an ALE meta-analysis and MACM analysis. Neuroimage. 2014;87:345–55.
Thorsen AL, Hagland P, Radua J, Mataix-Cols D, Kvale G, Hansen B, et al. Emotional processing in obsessive-compulsive disorder: a systematic review and meta-analysis of 25 functional neuroimaging studies. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018;3:563–71.
Milad MR, Furtak SC, Greenberg JL, Keshaviah A, Im JJ, Falkenstein MJ, et al. Deficits in conditioned fear extinction in obsessive-compulsive disorder and neurobiological changes in the fear circuit. JAMA Psychiatry. 2013;70:608–18.
Van Schalkwyk GI, Bhalla IP, Griepp M, Kelmendi B, Davidson L, Pittenger C. Toward understanding the heterogeneity in obsessive-compulsive disorder: Evidence from narratives in adult patients. Aust NZ J Psychiatry. 2016;50:74–81.
Paul S, Beucke JC, Kaufmann C, Mersov A, Heinzel S, Kathmann N, et al. Amygdala–prefrontal connectivity during appraisal of symptom-related stimuli in obsessive–compulsive disorder. Psychol Med. 2019;49:278–86.
Apergis-Schoute AM, Gillan CM, Fineberg NA, Fernandez-Egea E, Sahakian BJ, Robbins TW. Neural basis of impaired safety signaling in obsessive compulsive disorder. PNAS. 2017;114:3216–21.
McLaughlin NC, Strong D, Abrantes A, Garnaat S, Cerny A, O’Connell C, et al. Extinction retention and fear renewal in a lifetime obsessive–compulsive disorder sample. Behav Brain Res. 2015;280:72–7.
Fyer AJ, Schneier FR, Simpson HB, Choo TH, Tacopina S, Kimeldorf MB, et al. Heterogeneity in fear processing across and within anxiety, eating, and compulsive disorders. J Affect Disord. 2020;271:329–38.
Jacoby RJ, Abramowitz JS. Intolerance of uncertainty in OCD. Obsessive-Compuls Disord: Phenomenol, Pathophysiol, Treat. 2017;12:171.
Kobori O, Salkovskis PM, Read J, Lounes N, Wong V. A qualitative study of the investigation of reassurance seeking in obsessive–compulsive disorder. J Obsessive-Compuls Relat Disord. 2012;1:25–32.
Gentes EL, Ruscio AM. A meta-analysis of the relation of intolerance of uncertainty to symptoms of generalized anxiety disorder, major depressive disorder, and obsessive-compulsive disorder. Clin Psychol Rev. 2011;31:923–33.
Weidt S, Lutz J, Rufer M, Delsignore A, Jakob NJ, Herwig U, et al. Common and differential alterations of general emotion processing in obsessive-compulsive and social anxiety disorder. Psychol Med. 2016;46:1427–36.
Stern ER, Welsh RC, Gonzalez R, Fitzgerald KD, Abelson JL, Taylor SF. Subjective uncertainty and limbic hyperactivation in obsessive‐compulsive disorder. Hum Brain Mapp. 2013;34:1956–70.
Morriss J, Christakou A, van Reekum CM. Intolerance of uncertainty predicts fear extinction in amygdala-ventromedial prefrontal cortical circuitry. Biol Mood Anxiety Disord. 2015;5:4.
Sescousse G, Caldú X, Segura B, Dreher JC. Processing of primary and secondary rewards: a quantitative meta-analysis and review of human functional neuroimaging studies. Neurosci Biobehav Rev. 2013;37:681–96.
Hirschtritt ME, Bloch MH, Mathews CA. Obsessive-Compulsive Disorder: Advances in Diagnosis and Treatment. JAMA. 2017;317:1358–67.
Buhle JT, Silvers AJ, Wager TD, Lopez R, Onyemekwu C, Kober H. Cognitive Reappraisal of Emotion: A meta-analysis of human neuroimaging studies. Cereb Cortex. 2014;24:2981–90.
Olatunji BO, Ferreira-Garcia R, Caseras X, Fullana MA, Wooderson S, Speckens A, et al. Predicting response to cognitive behavioral therapy in contamination-based obsessive–compulsive disorder from functional magnetic resonance imaging. Psychol Med. 2014;44:2125–37.
Fullana MA, Zhu X, Alonso P, Cardoner N, Real E, López-Solà C, et al. Basolateral amygdala–ventromedial prefrontal cortex connectivity predicts cognitive behavioural therapy outcome in adults with obsessive–compulsive disorder. J Psychiatry Neurosci. 2017;42:378.
Belloch A, Cabedo E, Carrió C, Fernández-Alvarez H, García F, Larsson C. Group versus individual cognitive treatment for obsessive-compulsive disorder: changes in non-OCD symptoms and cognitions at post-treatment and one-year follow-up. Psychiatry Res. 2011;187:174–9.
Overton SM, Menzies RG. Cognitive change during treatment of compulsive checking. Behav Change. 2005;22:172–84.
Arce E, Simmons AN, Lovero KL, Stein MB, Paulus MP. Escitalopram effects on insula and amygdala BOLD activation during emotional processing. Psychopharmacology. 2008;196:661–72.
Selvaraj S, Walker C, Arnone D, Cao B, Faulkner P, Cowen PJ, et al. Effect of citalopram on emotion processing in humans: a combined 5-HT 1A [11 C] CUMI-101 PET and functional MRI study. Neuropsychopharmacology. 2018;43:655–64.
Kim M, Kwak S, Yoon YB, Kwak YB, Kim T, Cho KI, et al. Functional connectivity of the raphe nucleus as a predictor of the response to selective serotonin reuptake inhibitors in obsessive-compulsive disorder. Neuropsychopharmacology. 2019;44:2073–81.
Nitschke JB, Sarinopoulos I, Oathes DJ, Johnstone T, Whalen PJ, Davidson RJ, et al. Anticipatory activation in the amygdala and anterior cingulate in generalized anxiety disorder and prediction of treatment response. Am J Psychiatry. 2009;166:302–10.
De Wit SJ, Van der Werf YD, Mataix-Cols D, Trujillo JP, Van Oppen P, Veltman DJ, et al. Emotion regulation before and after transcranial magnetic stimulation in obsessive compulsive disorder. Psychological Med. 2015;45:3059–73.
Assaf M, Rabany L, Zertuche L, Bragdon L, Tolin D, Goethe J, et al. Neural functional architecture and modulation during decision making under uncertainty in individuals with generalized anxiety disorder. Brain Behav. 2018;8:e01015.
Rehn S, Eslick GD, Brakoulias V. A meta-analysis of the effectiveness of different cortical targets used in repetitive transcranial magnetic stimulation (rTMS) for the treatment of obsessive-compulsive disorder (OCD). Psychiatr Q. 2018;89:645–65.
Carmi L, Tendler A, Bystritsky A, Hollander E, Blumberger DM, Daskalakis J, et al. Efficacy and safety of deep transcranial magnetic stimulation for obsessive-compulsive disorder: a prospective multicenter randomized double-blind placebo-controlled trial. Am J Psychiatry. 2019;176:931–8.
Scheinost D, Stoica T, Saksa J, Papademetris X, Constable RT, Pittenger C, et al. Orbitofrontal cortex neurofeedback produces lasting changes in contamination anxiety and resting-state connectivity. Transl Psychiatry. 2013;3:e250.
Scheinost D, Stoica T, Wasylink S, Gruner P, Saksa J, Pittenger C, et al. Resting state functional connectivity predicts neurofeedback response. Front Behav Neurosci. 2014;8:338.
Paret C, Ruf M, Gerchen MF, Kluetsch R, Demirakca T, Jungkuntz M, et al. fMRI neurofeedback of amygdala response to aversive stimuli enhances prefrontal–limbic brain connectivity. Neuroimage. 2016;125:182–8.
Fridgeirsson EA, Figee M, Luigjes J, van den Munckhof P, Schuurman PR, van Wingen G, et al. Deep brain stimulation modulates directional limbic connectivity in obsessive-compulsive disorder. Brain. 2020;143:1603–12.
LeDoux JE, Pine DS. Using neuroscience to help understand fear and anxiety: a two-system framework. Am J Psychiatry. 2016;173:1083–93.
Luyten L, Hendrickx S, Raymaekers S, Gabriëls L, Nuttin B. Electrical stimulation in the bed nucleus of the stria terminalis alleviates severe obsessive-compulsive disorder. Mol Psychiatry. 2016;21:1272–80.
Li N, Baldermann JC, Kibleur A, Treu S, Akram H, Elias GJ, et al. A unified connectomic target for deep brain stimulation in obsessive-compulsive disorder. Nat Commun. 2020;11:1–2.
Liebrand LC, Caan MW, Schuurman PR, van den Munckhof P, Figee M, Denys D, et al. Individual white matter bundle trajectories are associated with deep brain stimulation response in obsessive-compulsive disorder. Brain Stimul. 2019;12:353–60.
Kurth F, Zilles K, Fox PT, Laird AR, Eickhoff SB. A link between the systems: functional differentiation and integration within the human insula revealed by meta-analysis. Brain Struct Funct. 2010;214:519–34.
Ferrão YA, Shavitt RG, Prado H, Fontenelle LF, Malavazzi DM, de Mathis MA, et al. Sensory phenomena associated with repetitive behaviors in obsessive-compulsive disorder: an exploratory study of 1001 patients. Psychiatry Res. 2012;197:253–8.
Lee JC, Prado HS, Diniz JB, Borcato S, da Silva CB, Hounie AG, et al. Perfectionism and sensory phenomena: phenotypic components of obsessive-compulsive disorder. Compr Psychiatry. 2009;50:431–6.
Rosario MC, Prado HS, Borcato S, Diniz JB, Shavitt RG, Hounie AG. Validation of the University of São Paulo Sensory Phenomena Scale: initial psychometric properties. CNS Spectr. 2009;14:315–23.
Shavitt RG, de Mathis MA, Oki F, Ferrao YA, Fontenelle LF, Torres AR, et al. Phenomenology of OCD: lessons from a large multicenter study and implications for ICD-11. J Psychiatr Res. 2014;57:141–8.
Summerfeldt LJ, Kloosterman PH, Antony MM, Swinson RP. Examining an obsessive-compulsive core dimensions model: Structural validity of harm avoidance and incompleteness. JOCRD. 2014;3:83–94.
Coughtrey AE, Shafran R, Lee M, Rachman SJ. It’s the feeling inside my head: a qualitative analysis of mental contamination in obsessive-compulsive disorder. Behavioural Cogn Psychother. 2012;40:163–73.
Reese HE, Scahill L, Peterson AL, Crowe K, Woods DW, Piacentini J, et al. The premonitory urge to tic: measurement, characteristics, and correlates in older adolescents and adults. Behav Ther. 2014;45:177–86.
Berman BD, Horovitz SG, Morel B, Hallett M. Neural correlates of blink suppression and the buildup of a natural bodily urge. Neuroimage. 2012;59:1441–50.
Jackson SR, Parkinson A, Kim SY, Schüermann M, Eickhoff SB. On the functional anatomy of the urge-for-action. Cogn Neurosci. 2011;2:227–43.
Mazzone SB, Cole LJ, Ando A, Egan GF, Farrell MJ, et al. Investigation of the neural control of cough and cough suppression in humans using functional brain imaging. J Neurosci. 2011;31:2948–58.
Bohlhalter S, Goldfine A, Matteson S, Garraux G, Hanakawa T, Kansaku K, et al. Neural correlates of tic generation in Tourette syndrome: an event-related functional MRI study. Brain. 2006;129:2029–37.
Neuner I, Werner CJ, Arrubla J, Stöcker T, Ehlen C, Wegener HP, et al. Imaging the where and when of tic generation and resting state networks in adult Tourette patients. Front Hum Neurosci. 2014;8:362.
Stern ER, Brown C, Ludlow M, Shahab R, Collins K, Lieval A, et al. The buildup of an urge in obsessive–compulsive disorder: Behavioral and neuroimaging correlates. Hum Brain Mapp. 2020;41:1611–25.
Subirà M, Sato JR, Alonso P, do Rosário MC, Segalàs C, Batistuzzo MC, et al. Brain structural correlates of sensory phenomena in patients with obsessive–compulsive disorder. J Psychiatry Neurosci. 2015;40:232–40.
Brown C, Shahab R, Collins K, Fleysher L, Goodman WK, Burdick KE, et al. Functional neural mechanisms of sensory phenomena in obsessive-compulsive disorder. J Psychiatr Res. 2019;109:68–75.
Tricomi E, Balleine BW, O’Doherty JP. A specific role for posterior dorsolateral striatum in human habit learning. Eur J Neurosci. 2009;29:2225–32.
De Wit S, Watson P, Harsay HA, Cohen MX, van de Vijver I, Ridderinkhof KR. Corticostriatal connectivity underlies individual differences in the balance between habitual and goal-directed action control. J Neurosci. 2012;32:12066–75.
Gillan CM, Robbins TW. Goal-directed learning and obsessive-compulsive disorder. Philos Trans R Soc Lond B Biol Sci. 2014;369:20130475.
Gillan CM, Apergis-Schoute AM, Morein-Zamir S, Urcelay GP, Sule A, Fineberg NA, et al. Functional neuroimaging of avoidance habits in obsessive-compulsive disorder. Am J Psychiatry. 2015;172:284–93.
Delorme C, Salvador A, Valabregue R, Roze E, Palminteri S, Vidailhet M, et al. Enhanced habit formation in Gilles de la Tourette syndrome. Brain. 2016;139:605–15.
Gillan CM, Kosinski M, Whelan R, Phelps EA, Daw ND. Characterizing a psychiatric symptom dimension related to deficits in goal-directed control. Elife. 2016;5:e11305.
Yin HH, Knowlton BJ. The role of the basal ganglia in habit formation. Nat Rev Neurosci. 2006;7:464–76.
Prado HS, Rosário MC, Lee J, Hounie AG, Shavitt RG, Miguel EC. Sensory phenomena in obsessive-compulsive disorder and tic disorders: a review of the literature. CNS Spectr. 2008;13:425–32.
Cavanna AE, Black KJ, Hallett M, Voon V. Neurobiology of the premonitory urge in Tourette’s syndrome: pathophysiology and treatment implications. J Neuropsychiatry Clin Neurosci. 2017;29:95–104.
Mathes BM, Kennedy GA, Wilver NL, Carlton CN, Cougle JR. A multi-method analysis of incompleteness in behavioral treatment of contamination-based OCD. Behav Res Ther. 2019;114:1–6.
Houghton DC, Capriotti MR, Scahill LD, Wilhelm S, Peterson AL, Walkup JT, et al. Investigating habituation to premonitory urges in behavior therapy for tic disorders. Behav Ther. 2017;48:834–46.
McGuire JF, Piacentini J, Brennan EA, Lewin AB, Murphy TK, Small BJ, et al. A meta-analysis of behavior therapy for Tourette syndrome. J Psychiatr Res. 2014;50:106–12.
Deckersbach T, Chou T, Britton JC, Carlson LE, Reese HE, Siev J, et al. Neural correlates of behavior therapy for Tourette׳ s disorder. Psychiatry Res: Neuroimaging. 2014;224:269–74.
Van de Griendt JM, Verdellen CW, Van Dijk MK, Verbraak MJ. Behavioural treatment of tics: habit reversal and exposure with response prevention. Neurosci Biobehav Rev. 2013;37:1172–7.
Dillenburger K. Habit reversal training as a treatment for refractory OCD–A case study. Eur J Behav Anal. 2006;7:67–75.
Chau DT, Fogelman P, Nordanskog P, Drevets WC, Hamilton JP. Distinct neural-functional effects of treatments with selective serotonin reuptake inhibitors, electroconvulsive therapy, and transcranial magnetic stimulation and their relations to regional brain function in major depression: a meta-analysis. Biol Psychiatry: Cogn Neurosci Neuroimaging. 2017;2:318–26.
Ye JH, Ponnudurai R, Schaefer R. Ondansetron: a selective 5-HT(3) receptor antagonist and its applications in CNS-related disorders. CNS Drug Rev. 2001;7:199–213.
Stern ER, Shahab R, Grimaldi SJ, Leibu E, Murrough JW, Fleysher L. High-dose ondansetron reduces activation of interoceptive and sensorimotor brain regions. Neuropsychopharmacology. 2019;44:390–8.
Heidari M, Zarei M, Hosseini SM, Taghvaei R, Maleki H, Tabrizi M. Ondansetron or placebo in the augmentation of fluvoxamine response over 8 weeks in obsessive-compulsive disorder. Int Clin Psychopharmacol. 2014;29:344–50.
Pallanti S, Bernardi S, Antonini S, Singh N, Hollander E. Ondansetron augmentation in patients with obsessive-compulsive disorder who are inadequate responders to serotonin reuptake inhibitors: improvement with treatment and worsening following discontinuation. Eur Neuropsychopharmacol. 2014;24:375–80.
Toren P, Weizman A, Ratner S, Cohen D, Laor N. Ondansetron treatment in Tourette’s disorder: a 3-week, randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2005;66:499–503.
Transcept Pharmaceuticals I. Transcept pharmaceuticals announces that a phase 2 clinical trial of TO-2061 as adjunctive therapy for obsessive compulsive disorder did not meet primary endpoint. 2012. http://ir.transcept.com/releasedetail.cfm?ReleaseID=728327. Accessed 4 Oct 2014.
Mantovani A, Simpson HB, Fallon BA, Rossi S, Lisanby SH. Randomized sham-controlled trial of repetitive transcranial magnetic stimulation in treatment-resistant obsessive-compulsive disorder. Int J Neuropsychopharmacol. 2010;13:217–27.
Le K, Liu L, Sun M, Hu L, Xiao N. Transcranial magnetic stimulation at 1 Hertz improves clinical symptoms in children with Tourette syndrome for at least 6 months. J Clin Neurosci. 2013;20:257–62.
Landeros-Weisenberger A, Mantovani A, Motlagh MG, de Alvarenga PG, Katsovich L, Leckman JF, et al. Randomized sham controlled double-blind trial of repetitive transcranial magnetic stimulation for adults with severe Tourette syndrome. Brain Stimul. 2015;8:574–81.
Senço NM, Huang Y, D’Urso G, Parra LC, Bikson M, Mantovani A, et al. Transcranial direct current stimulation in obsessive–compulsive disorder: emerging clinical evidence and considerations for optimal montage of electrodes. Expert Rev Med Devices. 2015;12:381–91.
D’Urso G, Brunoni AR, Mazzaferro MP, Anastasia A, de Bartolomeis A, Mantovani A. Transcranial direct current stimulation for obsessive-compulsive disorder: a randomized, controlled, partial crossover trial. Depress Anxiety. 2016;33:1132–40.
Deng ZD, Lisanby SH, Peterchev AV. Coil design considerations for deep transcranial magnetic stimulation. Clin Neurophysiol. 2014;125:1202–12.
Zibman S, Pell GS, Barnea-Ygael N, Roth Y, Zangen A. Application of transcranial magnetic stimulation for major depression: coil design and neuroanatomical variability considerations. Eur Neuropsychopharmacol. 2019. In Press.
Malik S, Jacobs M, Cho SS, Boileau I, Blumberger D, Heilig M, et al. Deep TMS of the insula using the H-coil modulates dopamine release: a crossover [11 C] PHNO-PET pilot trial in healthy humans. Brain Imaging Behav. 2018;12:1306–17.
Dinur-Klein L, Dannon P, Hadar A, Rosenberg O, Roth Y, Kotler M, et al. Smoking cessation induced by deep repetitive transcranial magnetic stimulation of the prefrontal and insular cortices: a prospective, randomized controlled trial. Biol Psychiatry. 2014;76:742–9.
Aron AR, Robbins TW, Poldrack RA. Inhibition and the right inferior frontal cortex: one decade on. Trends Cogn Sci. 2014;18:177–85.
Swick D, Ashley V, Turken U. Are the neural correlates of stopping and not going identical? Quantitative meta-analysis of two response inhibition tasks. Neuroimage. 2011;56:1655–65.
Abramovitch A, Abramowitz JS, Mittelman A. The neuropsychology of adult obsessive–compulsive disorder: a meta-analysis. Clin Psychol Rev. 2013;33:1163–71.
De Wit SJ, de Vries FE, van der Werf YD, Cath DC, Heslenfeld DJ, Veltman EM, et al. Presupplementary motor area hyperactivity during response inhibition: a candidate endophenotype of obsessive-compulsive disorder. Am J Psychiatry. 2012;169:1100–8.
Kang DH, Jang JH, Han JY, Kim JH, Jung WH, Choi JS, et al. Neural correlates of altered response inhibition and dysfunctional connectivity at rest in obsessive–compulsive disorder. Prog Neuro-Psychopharmacol Biol Psychiatry. 2013;40:340–6.
Rasmussen J, Siev J, Abramovitch A, Wilhelm S. Scrupulosity and contamination OCD are not associated with deficits in response inhibition. J Behav Ther Exp Psychiatry. 2016;50:120–6.
Silveira VP, Frydman I, Fontenelle LF, Mattos P, de Oliveira-Souza R, Moll J, et al. Exploring response inhibition and error monitoring in obsessive-compulsive disorder. J Psychiatr Res. 2020;126:26–33.
Kalanthroff E, Teichert T, Wheaton MG, Kimeldorf MB, Linkovski O, Ahmari SE, et al. The role of response inhibition in medicated and unmedicated obsessive‐compulsive disorder patients: evidence from the stop‐signal task. Depression Anxiety. 2017;34:301–306.
Leopold R, Backenstrass M. Neuropsychological differences between obsessive-compulsive washers and checkers: a systematic review and meta-analysis. J Anxiety Disord. 2015;30:48–58.
van Wijk BC, Alkemade A, Forstmann BU. Functional segregation and integration within the human subthalamic nucleus from a micro-and meso-level perspective. Cortex. 2020;131:103–13.
Rottschy C, Langner R, Dogan I, Reetz K, Laird AR, Schulz JB, et al. Modelling neural correlates of working memory: a coordinate-based meta-analysis. Neuroimage. 2012;60:830–46.
Rappel P, Marmor O, Bick AS, Arkadir D, Linetsky E, Castrioto A, et al. Subthalamic theta activity: a novel human subcortical biomarker for obsessive compulsive disorder. Transl Psychiatry. 2018;8:1–11.
Cavanagh JF, Frank MJ. Frontal theta as a mechanism for cognitive control. Trends Cogn Sci. 2014;18:414–21.
Widge AS, Zorowitz S, Basu I, Paulk AC, Cash SS, Eskandar EN, et al. Deep brain stimulation of the internal capsule enhances human cognitive control and prefrontal cortex function. Nat Commun. 2019;10:1.
Alegria AA, Wulff M, Brinson H, Barker GJ, Norman LJ, Brandeis D, et al. Real‐time fMRI neurofeedback in adolescents with attention deficit hyperactivity disorder. Hum Brain Mapp. 2017;38:3190–209.
Rubia K, Criaud M, Wulff M, Alegria A, Brinson H, Barker G, et al. Functional connectivity changes associated with fMRI neurofeedback of right inferior frontal cortex in adolescents with ADHD. NeuroImage. 2019;188:43–58.
Haber SN, Knutson B. The reward circuit: linking primate anatomy and human imaging. Neuropsychopharmacology. 2010;35:4–26.
Figee M, Vink M, de Geus F, Vulink N, Veltman DJ, Westenberg H, et al. Dysfunctional reward circuitry in obsessive-compulsive disorder. Biol Psychiatry. 2011;69:867–74.
Kaufmann C, Beucke JC, Preuße F, Endrass T, Schlagenhauf F, Heinz A, et al. Medial prefrontal brain activation to anticipated reward and loss in obsessive–compulsive disorder. Neuroimage Clin. 2013;2:212–20.
Abramovitch A, Pizzagalli DA, Reuman L, Wilhelm S. Anhedonia in obsessive-compulsive disorder: beyond comorbid depression. Psychiatry Res. 2014;216:223–9.
Pushkarskaya H, Sobowale K, Henick D, Tolin DF, Anticevic A, Pearlson GD, et al. Contrasting contributions of anhedonia to obsessive-compulsive, hoarding, and post-traumatic stress disorders. J Psychiatr Res. 2019;109:202–13.
Xie C, Ma L, Jiang N, Huang R, Li L, Gong L, et al. Imbalanced functional link between reward circuits and the cognitive control system in patients with obsessive-compulsive disorder. Brain Imaging Behav. 2017;11:1099–109.
Jung WH, Kang D-H, Kim E, Shin KS, Jang JH, Kwon JS. Abnormal corticostriatal-limbic functional connectivity in obsessive–compulsive disorder during reward processing and resting-state. Neuroimage Clin. 2013;3:27–38.
Koch K, Reeß TJ, Rus OG, Gürsel DA, Wagner G, Berberich G, et al. Increased default mode network connectivity in obsessive–compulsive disorder during reward processing. Front Psychiatry. 2018;9:254.
Admon R, Bleich-Cohen M, Weizmant R, Poyurovsky M, Faragian S, Hendler T. Functional and structural neural indices of risk aversion in obsessive–compulsive disorder (OCD). Psychiatry Res: Neuroimaging. 2012;203:207–13.
Norman LJ, Carlisi CO, Christakou A, Murphy CM, Chantiluke K, Giampietro V, et al. Frontostriatal dysfunction during decision making in attention-deficit/hyperactivity disorder and obsessive-compulsive disorder. Biol Psychiatry: Cogn Neurosci Neuroimaging. 2018;3:694–703.
Moreira PS, Macoveanu J, Marques P, Coelho A, Magalhaes R, Siebner HR, et al. Altered response to risky decisions and reward in patients with obsessive-compulsive disorder. J Psychiatry Neurosci. 2020;45:98–108.
Grassi G, Pallanti S, Righi L, Figee M, Mantione M, Denys D, et al. Think twice: impulsivity and decision making in obsessive–compulsive disorder. J Behav Addict. 2015;4:263–72.
Grassi G, Makris N, Pallanti S. Addicted to compulsion: assessing three core dimensions of addiction across obsessive-compulsive disorder and gambling disorder. CNS Spectr. 2019;20:392–401.
Rouhani N, Wimmer GE, Schneier FR, Fyer AJ, Shohamy D, Simpson HB. Impaired generalization of reward but not loss in obsessive–compulsive disorder. Depression Anxiety. 2019;36:121–9.
Voon V, Baek K, Enander J, Worbe Y, Morris LS, Harrison NA, et al. Motivation and value influences in the relative balance of goal-directed and habitual behaviours in obsessive-compulsive disorder. Transl Psychiatry. 2015;5:e670.
Sip KE, Gonzalez R, Taylor SF, Stern ER. Increased loss aversion in unmedicated patients with obsessive–compulsive disorder. Front Psychiatry. 2018;8:309.
Jung WH, Kang DH, Han JY, Jang JH, Gu BM, Choi JS, et al. Aberrant ventral striatal responses during incentive processing in unmedicated patients with obsessive–compulsive disorder. Acta Psychiatr Scandinavica. 2011;123:376–86.
Choi JS, Shin YC, Jung WH, Jang JH, Kang DH, Choi CH, et al. Altered brain activity during reward anticipation in pathological gambling and obsessive-compulsive disorder. PLoS ONE. 2012;7:e45938.
Hauser TU, Iannaccone R, Dolan RJ, Ball J, Hättenschwiler J, Drechsler R, et al. Increased fronto-striatal reward prediction errors moderate decision making in obsessive–compulsive disorder. Psychological Med. 2017;47:1246–58.
Phan KL, Fitzgerald DA, Nathan PJ, Moore GJ, Uhde TW, Tancer ME. Neural substrates for voluntary suppression of negative affect: a functional magnetic resonance imaging study. Biol Psychiatry. 2005;57:210–9.
Murray GK, Knolle F, Ersche KD, Craig KJ, Abbott S, Shabbir SS, et al. Dopaminergic drug treatment remediates exaggerated cingulate prediction error responses in obsessive-compulsive disorder. Psychopharmacology. 2019;236:2325–36.
Palminteri S, Clair A-H, Mallet L, Pessiglione M. Similar improvement of reward and punishment learning by serotonin reuptake inhibitors in obsessive-compulsive disorder. Biol Psychiatry. 2012;72:244–50.
Kranz GS, Kasper S, Lanzenberger R. Reward and the serotonergic system. Neuroscience. 2010;166:1023–35.
Rubia K, Halari R, Cubillo A, Mohammad AM, Brammer M, Taylor E. Methylphenidate normalises activation and functional connectivity deficits in attention and motivation networks in medication-naive children with ADHD during a rewarded continuous performance task. Neuropharmacology. 2009;57:640–52.
Figee M, Luigjes J, Smolders R, Valencia-Alfonso CD, van Wingen G, de Kwaasteniet B, et al. Deep brain stimulation restores frontostriatal network activity in obsessive-compulsive disorder. Nat Neurosci. 2013;16:386–7.
Coenen VA, Schlaepfer TE, Goll P, Reinacher PC, Voderholzer U, Tebartz van Elst L, et al. The medial forebrain bundle as a target for deep brain stimulation for obsessive-compulsive disorder. CNS Spectr. 2017;22:282–9.
Greer SM, Trujillo AJ, Glover GH, Knutson B. Control of nucleus accumbens activity with neurofeedback. Neuroimage. 2014;96:237–44.
Marek S, Dosenbach NU. The frontoparietal network: function, electrophysiology, and importance of individual precision mapping. Dialogues Clin Neurosci. 2018;20:133.
Vossel S, Geng JJ, Fink GR. Dorsal and ventral attention systems: distinct neural circuits but collaborative roles. Neuroscientist. 2014;20:150–9.
Snyder HR, Kaiser RH, Warren SL, Heller W. Obsessive-compulsive disorder is associated with broad impairments in executive function: a meta-analysis. Clin Psychological Sci. 2015;3:301–30.
Vaghi MM, Vértes PE, Kitzbichler MG, Apergis-Schoute AM, van der Flier FE, Fineberg NA, et al. Specific frontostriatal circuits for impaired cognitive flexibility and goal-directed planning in obsessive-compulsive disorder: evidence from resting-state functional connectivity. Biol Psychiatry. 2017;81:708–17.
Olson CA, Hale LR, Hamilton N, Powell JN, Martin LE, Savage CR. Altered source memory retrieval is associated with pathological doubt in obsessive–compulsive disorder. Behavioural Brain Res. 2016;296:53–60.
Jaafari N, Frasca M, Rigalleau F, Rachid F, Gil R, Olié JP, et al. Forgetting what you have checked: a link between working memory impairment and checking behaviors in obsessive-compulsive disorder. Eur Psychiatry. 2013;28:87–93.
Buhlmann U, Deckersbach T, Engelhard I, Cook LM, Rauch SL, Kathmann N, et al. Cognitive retraining for organizational impairment in obsessive-compulsive disorder. Psychiatry Res. 2006;144:109–16.
Park HS, Shin YW, Ha TH, Shin MS, Kim YY, Lee YH, et al. Effect of cognitive training focusing on organizational strategies in patients with obsessive‐compulsive disorder. Psychiatry Clin Neurosci. 2006;60:718–26.
Kashyap H, Reddy P, Mandadi S, Narayanaswamy JC, Sudhir PM, Reddy YJ. Cognitive training for neurocognitive and functional impairments in obsessive compulsive disorder: a case report. J Obsessive-Compuls Relat Disord. 2019;23:100480.
Kalanthroff E, Steinman SA, Schmidt AB, Campeas R, Simpson HB. Piloting a personalized computerized inhibitory training program for individuals with obsessive-compulsive disorder. Psychother Psychosom. 2018;87:52–5.
Zheng H, Jia F, Han H, Wang S, Guo G, Quan D. Combined fluvoxamine and extended-release methylphenidate improved treatment response compared to fluvoxamine alone in patients with treatment-refractory obsessive-compulsive disorder: a randomized double-blind, placebo-controlled study. Eur Neuropsychopharmacol. 2019;29:397–404.
Faraone SV. The pharmacology of amphetamine and methylphenidate: relevance to the neurobiology of attention-deficit/hyperactivity disorder and other psychiatric comorbidities. Neurosci Biobehav Rev. 2018;87:255–70.
Woolley JB, Heyman I. Dexamphetamine for obsessive-compulsive disorder. Am J Psychiatry. 2003;160:183.
Bloch M, Landeros-Weisenberger A, Kelmendi B, Coric V, Bracken MB, Leckman JF. A systematic review: antipsychotic augmentation with treatment refractory obsessive-compulsive disorder. Mol Psychiatry. 2006;11:622–32.
Cools R, D’Esposito M. Inverted-U–shaped dopamine actions on human working memory and cognitive control. Biol Psychiatry. 2011;69:e113–25.
Zhou DD, Wang W, Wang GM, Li DQ, Kuang L. An updated meta-analysis: short-term therapeutic effects of repeated transcranial magnetic stimulation in treating obsessive-compulsive disorder. J Affect Disord. 2017;215:187–96.
D’Urso G, Brunoni AR, Mazzaferro MP, Anastasia A, de Bartolomeis A, Mantovani A. Transcranial direct current stimulation for obsessive–compulsive disorder: a randomized, controlled, partial crossover trial. Depression Anxiety. 2016;33:1132–40.
Gowda SM, Narayanaswamy JC, Hazari N, Bose A, Chhabra H, Balachander S, et al. Efficacy of pre-supplementary motor area transcranial direct current stimulation for treatment resistant obsessive compulsive disorder: a randomized, double blinded, sham controlled trial. Brain Stimul. 2019;12:922–9.
Choi EY, Tanimura Y, Vage PR, Yates EH, Haber SN. Convergence of prefrontal and parietal anatomical projections in a connectional hub in the striatum. Neuroimage. 2017;146:821–32.
Picó-Pérez M, Radua J, Steward T, Menchón JM, Soriano-Mas C. Emotion regulation in mood and anxiety disorders: a meta-analysis of fMRI cognitive reappraisal studies. Prog Neuropsychopharmacol Biol Psychiatry. 2017;79:96–104.
Picó-Pérez M, Alemany-Navarro M, Dunsmoor JE, Radua J, Albajes-Eizagirre A, Vervliet B, et al. Common and distinct neural correlates of fear extinction and cognitive reappraisal: a meta-analysis of fMRI studies. Neurosci Biobehav Rev. 2019;104:102–15.
Tang W, Jbabdi S, Zhu Z, Cottaar M, Grisot G, Lehman JF, et al. A connectional hub in the rostral anterior cingulate cortex links areas of emotion and cognitive control. Elife. 2019;8:e43761.
Haber SN, Tang W, Choi EY, Yendiki A, Liu H, Jbabdi S, et al. Circuits, networks, and neuropsychiatric disease: transitioning from anatomy to imaging. Biol Psychiatry. 2020;87:318–27.
van den Heuvel OA, Boedhoe P, Bertolin S, Bruin WB, Francks C, Ivanov I, et al. An overview of the first 5 years of the ENIGMA obsessive–compulsive disorder working group: the power of worldwide collaboration. Hum Brain Mapp. 2020. https://doi.org/10.1002/hbm.24972.
Boedhoe P, Schmaal L, Abe Y, Alonso P, Ameis SH, Anticevic A, et al. Cortical abnormalities associated with pediatric and adult obsessive-compulsive disorder: findings from the ENIGMA Obsessive-Compulsive Disorder Working Group. Am J Psychiatry. 2018;175:453–62.
Stern ER, Fitzgerald KD, Welsh RC, Abelson JL, Taylor SF. Resting-state functional connectivity between fronto-parietal and default mode networks in obsessive-compulsive disorder. PloS ONE. 2012;7:e36356.
Scolari M, Seidl-Rathkopf KN, Kastner S. Functions of the human frontoparietal attention network: evidence from neuroimaging. Curr Opin Behav Sci. 2015;1:32–9.
Sheffield JM, Repovs G, Harms MP, Carter CS, Gold JM, MacDonald AW III, et al. Fronto-parietal and cingulo-opercular network integrity and cognition in health and schizophrenia. Neuropsychologia. 2015;73:82–93.
Bikson M, Brunoni AR, Charvet LE, Clark VP, Cohen LG, Deng ZD, et al. Rigor and reproducibility in research with transcranial electrical stimulation: an NIMH-sponsored workshop. Brain Stimul. 2018;11:465–80.
Stein DJ. An integrative approach to psychiatric diagnosis and research. World Psychiatry. 2014;13:51.
Dougherty DD. Will deep brain stimulation help move precision medicine to the clinic in psychiatry? Biol Psychiatry. 2019;85:706–7.
Freeston MH, Rhéaume J, Letarte H, Dugas MJ, Ladouceur R. Why do people worry? Pers Individ Diff. 1994;17:791–802.
Coles ME, Heimberg RG, Frost RO, Steketee G. Not just right experiences and obsessive-compulsive features: experimental and self-monitoring perspectives. Behav Res Ther. 2005;43:153–67.
Brunoni AR, Sampaio-Junior B, Moffa AH, Aparício LV, Gordon P, Klein I, et al. Noninvasive brain stimulation in psychiatric disorders: a primer. Braz J Psychiatry. 2019;41:70–81.
Acknowledgements
We are very grateful to the patients who shared experiences of their symptoms and agreed for these to be included in this article. This work was supported by a postdoctoral fellowship awarded to ES from the São Paulo Research Foundation (18/22396-7) and research grants from the São Paulo Research Foundation (2014/50917-0) and CNPq (465550/2014-2) awarded to ECM as part of the National Institute of Developmental Psychiatry for Children and Adolescents (INDP).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
RGS has received consulting honoraria from Lundbeck and a travel grant from LIBBS. ARB has received funding from the São Paulo Research Foundation (2017/50223-6, 2018/10861-7), the Brazilian National Council of Scientific Development productivity support (PQ-1B), and the University of São Paulo Medical School productivity support (PIPA-A), and is the Chief Medical Advisor of Flow Neuroscience (Malmö, Sweden) and has a small equity in this company. JR Y.C. has received support from the various Government of India funding agencies for research on OCD, including the Department of Biotechnology (DBT), Department of Science and Technology (DST), and the Indian Council of Medical Research (ICMR); he is also currently involved in an NIMH multicenter international study on OCD. DJS has received research grants and/or consultancy honoraria from Lundbeck and Servier. HBS has received research funds for a multisite industry-sponsored clinical trial from Biohaven Inc., royalties from Cambridge University Press and UpToDate Inc., and a stipend from the American Medical Association for serving as an Associate Editor for JAMA Psychiatry. The other authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shephard, E., Stern, E.R., van den Heuvel, O.A. et al. Toward a neurocircuit-based taxonomy to guide treatment of obsessive–compulsive disorder. Mol Psychiatry 26, 4583–4604 (2021). https://doi.org/10.1038/s41380-020-01007-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-020-01007-8
This article is cited by
-
Obsessive–compulsive symptoms and brain lesions compatible with multiple sclerosis
Journal of Neural Transmission (2024)
-
Obsessive-compulsive symptoms in two patients with strategic basal ganglia lesions
Molecular Psychiatry (2023)
-
Mechanisms underlying capsulotomy for refractory obsessive-compulsive disorder: neural correlates of negative affect processing overlap with deep brain stimulation targets
Molecular Psychiatry (2023)
-
Cognitive outcomes following functional neurosurgery in refractory OCD patients: a systematic review
Neurosurgical Review (2023)
-
Dissecting Psychiatric Heterogeneity and Comorbidity with Core Region-Based Machine Learning
Neuroscience Bulletin (2023)