Abstract
Increasingly, molecular methods are being utilized in the workup of melanocytic neoplasms. To this end, we sought to correlate data from a single nucleotide polymorphism (SNP) array platform based on molecular inversion probes with clinical data. Copy number variation (CNV) data were obtained on 95 melanocytic tumors (6 ordinary nevi, 15 atypical nevi, 34 ambiguous neoplasms, and 40 melanomas) from 92 patients. The average number of significant CNVs was 0 for nevi, 0.6 for atypical nevi (range 0–3), 2.8 for ambiguous neoplasms (range 0–17), and 18.1 for melanomas (range 0–69). Clinical follow-up data were available in 57 of 95 lesions (56 of 92 patients). Tumors from patients with adverse events demonstrated an average number of CNVs of 24.5 (range 6–69) as compared with 7.9 (range 0–35) among tumors without an associated adverse event (p ≤ 0.001). No adverse events were observed in nevi including atypical nevi. Adverse events were found in 2 of 19 ambiguous neoplasms and 10 of 32 melanomas with follow up. In these two latter groups of neoplasms, the correlation between adverse events and the average number of CNVs remained statistically significant even when controlled for Breslow depth (21.5 versus 8.7, p value = 0.036). No neoplasm with adverse events had ≤3 CNVs. These results provide further evidence that SNP array testing for CNVs may be helpful in the classification and prognostication of ambiguous neoplasms. Based on these results, an algorithmic approach to challenging melanocytic neoplasms using CNV data is suggested, using as cutoff of >3 CNVs with some caveats, as the threshold for a positive result. Future clinical validation, using a larger cohort of relevant tumors, will be necessary.
Similar content being viewed by others
Introduction
Histopathological features differentiating benign and malignant melanocytic tumors are well-known to the dermatopathologist and include architectural and cytological features [1]. Histological examination remains the gold standard today, as it was 100 years ago. While the vast majority of melanocytic tumors can be easily classified as benign or malignant, diagnostic uncertainty exists in a significant minority of tumors when based on histopathology alone. In order to allow for more specific classification, various methods have been pursued including fluorescence in situ hybridization, and comparative genomic hybridization (CGH) [2].
The utility of single nucleotide polymorphism (SNP) array, a modified form of CGH, is based upon the premise that melanomas tend to have multiple genetic copy number abnormalities usually involving segments of chromosomes, whereas nevi tend to have few or none [3, 4]. These alterations can be evaluated using SNP array testing. In this study our aim was to correlate copy number changes with clinical data in a cohort that included nevi and melanomas, as well as histologically borderline/ambiguous neoplasms using a platform designed for formalin-fixed paraffin embedded tissue (FFPE).
Methods
Patients and clinical data
This study was approved by the Institutional Review Board at the University of Michigan. Representative melanocytic neoplasms were collected from the University of Michigan surgical pathology archives (both in-house cases and consultation cases) to include cases spanning the years 2005–2019, with some cases collected retrospectively and some collected prospectively. An effort was made to acquire cases which covered the entire spectrum of melanocytic neoplasia and no cases for which SNP array data were interpretable were excluded. Tumors were classified as nevi, atypical nevi (tumors that are non-malignant by histology but demonstrate some unusual features), ambiguous or borderline melanocytic tumors (tumors in which differential diagnosis rests between nevus and melanoma), and unequivocal melanomas. For ambiguous neoplasms, the decision for performing SNP array testing was based on the clinical need assessment of the primary dermatopathologist. To assist in defining different classes of melanocytic neoplasms, SNP array testing was also retrospectively performed on randomly selected nevi, atypical nevi, and unequivocal melanomas. In a small subset of melanoma cases, testing was performed to evaluate clonal relationship between morphologic subpopulations. Testing results were excluded only if they were uninterpretable due to low run quality (high background). A total of 95 cases were identified. Final diagnosis for each case was made by the original pathologist (many cases were also seen by multiple pathologists in intradepartmental consultation) and confirmed by subsequent review (AAA and AKA). For difficult or borderline cases, the diagnosis was generated by consensus. Demographic and follow-up data were gathered from electronic medical records and/or from the referring institution as available. An adverse event was recorded if there was local recurrence, cutaneous metastasis, distant metastasis, or death. Sentinel or regional lymph node metastases discovered during staging were not considered an adverse event for purposes of this study.
SNP array testing
SNP microarray analysis was performed using the OncoScan FFPE Express 3.0 assay kit (Affymetrix, Santa Clara, CA) as per manufacturer’s recommendation. The assay utilizes Molecular Inversion Probe (MIP) technology, which is optimized for highly degraded FFPE samples (probe interrogation site of just 40 base pairs). The assay employs 220,000 SNP MIP probes which ensure a resolution of 50–100 kb in selected genomic regions covering 900 cancer genes and of 300 kb outside of these regions. Briefly, ten unstained FFPE tissue sections cut at 10 µm were obtained and tumor was macrodissected using a hematoxylin and eosin-stained slide as a guide. DNA was extracted and purified from the samples using the QIAamp DNA FFPE Tissue Kit (Qiagen, Dusseldorf, Germany) according to the manufacturer’s protocols. Extracted DNA was quantified using the Qubit dsDNA HS assay kit using Qubit 2.0 fluorometer (Invitrogen, Carlsbad, CA, USA) following the manufacturer’s protocol. A total of 80 ng of DNA from each sample was annealed to the MIP probe panel. Annealed MIPs were circularized, followed by enzymatic removal of un-ligated probes and template DNA. Remaining MIPs were linearized, amplified, enzymatically fragmented, and hybridized to oligonucleotide microarrays. The arrays were washed, scanned, and the results were analyzed and interpreted using OncoScan Console and Nexus Express for OncoScan 3 software (BioDiscovery, El Segundo, CA, USA) as previously described [5, 6]. Out of 94 cases, SNP array results were interpretable in 89 cases.
Statistical analysis
Microsoft Excel software was used for data analysis. Individual t-statistics and p values were obtained to assess the differences in the number of copy number variations (CNVs) between various groups of nevi, ambiguous lesions, and melanomas. Regression testing and analysis of covariance was used to perform multivariate analysis when multiple variables were involved. A p value of 0.05 was considered the cutoff for statistical significance.
Results
Cases and patient characteristics
Our study consisted of 95 tumors (6 nevi, 15 atypical nevi, 34 ambiguous neoplasms, and 40 melanomas) from 92 total patients. One atypical nevus and one ambiguous neoplasm were collected from a single patient, one ambiguous neoplasm and one melanoma were collected from a separate single patient (see Special cases below), and two morphologically distinct melanomas were collected from another single patient. All tumors had a dermal component of at least 0.5 mm in width and 0.5 mm in thickness to ensure tissue adequacy for testing. No pure in situ tumors were included. Some cases underwent macrodissection to enrich for tumor cells. An estimated tumor purity was assigned to each case. See Table 1 for general patient and tumor characteristics.
Nevi
A total of six nevi were collected from patients with an average age of 21.5 years (range 9–30) and consisting of 67% females and 33% males. Lesions were taken from the head and neck (50%), trunk (33%), and extremities (17%). Histological subtypes in this group included deep penetrating nevi (33%), intradermal nevi (33%), and two intradermal Spitz nevi (33%). Tumor purity information was available for two cases with an average of 27.5% (range 25–30%). Clinical follow-up data were available for one case, and no adverse events were observed at 940 days follow-up.
Atypical nevi
A total of 15 atypical nevi were collected from patients with an average age of 36.9 years (range 2–83) and consisting of 33% females and 67% males. Distribution of anatomic sites included extremities (40%), trunk (33%), and head and neck (27%). Histological subtypes in this group included atypical Spitz nevi (40%), atypical cellular blue nevi (27%), atypical combined nevi (13%), one atypical deep penetrating nevus (7%), one atypical congenital nevus (7%), and one atypical BAP1-deficient nevus (7%). Tumor purity information was available for 11 cases with an average of 59.6% (range 5–80%). Follow-up data were available for five cases. No adverse events were observed in this group at an average follow-up of 1167 days.
Ambiguous melanocytic neoplasms
A total of 34 ambiguous tumors were collected from patients with an average age of 28.3 years (range 3–62) and consisting of tumors from 50% females and 50% males. Lesions were distributed on the head and neck (41%), trunk (32%), and extremities (26%). Histological subtypes in this category included atypical Spitz tumors (32%), BAP1-deficient tumors (24%), pigmented epithelioid melanocytomas (12%), deep penetrating nevus-like tumors (9%), cellular blue-like (3%), congenital-type (3%), and melanocytic tumors of uncertain malignant potential/other (17%). Tumor purity information was available for twenty cases with an average of 53.5% (range 20–90%). The Breslow depth of ambiguous lesions ranged from 1.0 mm to 11.0 mm (average 3.2 mm, info was available for 25 cases). Follow-up data were available for 19 patients with an average follow-up time of 534 days. Two cases experienced an adverse event (one distant metastasis and one deep local recurrence with morphologic progression to melanoma).
Melanoma
A total of 40 melanomas were collected from patients with an average age of 53.9 years (range 0.3–92 years) and consisting of 52% females and 48% males. Lesions were taken from the extremities (45%), head and neck (33%), trunk (15%), and mucosa (8%). Histological subtypes included spitzoid (13%), desmoplastic/spindle cell (13%), nodular (13%), superficial spreading (13%), pigment synthesizing (5%), nevoid (5%), acral lentiginous (3%), and other (18%). This group also included eight recurrent/cutaneous metastatic lesions (20%) on which SNP array testing was performed. Tumor purity information was available for 29 cases with an average of 61.6% (range 20–90%). For primary cutaneous melanomas, the Breslow depth ranged from 0.7 mm to 15.0 mm (average 4.6, info was available for 30 cases) with 37% of cases having a pathologic T stage of T1 or 2 (≤2 mm). Follow-up data were available for 32 of 40 cases (80%) with an average follow-up period of 636 days. The ten patients who experienced an adverse event had an average follow-up time of 936 days and the 22 patients who did not experience an adverse event had an average follow-up period of 499 days. Twenty-four patients in this group underwent a sentinel lymph node biopsy or regional lymph node dissection, and of these nine were positive (38%).
SNP array results
Overall, 62 of 95 tumors (65%) had abnormalities on SNP array. Twelve of 57 cases (21%) with available clinical data had an adverse event. The average number of CNVs/tumor among cases with adverse events was 24.5 (range 6–69) as compared with 7.9 (range 0–35) in cases without adverse events (p < 0.001). Results are summarized in Table 2.
Nevi and atypical nevi
No CNVs were found in the nevus group (n = 6). In the atypical nevus group, 7 out of 15 cases (47%) showed CNVs. Three of these seven cases demonstrated only isolated changes known to be associated with indolent melanocytic tumors (two with 11p gains and one with 3p21 loss). The other four cases demonstrated one to three CNVs. When non-significant CNVs (11p gains and 3p21 losses) are excluded, the average number of CNVs/tumor in the atypical nevus group was 0.6 while among both nevi and atypical nevi was 0.4 (see Table 3).
Ambiguous
Twenty one out of 34 ambiguous tumors (62%) demonstrated 1 to 17 CNVs for an average of 2.8 CNVs/tumor. Only two patients in this group subsequently developed adverse events (average CNVs is 8.5/tumor); one of which developed systemic metastasis (her tumor had eight CNVs) and one developed deep soft tissue recurrence with morphologic progression to Spitzoid melanoma (her tumor had nine CNVs). For tumors with CNVs, the average Breslow depth was 3.6 mm, while tumors with no CNVs, the average Breslow depth was 2.4 mm (p value = 0.12). See Table 4.
Melanoma
Thirty-seven of 40 melanomas (93%) in this group demonstrated 2–69 CNVs for an average of 18.1 CNVs/tumor. Patients with an adverse event had a greater average number of CNVs (average 27.7, range 6–69) in comparison to those without (average 13.0, range 0–35) with a p value of 0.007. Tumors that resulted in positive sentinel or regional lymph node metastasis had a greater number of CNVs (average 21.9, range 0–69) than those that did not (average 10.9, range 0–35), although this difference did not reach statistical difference (p value of 0.06). Three melanoma cases showed no CNVs, another three cases demonstrated only two CNVs and one case had three CNVs (total of seven cases with 3 or less CNVs). In four melanoma cases with CNVs of more than 0 but less or equal to 3, there was at least one specific alteration that is frequently encountered in melanomas (homozygous deletion of 9p (spanning the CDKN2A gene), loss of 6q (including the MYB gene), or gains involving 8q24 (MYC) or 6p25 (RREB1).
Comparison between and within groups
The average number of CNVs/tumor was lower in nevi, including nevi and atypical nevi (0.4) compared with melanoma (18.1) and this difference was statistically significant (p < 0.001). The correlation coefficient R between the number of CNV and the Breslow depth for ambiguous and melanoma cases combined is 0.28 (p value = 0.03), suggesting weak positive correlation. However, the difference of CNVs between ambiguous and melanoma cases remained statistically significant even after controlling for Breslow depth by analysis of covariance (p value < 0.001).
The difference in CNVs between all cases with adverse events (average 24.5, (range 6–69)) and those without (average 7.9, (range 0–35)) was also statistically significant (p < 0.001). When evaluating ambiguous lesions and primary cutaneous melanomas with available information on Breslow depth, the number of CNVs in lesions with adverse events was 21.5 versus 8.7 in lesions with no adverse events. This difference was statistically significant even after controlling for potential confounding effect of Breslow depth by multivariate analysis (p value = 0.036). See Table 5.
Seven melanoma cases had tumor purity of less than 40% with an average CNVs of 13.2/tumor (range 0–27). The other 22 cases with tumor purity of more than 40% had an average CNVs of 19.1/tumor (range 0–69), (p value = 0.10). For primary melanoma cases with a Breslow depth of ≤2 mm, the average CNV was 11.7 while cases with a Breslow depth of >2 mm had an average CNV of 19.7 (p value = 0.10). The difference in average CNVs/tumor between melanomas with adverse events (average 27.7, (range 6–69)) and those without (average 13.0, (range (0–35)) was statistically significant (p = 0.007). For primary cutaneous melanomas with available information on Breslow depth, the average CNV and Breslow depth were 24.0 CNV/tumor and 4.7 mm, respectively in tumors with adverse events (n = 5). This is in contrast to 12.6 CNV/tumor and 4.0 mm for those melanomas without adverse event (n = 19). Interestingly, after controlling for Breslow depth, this association between the number of CNV/tumor and adverse events lost its statistical significance (p value = 0.17). The difference in the average CNVs/tumor between melanoma with positive sentinel or regional nodes (average 21.9, (range 0–69)) and those without (average 10.9, (range 0–35)) trended toward significance (p = 0.06). Comparisons are summarized in Fig. 1.
Intergroup comparisons. (Left) Comparison of CNV burden among diagnostic groups reveals significant correlation with increasing atypia and risk. (Middle) Melanocytic tumors (including ambiguous tumors and melanomas) with adverse events displayed significantly higher CNV burden than tumors without adverse events. (Right) Considering only melanomas, tumors with adverse events were associated with significantly higher CNV burden than those without adverse events. Adverse events were defined as recurrent disease (local, regional, or distant) or any distant metastasis.
Sensitivity and specificity
If a cutoff of >3 CNVs are selected for a positive result, the SNP array test is interpreted as positive in 33 out of 40 melanomas, including all ten melanomas with adverse events (sensitivity of 82.5%) and in no nevi or atypical nevi (specificity of 100%). For ambiguous tumors, the test will be positive in 8 out of 34 cases (23.5%), including the two patients with adverse events.
Special cases
Two cases deserve special mention. One case was that of a 15-year-old male with a large congenital nevus on the trunk who developed two nodules. Upon histologic examination one of the lesions was interpreted as an atypical nevus with congenital features (this case was included in the atypical nevus group) while the other one was diagnosed as a markedly atypical epithelioid melanocytic proliferation (included in the ambiguous group). The atypical nevus demonstrated three CNVs including an area of chromothripsis involving chromosome 1p. The borderline tumor showed five CNVs, including the same three seen in the atypical nevus. The entire lesion was excised and the patient was disease free at 3.5 years after diagnosis (see Fig. 2).
Biopsy from a nodule within a congenital nevus on the trunk of a 15-year-old male showing a predominately intradermal nevus with bland cytology and congenital growth pattern (a Low power, b High power). This lesion demonstrated three copy number variations including an area of chromothripsis involving chromosome 1p (c).
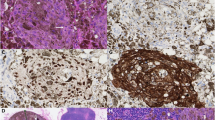
A second special case is that of a young female, who at the age of 15 had a biopsy of a lesion on the right thigh. This was called a markedly atypical compound melanocytic proliferation and revealed eight CNVs on SNP array (this tumor was included in the ambiguous group with adverse event for purposes of this study). Two years later she developed lymphadenopathy and biopsy of a right inguinal lymph node revealed metastatic spread. SNP array analysis of this tumor revealed nine CNVs (this metastatic tumor was included in the melanoma group, but excluded from the analysis for adverse events). At most recent follow-up, she was alive with lymph node and liver metastases (see Fig. 3).
Right thigh lesion from a 15-year-old female demonstrating a markedly atypical compound melanocytic proliferation with fusiform to ovoid melanocytes in nests and single units with prominent nucleoli and a moderate amount of cytoplasm (a Low power, b High power). Consensus diagnosis was that of a borderline melanocytic proliferation of uncertain malignant potential. SNP array analysis revealed eight copy number variations (c). This patient subsequently developed metastatic disease (regional lymph node and liver).
Discussion
Light microscopy using hematoxylin and eosin stained sections of FFPE specimens has been the gold standard in the classification and diagnosis of melanocytic tumors for many years. While this method is adequate for the vast majority of lesions, there remains a substantial minority of tumors that cannot be accurately classified using light microscopy alone. For many of these melanocytic tumors diagnostic concordance has been low, even among expert pathologists [7,8,9,10]. In recent years, the use of ancillary testing, like CGH/SNP array has increased, in order to provide additional diagnostic information [11, 12]. However, interpretation guidelines are still being delineated. In this study we evaluated the presence of chromosomal abnormalities by SNP array in a cohort of melanocytic tumors spanning the spectrum from benign to malignant and correlated the results with histologic diagnoses and available clinical follow-up data.
The number of CNVs was observed to increase with the degree of histologic atypia from benign nevus to melanoma. When melanomas and ambiguous tumors are evaluated together, those with an adverse event had a greater number of CNVs in comparison with those without an adverse event, even after controlling for the Breslow depth. When this analysis was limited to specific diagnostic groups (ambiguous tumors or melanomas alone), the association lost statistical significance; however, the number of tumors was low in some of these subcategories. These results provide further evidence that SNP array testing for CNVs may be helpful in the classification and prognostication of melanocytic neoplasms.
It has been previously shown that CNVs can be encountered in nevi and indolent melanocytic tumors. For example, the presence of 11p gains is seen in a subset of desmoplastic Spitz nevi characterized also by HRAS mutation [13]. The recently characterized translocation associated spitzoid lesions can be associated with isolated CNVs spanning the loci for the rearranged genes. For example, NTRK1 translocated neoplasms often demonstrate an isolated deletion involving chromosome 1q22-q23.1. The breakpoints of this deletion are within LMNA and NTRK1 genes and result in an LMNA-NTRK1 fusion product. This fusion has been described in 10.7% of Spitz nevi, 25% of atypical Spitz tumors and 21.2% of spitzoid melanomas and therefore, in isolation has no prognostic implications [14, 15]. The BAP1-deficient melanocytic tumors, which for the most part behave in an indolent fashion, are characterized by an isolated loss centered on 3p21 locus spanning the BAP1 gene [16]. Finally, proliferative nodules developing in congenital nevi are characterized by gains and losses of entire chromosomes [17]. Accordingly, we believe that if there is strong evidence from the literature and a general consensus between experts that a particular CNV is associated with indolent tumors or carries no prognostic value (present at the whole spectrum of a particular class of melanocytic neoplasms), it can be considered as insignificant. This may improve the overall performance and reliability of the test. As might be expected, the list of such CNVs could evolve in the future as more data is being collected and analyzed.
In our dataset, if the isolated abnormalities associated with indolent tumors are excluded, 4 out of 21 nevi and atypical nevi demonstrated CNVs. Three of these cases showed 1 to 2 CNVs while one showed 3 CNVs including an area or chromothripsis on chromosome 1p. Based on these findings we propose that finding >3 CNVs in a borderline melanocytic tumor supports a potential for an aggressive behavior and should trigger more aggressive treatment. An exception to this rule (not observed in our cohort) is the occurrence of whole chromosomal gains and/or losses without segmental abnormalities, which have been described in indolent proliferative nodules. Also finding ≤3 CNVs may be interpreted as a positive result if they include selected abnormalities such as homozygous losses of 9p21 (CDKN2A) or gains involving 11q13 (CCND1), 8q24 (MYC) or 6p25 (RREB1) loci [18,19,20,21]. As an aside, an interesting occurrence in our dataset is the finding of chromothripsis in a case of an atypical nevus. Prior studies have shown that chromothripsis is associated with adverse outcome in cancers including melanoma [22]. Our study shows that chromothripsis may be encountered in indolent melanocytic tumors and in isolation does not seem to always correlate with an adverse outcome.
Our results are in line with prior studies showing that most melanomas have multiple copy number abnormalities of segments of chromosomes, whereas most benign nevi do not [3, 23,24,25]. Other studies have also looked at outcome data in spitzoid melanocytic tumors [26,27,28], and while our study looked at a more diverse collection of melanocytic tumors, our results correlate with these prior studies.
In our dataset, 37 of 40 melanomas demonstrate CNVs with an average of 18.1 CNVs per case. If a cutoff of >3 CNVs is used, the sensitivity and specificity of the SNP array test in differentiating melanomas from nevi are 82.5% and 100%, respectively. Based on these findings we suggest an algorithmic approach to melanocytic tumor diagnosis (see Fig. 4). Although this proposed algorithm has not been prospectively tested, we believe it may represent a guide for designing further studies to assess the clinical utility and role of SNP array as an ancillary test in the evaluation of melanocytic neoplasms. In this algorithm, melanocytic neoplasms in which a definitive diagnosis of nevus or melanoma can be rendered by conventional methods do not need further molecular analysis. For borderline tumors, an effort should be made to sub-classify them in three categories based on histologic impression: (1) ambiguous favor benign, (2) ambiguous, or (3) ambiguous favor malignant. When a benign diagnosis is favored histologically and SNP/CGH array is negative, or a malignant diagnosis is favored and SNP/CGH array is positive, the tumors can be diagnosed as nevus (probably with an atypical modifier) and melanoma, respectively. When the diagnosis is ambiguous and neither a nevus nor a melanoma can be favored on histology, a diagnosis of “ambiguous, favor nevus” can be rendered if SNP/CGH array is negative. Conversely, if SNP/CGH array is positive, the diagnosis would be “ambiguous, favor melanoma”. Finally, if a benign diagnosis is favored histologically and SNP/CGH array is positive, or a malignant diagnosis is favored and the test is negative, the lesion should be regarded as borderline with uncertain biological potential.
For practical purposes, it is important to emphasize that SNP/CGH array should be used as only as an ancillary tool to provide further information for melanocytic neoplasms of uncertain malignant potential (histologically ambiguous tumors). We do not currently recommend using molecular techniques to support a histologically unequivocally benign or malignant diagnosis, as this is not economically appropriate and the risk of a false positive or false negative result in these groups is amplified.
This study has several limitations. Our series is moderately sized overall, heterogenous in its inclusion criteria and partially retrospective in nature. Another important potential limitation to this study is related to tumor purity. Previous studies have suggested that for CNVs to be reliably detected, the neoplastic cell population should represent at least 40% of the tested sample [29]. Although the two cases of nevi with available information had an average tumor purity of less than 40%, the three other categories had an average tumor purity of more than 40% suggesting that the detected progressive increase in CNVs represents a genuine difference in the genomic makeup of these tumors rather than an artifact related to analytic sensitivity of the test. Moreover, even in the melanoma group, the cases with less than 40% tumor purity did show several CNVs; albeit at a lower average number relative to cases with more than 40% tumor purity and this difference did not reach statistical significance. We, therefore, believe that further studies to include the whole spectrum of melanocytic neoplasms are still needed to provide additional information on the full range of genetic aberrations in these tumors and on the utility of this information in clinical practice. While most melanomas had numerous CNVs, the presence of melanomas with ≤3 CNVs is a proof that such melanomas do exist and therefore limits the use of SNP array as a means to independently exclude melanoma.
As previously stated, SNP array testing should only be interpreted in the clinical and pathological context and should not be thought of as diagnostic in isolation. Similarly, our study provides evidence that CNV data correlate with the risk of an adverse event in patients with melanoma; however, our study is limited in size with regard to ambiguous tumors with adverse events, and further studies are needed to determine risk levels based on data for an individual patient, especially as our limited data lost their statistical significance upon multivariate analysis. Our study is also not controlled for all histological or clinical features, which might deliver a confounding effect. In recognition that melanoma is a histologically diverse disease, an effort was made to include a diverse range of histological subtypes. Inevitably, not every type of tumor is represented and some histological subtypes are represented in only small numbers. Since most of the ambiguous cases were received in consultation, follow-up data were not available for some cases and limited in others. The average length of follow-up was shorter for patients who did not experience an adverse event, likely because patients who are doing well are more likely to follow-up locally and less frequently. Finally, complete re-excision was recommended for the majority of tumors in the atypical nevus and ambiguous groups, and this may have an obscuring effect on true biological behavior.
In summary, our data confirm that the number of CNVs determined by SNP array increases along the biological spectrum from benign to malignant and additionally suggests that the number of CNVs correlates with clinical behavior. Based on these data we also have suggested an algorithmic approach for the interpretation of CNV data in the context of challenging melanocytic neoplasms, using as cutoff of >3 CNVs, with caveats as discussed below, as the threshold for a positive result.
A positive result is defined as >3 CNVs, excluding the following insignificant CNVs: 3p21 loss, 11p gain, 1q22-q23.1 loss, and whole chromosomal losses and gains in the setting of a congenital nevus background.
A negative result is defined as ≤3 CNVs, unless any of those CNVs are homozygous loss of CDKN2A, or gains involving 11q13, 8q24, or 6p25.
Although we do acknowledge that the cutoff point of 3 is suggested despite the presence of several limitations to this study, we believe our data are sufficiently strong to provisionally support such an algorithm. These results will need to be confirmed through a formal clinical validation study involving a larger prospective cohort of clinically-relevant neoplasms with clinical outcomes as the reference standard.
References
Massi G, LeBoit PE. Histological diagnosis of nevi and melanoma. Heidelberg; 2014.
Murphy MJ. Molecular diagnostics in dermatology and dermatopathology. New York: Humana Press; 2011.
Bauer J, Bastian BC. Distinguishing melanocytic nevi from melanoma by DNA copy number changes: comparative genomic hybridization as a research and diagnostic tool. Dermatol Ther. 2006;19:40–9.
Bastian BC, Olshen AB, LeBoit PE, Pinkel D. Classifying melanocytic tumors based on DNA copy number changes. Am J Pathol. 2003;163:1765–70.
Foster JM, Oumie A, Togneri FS, Vasques FR, Hau D, Taylor M, et al. Cross-laboratory validation of the OncoScan(R) FFPE Assay, a multiplex tool for whole genome tumour profiling. BMC Med Genomics. 2015;8:5.
Wang Y, Cottman M, Schiffman JD. Molecular inversion probes: a novel microarray technology and its application in cancer research. Cancer Genet. 2012;205:341–55.
Ackerman AB. Discordance among expert pathologists in diagnosis of melanocytic neoplasms. Hum Pathol. 1996;27:1115–6.
Elmore JG, Barnhill RL, Elder DE, Longton GM, Pepe MS, Reisch LM, et al. Pathologists’ diagnosis of invasive melanoma and melanocytic proliferations: observer accuracy and reproducibility study. BMJ. 2017;357:j2813.
Farmer ER, Gonin R, Hanna MP. Discordance in the histopathologic diagnosis of melanoma and melanocytic nevi between expert pathologists. Hum Pathol. 1996;27:528–31.
Shoo BA, Sagebiel RW, Kashani-Sabet M. Discordance in the histopathologic diagnosis of melanoma at a melanoma referral center. J Am Acad Dermatol. 2010;62:751–6.
Dadras SS. Molecular diagnostics in melanoma: current status and perspectives. Arch Pathol Lab Med. 2011;135:860–9.
March J, Hand M, Truong A, Grossman D. Practical application of new technologies for melanoma diagnosis: Part II. Molecular approaches. J Am Acad Dermatol. 2015;72:943–58. quiz 59-60.
Bastian BC, LeBoit PE, Pinkel D. Mutations and copy number increase of HRAS in Spitz nevi with distinctive histopathological features. Am J Pathol. 2000;157:967–72.
Tetzlaff MT, Reuben A, Billings SD, Prieto VG, Curry JL. Toward a molecular-genetic classification of spitzoid neoplasms. Clin Lab Med. 2017;37:431–48.
Wiesner T, He J, Yelensky R, Esteve-Puig R, Botton T, Yeh I, et al. Kinase fusions are frequent in Spitz tumours and spitzoid melanomas. Nat Commun. 2014;5:3116.
Wiesner T, Obenauf AC, Murali R, Fried I, Griewank KG, Ulz P, et al. Germline mutations in BAP1 predispose to melanocytic tumors. Nat Genet. 2011;43:1018–21.
Bastian BC, Xiong J, Frieden IJ, Williams ML, Chou P, Busam K, et al. Genetic changes in neoplasms arising in congenital melanocytic nevi: differences between nodular proliferations and melanomas. Am J Pathol. 2002;161:1163–9.
Gerami P, Beilfuss B, Haghighat Z, Fang Y, Jhanwar S, Busam KJ. Fluorescence in situ hybridization as an ancillary method for the distinction of desmoplastic melanomas from sclerosing melanocytic nevi. J Cutan Pathol. 2011;38:329–34.
Gerami P, Jewell SS, Morrison LE, Blondin B, Schulz J, Ruffalo T, et al. Fluorescence in situ hybridization (FISH) as an ancillary diagnostic tool in the diagnosis of melanoma. Am J Surg Pathol. 2009;33:1146–56.
Gerami P, Li G, Pouryazdanparast P, Blondin B, Beilfuss B, Slenk C, et al. A highly specific and discriminatory FISH assay for distinguishing between benign and malignant melanocytic neoplasms. Am J Surg Pathol. 2012;36:808–17.
Gerami P, Scolyer RA, Xu X, Elder DE, Abraham RM, Fullen D, et al. Risk assessment for atypical spitzoid melanocytic neoplasms using FISH to identify chromosomal copy number aberrations. Am J Surg Pathol. 2013;37:676–84.
Hirsch D, Kemmerling R, Davis S, Camps J, Meltzer PS, Ried T, et al. Chromothripsis and focal copy number alterations determine poor outcome in malignant melanoma. Cancer Res. 2013;73:1454–60.
Harvell JD, Kohler S, Zhu S, Hernandez-Boussard T, Pollack JR, van de Rijn M. High-resolution array-based comparative genomic hybridization for distinguishing paraffin-embedded Spitz nevi and melanomas. Diagn Mol Pathol. 2004;13:22–5.
Wang L, Rao M, Fang Y, Hameed M, Viale A, Busam K, et al. A genome-wide high-resolution array-CGH analysis of cutaneous melanoma and comparison of array-CGH to FISH in diagnostic evaluation. J Mol Diagn. 2013;15:581–91.
Mesbah Ardakani N, Thomas C, Robinson C, Mina K, Harvey NT, Amanuel B, et al. Detection of copy number variations in melanocytic lesions utilising array based comparative genomic hybridisation. Pathology. 2017;49:285–91.
Ali L, Helm T, Cheney R, Conroy J, Sait S, Guitart J, et al. Correlating array comparative genomic hybridization findings with histology and outcome in spitzoid melanocytic neoplasms. Int J Clin Exp Pathol. 2010;3:593–9.
Gerami P, Cooper C, Bajaj S, Wagner A, Fullen D, Busam K, et al. Outcomes of atypical spitz tumors with chromosomal copy number aberrations and conventional melanomas in children. Am J Surg Pathol. 2013;37:1387–94.
Raskin L, Ludgate M, Iyer RK, Ackley TE, Bradford CR, Johnson TM, et al. Copy number variations and clinical outcome in atypical spitz tumors. Am J Surg Pathol. 2011;35:243–52.
Wang L, Rao M, Fang Y, et al. A genome-wide high-resolution array-CGH analysis of cutaneous melanoma and comparison of array-CGH to FISH in diagnostic evaluation. J Mol Diagn. 2013;15:581–91
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alomari, A.K., Miedema, J.R., Carter, M.D. et al. DNA copy number changes correlate with clinical behavior in melanocytic neoplasms: proposal of an algorithmic approach. Mod Pathol 33, 1307–1317 (2020). https://doi.org/10.1038/s41379-020-0499-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-020-0499-y
This article is cited by
-
Towards diagnostic criteria for malignant deep penetrating melanocytic tumors using single nucleotide polymorphism array and next-generation sequencing
Modern Pathology (2022)
-
Genome-wide copy number variations as molecular diagnostic tool for cutaneous intermediate melanocytic lesions: a systematic review and individual patient data meta-analysis
Virchows Archiv (2021)