Abstract
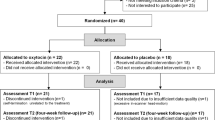
A discrepancy in oxytocin’s behavioral effects between acute and repeated administrations indicates distinct underlying neurobiological mechanisms. The current study employed a combination of human clinical trial and animal study to compare neurochemical changes induced by acute and repeated oxytocin administrations. Human study analyzed medial prefrontal metabolite levels by using 1H-magnetic resonance spectroscopy, a secondary outcome in our randomized, double-blind, placebo-controlled crossover trial of 6 weeks intranasal administrations of oxytocin (48 IU/day) and placebo within-subject design in 17 psychotropic-free high-functioning men with autism spectrum disorder. Medial prefrontal transcript expression levels were analyzed in adult male C57BL/6J mice after intraperitoneal injection of oxytocin or saline either once (200 ng/100 μL/mouse, n = 12) or for 14 consecutive days (200 ng/100 μL/mouse/day, n = 16). As the results, repeated administration of oxytocin significantly decreased the medial prefrontal N-acetylaspartate (NAA; p = 0.043) and glutamate–glutamine levels (Glx; p = 0.001), unlike the acute oxytocin. The decreases were inversely and specifically associated (r = 0.680, p = 0.004 for NAA; r = 0.491, p = 0.053 for Glx) with oxytocin-induced improvements of medial prefrontal functional MRI activity during a social judgment task not with changes during placebo administrations. In wild-type mice, we found that repeated oxytocin administration reduced medial frontal transcript expression of N-methyl-d-aspartate receptor type 2B (p = 0.018), unlike the acute oxytocin, which instead changed the transcript expression associated with oxytocin (p = 0.0004) and neural activity (p = 0.0002). The present findings suggest that the unique sensitivity of the glutamatergic system to repeated oxytocin administration may explain the differential behavioral effects of oxytocin between acute and repeated administration.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Yamasue H, Yee JR, Hurlemann R, Rilling JK, Chen FS, Meyer-Lindenberg A, et al. Integrative approaches utilizing oxytocin to enhance prosocial behavior: from animal and human social behavior to autistic social dysfunction. J Neurosci. 2012;32:14109–17.
Young LJ, Barrett CE. Neuroscience. Can oxytocin treat autism? Science. 2015;347:825–6.
Harris JC, Carter CS. Therapeutic interventions with oxytocin: current status and concerns. J Am Acad Child Adolesc Psychiatry. 2013;52:998–1000.
Andari E, Duhamel JR, Zalla T, Herbrecht E, Leboyer M, Sirigu A. Promoting social behavior with oxytocin in high-functioning autism spectrum disorders. Proc Natl Acad Sci USA. 2010;107:4389–94.
Watanabe T, Abe O, Kuwabara H, Yahata N, Takano Y, Iwashiro N, et al. Mitigation of sociocommunicational deficits of autism through oxytocin-induced recovery of medial prefrontal activity: a randomized trial. JAMA Psychiatry. 2014;71:166–75.
Guastella AJ, Einfeld SL, Gray KM, Rinehart NJ, Tonge BJ, Lambert TJ, et al. Intranasal oxytocin improves emotion recognition for youth with autism spectrum disorders. Biol Psychiatry. 2010;67:692–4.
Domes G, Heinrichs M, Kumbier E, Grossmann A, Hauenstein K, Herpertz SC. Effects of intranasal oxytocin on the neural basis of face processing in autism spectrum disorder. Biol Psychiatry. 2013;74:164–71.
Gordon I, Vander Wyk BC, Bennett RH, Cordeaux C, Lucas MV, et al. Oxytocin enhances brain function in children with autism. Proc Natl Acad Sci USA. 2013;110:20953–8.
Aoki Y, Yahata N, Watanabe T, Takano Y, Kawakubo Y, Kuwabara H, et al. Oxytocin improves behavioural and neural deficits in inferring others’ social emotions in autism. Brain. 2014;137:3073–86.
Takayanagi Y, Yoshida M, Takashima A, Takanami K, Yoshida S, Nishimori K, et al. Activation of supraoptic oxytocin neurons by secretin facilitates social recognition. Biol Psychiatry. 2015;81:243–51.
Scheele D, Kendrick KM, Khouri C, Kretzer E, Schläpfer TE, Stoffel-Wagner B, et al. An oxytocin-induced facilitation of neural and emotional responses to social touch correlates inversely with autism traits. Neuropsychopharmacol. 2014;39:2078–85.
Benner S, Yamasue H. Clinical potential of oxytocin in autism spectrum disorder: current issues and future perspectives. Behav Pharmacol. 2018;29:1–12.
Yamasue H. Promising evidence and remaining issues regarding the clinical application of oxytocin in autism spectrum disorders. Psychiatr Clin Neurosci. 2016;70:89–99.
Yamasue H, Domes G. Oxytocin and autism spectrum disorders. Curr Top Behav Neurosci. 2017;35:449–65.
Bales KL, Solomon M, Jacob S, Crawley JN, Silverman JL, Larke RH, et al. Long-term exposure to intranasal oxytocin in a mouse autism model. Transl Psychiatry. 2014;4:e480.
Bales KL, Perkeybile AM, Conley OG, Lee MH, Guoynes CD, Downing GM, et al. Chronic intranasal oxytocin causes long-term impairments in partner preference formation in male prairie voles. Biol Psychiatry. 2013;74:180–8.
Aoki Y, Watanabe T, Abe O, Kuwabara H, Yahata N, Takano Y, et al. Oxytocin’s neurochemical effects in the medial prefrontal cortex underlie recovery of task-specific brain activity in autism: a randomized controlled trial. Mol Psychiatry. 2011;20:447–53.
Watanabe T, Kuroda M, Kuwabara H, Aoki Y, Iwashiro N, Tatsunobu N, et al. Clinical and neural effects of six-week administration of oxytocin on core symptoms of autism. Brain. 2015;138:3400–12.
Harada M, Taki MM, Nose A, Kubo H, Mori K, Nishitani H. et al. Non-invasive evaluation of the GABAergic/glutamatergic system in autistic patients observed by MEGA-editing proton MR spectroscopy using a clinical 3 tesla instrument. J Autism Dev Disord. 2011;41:447–54.
Purcell A, Jeon O, Zimmerman A, Blue M, Pevsner J. Postmortem brain abnormalities of the glutamate neurotransmitter system in autism. Neurology. 2001;57:1618–28.
Wechsler D. WAIS-R: manual: Wechsler adult intelligence scale—revised. Revised edition. San Antonio: Harcourt Brace Jovanovich [for] Psychological Corporation; 1981.
Lord C, Rutter M, Le Couteur A. Autism diagnostic interview-revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord. 1994;24:659–85.
Lord C, Rutter M, Goode S, Heemsbergen J, Jordan H, Mawhood L, et al. Autism diagnostic observation schedule: a standardized observation of communicative and social behavior. J Autism Dev Disord. 1989;19:185–212.
Feifel D, Macdonald K, Nguyen A, Cobb P, Warlan H, Galangue B, et al. Adjunctive intranasal oxytocin reduces symptoms in schizophrenia patients. Biol Psychiatry. 2010;68:678–80.
McCracken JT, McGough J, Shah B, Cronin P, Hong D, Aman MG, et al. Risperidone in children with autism and serious behavioral problems. N Engl J Med. 2002;347:314–21.
Tachibana M, Kagitani-Shimono K, Mohri I, Yamamoto T, Sanefuji W, Nakamura A, et al. Long-term administration of intranasal oxytocin is a safe and promising therapy for early adolescent boys with autism spectrum disorders. J Child Adolesc Psychopharmacol. 2013;23:123–7.
Anagnostou E, Soorya L, Chaplin W, Bartz J, Halpern D, Wasserman S, et al. Intranasal oxytocin versus placebo in the treatment of adults with autism spectrum disorders: a randomized controlled trial. Mol Autism. 2012;3:16.
Aoki Y, Abe O, Yahata N, Kuwabara H, Natsubori T, Iwashiro N, et al. Absence of age-related prefrontal NAA change in adults with autism spectrum disorders. Transl Psychiatry. 2012a;2:e178.
Teng BL, Nonneman RJ, Agster KL, Nikolova VD, Davis TT, Riddick NV, et al. Prosocial effects of oxytocin in two mouse models of autism spectrum disorders. Neuropharmacology. 2013;72:187–96.
Abbott C, Bustillo J. What have we learned from proton magnetic resonance spectroscopy about schizophrenia? A critical update. Curr Opin Psychiatry. 2006;19:135–9.
Goff DC, Coyle JT. The emerging role of glutamate in the pathophysiology and treatment of schizophrenia. Am J Psychiatry. 2001;158:1367–77.
Moffett JR, Ross B, Arun P, Madhavarao CN, Namboodiri AM. N-acetylaspartate in the CNS: from neurodiagnostics to neurobiology. Prog Neurobiol. 2007;81:89–131.
Rubin Y, LaPlaca MC, Smith DH, Thibault LE, Lenkinski RE. The effect of N-acetylaspartate on the intracellular free calcium concentration in NTera2-neurons. Neurosci Lett. 1995;198:209–12.
Thatcher NM, Badar-Goffer RS, Ben-Yoseph O, McLean MA, Morris PG, Prior MJ, et al. A comparison of some metabolic effects of N-methylaspartate stereoisomers, glutamate and depolarization: a multinuclear MRS study. Neurochem Res. 2002;27:51–58.
Tranberg M, Stridh MH, Guy Y, Jilderos B, Wigstrom H, Weber SG, et al. NMDA-receptor mediated efflux of N-acetylaspartate: physiological and/or pathological importance? Neurochem Int. 2004;45:1195–204.
Yamakura T, Shimoji K. Subunit- and site-specific pharmacology of the NMDA receptor channel. Prog Neurobiol. 1999;59:279–98.
Akashi K, Kakizaki T, Kamiya H, Fukaya M, Yamasaki M, Abe M, et al. NMDA receptor GluN2B (GluR epsilon 2/NR2B) subunit is crucial for channel function, postsynaptic macromolecular organization, and actin cytoskeleton at hippocampal CA3 synapses. J Neurosci. 2009;29:10869–82.
Meguro H, Mori H, Araki K, Kushiya E, Kutsuwada T, Yamazaki M, et al. Functional characterization of a heteromeric NMDA receptor channel expressed from cloned cDNAs. Nature. 1992;357:70–74.
Mairesse J, Gatta E, Reynaert ML, Marrocco J, Morley-Fletcher S, Soichot M, et al. Activation of presynaptic oxytocin receptors enhances glutamate release in the ventral hippocampus of prenatally restraint stressed rats. Psychoneuroendocrinol. 2015;62:36–46.
Mesic I, Guzman YF, Guedea AL, Jovasevic V, Corcoran KA, Leaderbrand K, et al. Double dissociation of the roles of metabotropic glutamate receptor 5 and oxytocin receptor in discrete social behaviors. Neuropsychopharmacol. 2015;40:2337–46.
Monaco SA, Gulchina Y, Gao WJ. NR2B subunit in the prefrontal cortex: a double-edged sword for working memory function and psychiatric disorders. Neurosci Biobehav Rev. 2015;56:127–38.
Nelson SB, Valakh V. Excitatory/inhibitory balance and circuit homeostasis in autism spectrum disorders. Neuron. 2015;87:684–98.
Guastella AJ, Gray KM, Rinehart NJ, Alvares GA, Tonge BJ, Hickie IB, et al. The effects of a course of intranasal oxytocin on social behaviors in youth diagnosed with autism spectrum disorders: a randomized controlled trial. J Child Psychol Psychiatry. 2015;56:444–52.
Bejjani A, O’Neill J, Kim JA, Frew AJ, Yee VW, Ly R, et al. Elevated glutamatergic compounds in pregenual anterior cingulate in pediatric autism spectrum disorder demonstrated by 1H MRS and 1H MRSI. PLoS ONE. 2012;7:e38786.
Acknowledgements
We thank Drs. T. Kadowaki, T. Iwatsubo, and Y. Arakawa in the Project to Create Early-Stage and Exploratory Clinical Trial Centres for providing MRI scanning opportunities. A part of this study is the result of Grants-in-Aid for Scientific Research (KAKENHI) from the Japan Society for the Promotion of Science (23659558; 26670535 to HY), the Strategic Research Program for Brain Sciences of the Japan Agency for Medical Research and Development (to HY and MaKa), and the Center of Innovation Program of the Japan Science and Technology Agency (HY). HY had full access to all study data and takes responsibility for its integrity and the accuracy of the data analysis. We thank Richard Lipkin, PhD, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript. A research grant from Takeda Science Foundation (to HB).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
41380_2018_249_MOESM1_ESM.docx
Supplementary information for Benner et al., “Neurochemical evidence for differential effects of acute and repeated oxytocin administration”
Rights and permissions
About this article
Cite this article
Benner, S., Aoki, Y., Watanabe, T. et al. Neurochemical evidence for differential effects of acute and repeated oxytocin administration. Mol Psychiatry 26, 710–720 (2021). https://doi.org/10.1038/s41380-018-0249-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-018-0249-4
This article is cited by
-
Results of a phase Ib study of SB-121, an investigational probiotic formulation, a randomized controlled trial in participants with autism spectrum disorder
Scientific Reports (2023)
-
Intranasal oxytocin in a genetic animal model of autism
Molecular Psychiatry (2023)
-
A randomized controlled trial of intranasal oxytocin in Phelan-McDermid syndrome
Molecular Autism (2021)
-
Oxytocin-induced increase in N,N-dimethylglycine and time course of changes in oxytocin efficacy for autism social core symptoms
Molecular Autism (2021)
-
Repeated oxytocin prevents central sensitization by regulating synaptic plasticity via oxytocin receptor in a chronic migraine mouse model
The Journal of Headache and Pain (2021)