Abstract
Histomorphologic parameters of atrial appendages removed during the Cox-Maze procedure have been shown to correlate with recurrence of atrial fibrillation. While amyloid deposition has been noted within atrial appendages, the incidence and significance remains incompletely understood. More accurate amyloid typing methodologies and targeted pharmacotherapeutics have recently been developed, prompting pathologists to provide more detailed information about the type of amyloid identified in such samples. This study sought to fully characterize the morphologic characteristics of atrial amyloid as well as its incidence and clinical significance. Tissue archives were queried for atrial appendages removed during the cardiac surgeries (2010–2014). Patient demographics, imaging features, and salient clinical findings were recorded. Pattern and extent of amyloid deposition were recorded. Typing of the amyloid protein, when present, was performed on a subset of cases by laser capture microdissection with mass spectrometry-based proteomic analysis. A total of 383 atrial appendages from 345 consecutive patients were included in the study (mean age, 69 years; range, 26–92 years). Amyloid was present in 46% of patients. A linear relationship was observed between age and presence of atrial amyloidosis. Women were more likely to have atrial amyloidosis. Two distinct morphologies of amyloid were observed: filamentous and nonfilamentous, and correlated perfectly with amyloid type (filamentous = AANF-type amyloid; nonfilamentous = ATTR-type amyloid). Filamentous deposits were observed in 91% of those with amyloid. Amyloid was more likely to be found in the left atrial appendage than the right. Patients with atrial amyloid, irrespective of type, were more likely to have experienced stroke or TIA and more likely to have atrial arrhythmia preoperatively. Postoperatively, those with atrial amyloid are more likely to experience recurrence of arrhythmia than those who did not have atrial amyloid. Understanding the morphologic characteristics of AANF-type amyloid will allow for identification by the light microscopy and obviates the need for expensive ancillary typing techniques. The finding of nonfilamentous amyloid, should still prompt confirmation of amyloid type so that targeted therapy may be employed.
Similar content being viewed by others
Introduction
Atrial appendages, resected during cardiac surgeries, are commonly encountered specimens in the surgical pathology laboratories. Historically, their pathological evaluation has been limited to gross examination only or intraoperative disposal. In recent years, histopathological parameters of appendages removed during Maze procedures have been shown to correlate with the persistence and recurrence of atrial fibrillation (AF) [1,2,3,4]. Such observations make a solid case for routine histologic examination. Consequently, seemingly incidental findings, such as amyloidosis, are encountered that raise questions of their significance.
The reported prevalence of amyloid in atrial appendages varies from 40 to 67% in appendages resected surgically and acquired through autopsy, respectively, and is thought to be primarily of the ANF (atrial natriuretic factor) variety [5,6,7]. Atrial amyloidosis is frequently associated with AF, but whether this accumulation is a cause or consequence of AF is unclear [5, 6, 8,9,10]. This is due, in part, to a paucity of data regarding epidemiology, clinical significance, histomorphologic, and proteomic spectra of atrial amyloidosis in appendages.
Prognostication and treatment selection for cardiac amyloidosis in general relies on early detection and accurate typing. However, data on the relevance of amyloid deposits in atrial appendages is somewhat lacking. Given the estimated disease burden of atrial amyloidosis in these specimens, routine typing would add substantial expense, and currently lacks substantiation through evidence-based medicine [11].
This study aimed to (1) descriptively characterize the morphologic features of amyloid in atrial appendages; (2) analyze the type(s) and relative prevalence of amyloid present in the surgically resected specimens; (3) evaluate if histomorphologic features of amyloid deposits could accurately predict the amyloid type; and (4) investigate the correlation between atrial amyloid deposition and post-Maze recurrence of AF, and other clinical features.
Material and methods
The study was reviewed and approved by the Mayo Clinic Institutional Review Board and Bio-specimens subcommittee (IRB# 13-008181).
Cohort selection and demographics
All patients with resection of one or both atrial appendages at Mayo Clinic in Rochester, MN, between January 1, 2010, and July 31, 2014, were identified from the institutional tissue registry archives. Patient age, sex, height/weight at the time of surgery, and salient clinical information was abstracted from the medical record.
Histomorphological analysis
Paraffin blocks from each case were cut at 3 µm and stained with hematoxylin and eosin (H&E) and sulfated Alcian blue (SAB) by established methods. Light microscopic patterns and extent of amyloid deposition were assessed by cardiovascular pathologists (JJM and WDE), blinded to the clinical information. Three histomorphologic patterns, including interstitial, vascular, and endocardial, were independently recorded. Two distinct morphologies of amyloid deposition (or a combination thereof) were also recognized (Fig. 1): (1) “filamentous” amyloid deposits, that stained deeper with a SAB stain, and had an unusual thread-like appearance on H&E; (2) “nonfilamentous” deposits, characterized by the amyloid deposits of usual character that appeared waxy, nodular, and homogenous on H&E and SAB; and (3) mixed pattern, with co-deposition of filamentous and nonfilamentous forms in the same specimen.
Nonfilamentous and filamentous types of atrial amyloid. Nonfilamentous amyloid exhibits a homogenous and dense staining pattern on both (a) hematoxylin & eosin and (c) sulfated Alcian blue staining; whereas filamentous amyloid appears more thread-like and darkly staining on (b) hematoxylin & eosin and (d) sulfated Alcian blue staining (original magnification, ×200)
The extent of interstitial, vascular, and endocardial amyloid deposition was evaluated semiquantitatively at low power (original magnification, ×4). Interstitial deposition was graded as follows: 0 = none; 1+ = mild, focal (<5% of myocardial interstitium involved); 2+ = moderate, multifocal (≥5% but <50% of myocardial interstitium); 3+ = severe, extensive (≥50% of myocardial interstitium). When present, the severity of vascular deposition was graded as being nonobstructive (<75% reduction in the luminal cross-sectional area) or obstructive (≥75% reduction in the luminal cross-sectional area). Endocardial deposition was graded as follows: 0 = none; 1+ = focal or multifocal; 2+ = diffuse and confluent. In “mixed” cases, location and extent of amyloid depositions of both morphological varieties were recorded separately. For cases with both appendages available, the appendage with the highest total grade was used.
Amyloid typing
A representative subset of 30 appendages demonstrating amyloid deposits from 28 patients was selected for amyloid typing by liquid chromatography tandem mass spectrometry (LC-MS/MS) (Fig. 2). These included isolated left atrial appendages (LAA) from 23 patients, isolated right atrial appendages (RAA) from 3 patients, and bilateral atrial appendages from 2 patients. Of the 30 appendages, 15 (9 LAA, 3 RAA, both appendages in one case) demonstrated filamentous deposits; 1 (LAA) nonfilamentous; and 14 (12 LAA, both appendages from 1) were mixed.
For each case, a representative paraffin block, containing the atrial appendage tissue involved by amyloidosis, was procured. Thick (10 µm) sections were stained with Congo red, and areas of amyloid were laser microdissected. Mixed cases underwent differential microdissection for each morphologic amyloid type. Amyloid plaques then underwent trypsin digestion and analysis on a Thermo Finningan LTQ Orbitrap mass spectrometer (Thermo Electon, Bremen, Germany) coupled to an Eksingent nonLC-2D HPLC system (Eksigent, Dublin, CA, USA) as described previously [12]. Resulting tandem mass spectra were matched to the human UniProt protein sequence database using three different search engines [13]. Peptide matches were assembled into protein identifications using Scaffold software [13]. Proteins with at least one confident (probability ≥ 0.9) unique peptide identification and more than five spectral matches were considered for interpretation.
Ultrastructural analysis
Ultrastructural analysis was performed on two appendages with amyloidosis (one LAA with filamentous; one LAA with nonfilamentous deposits) from two different patients. The areas of interest were extracted, deparaffinized, and post-fixed in glutaraldehyde prior to plastic embedding, sectioning, and evaluation.
Clinical features, preoperative and postoperative atrial arrhythmias
A retrospective review of patient records was performed to abstract salient clinical conditions, including the presence of systemic hypertension, history of stroke/transient ischemic attack (TIA), and coronary artery disease (CAD).
All available modalities of electrocardiogram (ECG), including 12-lead ECG, 24-h Holter and real time ambulatory ECG monitors [earliest available through last follow-up date (January 28, 2017)] were manually reviewed by an electrophysiologist (either DP. or SJA.) blinded to amyloid status of the cases.
Preoperative and post-Maze (>3 months after Maze) atrial rhythm status for each patient was recorded as follows: sinus rhythm (SR) or atrial arrhythmia (AA) (namely AF), typical or atypical atrial flutter (typAFL or atypAFL) and atrial tachycardia (AT). When a patient presented with episodes of different arrhythmias, each patient was cataloged with a rhythm status in the following preferential order: AF > atypAFL > typAFL > AT. Patients with indeterminate atrial rhythm status due to paucity of data or secondary to known reversible cause were excluded from the statistical analysis.
Where available, the pattern of preoperative AF was classified and recorded according to relevant guidelines [10, 14, 15]. Paroxysmal AF was defined as recurrent (≥2) AF episodes terminating spontaneously or with intervention within 7 days of onset; when sustained beyond 7 days, AF was designated as persistent. Long-standing AF patterns (defined as sustained AF episode lasting >3 years) were considered persistent AF. Patients with mixed episodes of paroxysmal and persistent AF were labeled with the most frequent presentation.
Survival analysis
Each patient’s vital status was checked through Accurint® (LexisNexis®) on November 19, 2018. Date of death was recorded for all deceased patients.
Statistical analysis
JMP 10.0.0 (SAS, Carey, North Carolina) and Graphpad Prism version 8.0.2 (San Diego, California) software programs were used to analyze the data. Categorical variables are shown as numbers (n) and percentages (%). Continuous variables are expressed as means ± SD, unless indicated otherwise. Continuous variables were assessed on the basis of ANOVA followed by the tail-Mann–Whitney test, and all categorical variables were compared by χ2 analysis. A p value of <0.05 was considered statistically significant. Survival from the time of surgery was calculated using Kaplan–Meier survival curves. Comparison of survival curves was done with log-rank test. Cox proportional hazards model was utilized to assess the effect of clinical variables on survival.
Results
Cohort demographics and prevalence of amyloidosis
Three-hundred eighty-three atrial appendages (LAA from 267 patients, RAA from 40, and both appendages from 38) were surgically resected from 345 patients (mean age ± SD, 69 ± 12 years; range, 26–92; 60% men) (Table 1 and Fig. 2). Amyloid was present in 173 (45%) appendages from 160 (46%) patients. In cases wherein only the LAA was resected, amyloidosis was observed in 129 of 267 (48%) patients. Unilaterally resected RAAs were involved in 10 (25%) cases. Bilateral resection revealed amyloid in 21 (55%) cases, including bilateral amyloid deposition in 13 (34%), isolated LAA involvement in 8 (21%), and isolated RAA involvement in none.
Patients with amyloidosis had a higher average age at resection compared with those without amyloid (74 ± 9 years vs. 65 ± 13 years; analysis of variance p < 0.0001); with a linear relationship between age (by decade) and atrial amyloidosis (p < 0.001). The youngest individual with amyloid was 31-years-old, and had marked (grade 3) filamentous deposition within her left atrium, coinciding with a 6.5-year-long history of AF.
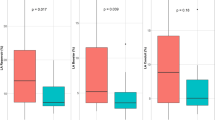
Women were also more likely to have atrial appendages involved by amyloidosis (multivariate p = 0.0161, adjusted for age), and had a higher predilection for AANF-type amyloid (Fig. 3). Although women were older than men at the time of surgery (71 ± 11 vs. 68 ± 12, ANOVA p = 0.0085), amyloidosis was directly related to age irrespective of patient sex (multivariate p < 0.0001, adjusted for sex) (Fig. 4).
Histomorphological analysis
Histologic sections of 173 appendages from the 160 patients with atrial amyloid, showed two distinct morphologies of amyloid: filamentous and nonfilamentous (Fig. 5) (as confirmed by green birefringence of Congo red-stained tissue under cross-polarized light). These morphologies were observed in all patterns of deposition (e.g. interstitial, vascular, or endocardial) and did not show morphology-specific predilection. Filamentous amyloid deposits were identified in 158 (91%) appendages from 146 of 160 (91%) patients (both appendages in 12 patients, LAA in 124, and RAA in 10). Isolated nonfilamentous deposits were seen in a single (0.6%) appendage (LAA). A mixed pattern of both filamentous and nonfilamentous amyloid was observed in 14 (8%) appendages from 13 (8%) patients (LAA in 12 patients and both appendages in 1 patient) (Fig. 6).
Mixed nonfilamentous and filamentous amyloid deposition. The morphologic differences between the two forms of amyloid are readily seen in deposits that reside adjacent to one another. Differential microdissection showed the nonfilamentous amyloid (left) to type as ATTR and the filamentous amyloid (right) to type as AANF
Vascular deposition of amyloid was prevalent and observed nearly universally in those patients in which amyloid was identified (157 of 160 (98%) cases), irrespective of type (Fig. 7). However, the deposits were rarely obstructive (3 of the 157 with vascular amyloid; 2%).
Endocardial deposition was also commonly observed, having been identified in 105 of 160 (66%) cases. However, the deposition was diffuse and confluent in only one case.
Correlation of histomorphologies and amyloid type by LC-MS/MS
When amyloid deposits were typed by LC-MS/MS, those with filamentous morphology all represented atrial natriuretic factor-type amyloid (AANF), and those with nonfilamentous morphology all represented transthyretin-type amyloid (ATTR) (χ2 p < 0.001).
Ultrastructural analysis
Regardless of their light microscopic morphology (filamentous or nonfilamentous), amyloid deposits showed 7.5–10 nm non-branching fibrils typical of amyloid, with no observed ultrastructural difference (Fig. 8).
Clinical features, preoperative, and post-Maze AAs
Surgical indications for the cohort are listed in Table 2. The reasons for atrial appendage resection were either protection from thromboembolism or incidental during cardiopulmonary bypass cannulation. Those patients for which the atrial appendage was resected for thromboembolic protection were more likely to have amyloid than those undergoing incidental cannulation (51% vs. 27%, p = 0.0090).
Fifty-four (16%) of the 345 patients had a documented history of stroke or TIA. Thirty-three (61%) of these had amyloidosis (vs. 21 (39%) without) [χ2 p = 0.0181; odds ratio (OR), 2.03; 95% confidence interval (CI), 1.1–3.7; p = 0.0196]. When adjusted for age using logistic regression analysis, the correlation between amyloidosis and stroke/TIA was still significant (OR, 2.7; 95% CI, 1.5–5; p = 0.0013).
Amyloid was identified in 128 (74%) of the 257 patients with a history of systemic hypertension (χ2 p = 0.0291; OR = 2.3152). CAD was present in 253 (73%) patients, 124 (49%) of which had amyloidosis (χ2 p = 0.1036).
Preoperative AAs and amyloidosis
Preoperative rhythm status was available for 335 (97%) patients. Of these, 42 (13%) were in SR, while 293 (87%) had AA, including 271 (92%) with AF, 16 (6%) with typAFL, and 6 (2%) with AT). Patients with amyloidosis were more likely to have AA than SR (147 vs. 12, respectively) compared with patients without amyloidosis (146 vs. 30) (χ2 p = 0.0088; OR, 2.51; 95% CI, 1.2–5.1; p = 0.0160) (Table 3).
Among 271 patients with preoperative AF, the pattern of AF was known for 252 (93%); 178 (71%) had persistent/long-term persistent AF, while 74 (29%) had paroxysmal AF. Patients with amyloidosis were more likely to have persistent/long-term persistent AF than paroxysmal AF (106 vs. 28, respectively), compared with patients without amyloid (72 vs. 46, respectively) (χ2 p = 0.0017; OR, 2.41; 95% CI, 1.4–4.2; p = 0.0019). However, the pattern of preoperative AF was statistically insignificant between cases with filamentous versus nonfilamentous amyloidosis (p = 0.2741).
The extent of amyloid deposition was more pronounced in patients with a history of stroke/TIA than in those without (unadjusted p = 0.0138; sex-adjusted p = 0.0067). However, no statistically significant correlation was observed between extent of amyloid deposition and preoperative arrhythmia status.
Post-Maze recurrence of AAs and amyloidosis
Among the total cohort of 345 patients, 247 (71.6%) underwent a Maze procedure, including 34 cases of cut-and-sew technique, 114 cryoablations, 94 radiofrequency ablations, 3 cut-and-sew and cryoablation combined, and 2 cryoablation and radiofrequency ablation combined.
Post-surgical atrial rhythm data were available for 123 patients, >3 months after their operation (Table 3). AA was more likely to recur in the amyloid-positive group (AA recurrence vs. no recurrence, 45 vs. 12) compared with the amyloid-negative group (AA recurrence vs. no recurrence, 37 vs. 29) (χ2 p = 0.0073; OR, 2.93; 95% CI, 1.3–6.5; p = 0.0083). Similar trends in AF recurrence; however, the statistical significance was lost after adjusting for age and sex.
There was no statistically significant correlation between the severity of amyloid deposition and >3 months post-Maze recurrence of arrhythmias of any type.
Survival analysis
Three patients (of 345) were excluded from the survival analysis, one due to unknown vital status, and two due to perioperative death (defined as death within 2-week of the surgery). Among the remaining 342 patients, the median follow-up time was 2440 days [interquartile range (IQR): 1008] in the amyloid-negative group and 2402 days (IQR: 947) in the amyloid-positive group.
Cox proportional-hazards survival analysis adjusting for age at surgery and sex of patient resulted in no survival differences when analyzed as following: (a) amyloid positive vs. amyloid negative (p = 0.9635); (b) AANF vs. amyloid-negative (p = 0.8463); (c) ATTR + Mixed vs. amyloid-negative (p = 0.1935); and (d) AANF vs. ATTR + Mixed (p = 0.0977). Age at surgery was the most significant factor for predicting the survival.
There was no statistical correlation between the extent of amyloid deposition and mortality (p > 0.05 for all).
Discussion
Historical background of atrial amyloidosis
Age-related (“senile”) cardiac amyloid was first described by Soyka in 1876 [7]. A century elapsed before Westermark et al. [16] showed that it includes two types of amyloid. The first, isolated atrial amyloid (IAA), appears at an earlier age, is limited to the atria, and has its major subunit protein derived from α-ANF synthesized predominately by atrial myocytes [17]. The second type, composed of ATTR (transthyretin/prealbumin), has more notoriety due to its widespread cardiac involvement and more overt clinical manifestations.
In early studies, it was differentiated from IAA based on the presence of the amino acid tryptophan using somewhat nondiscriminatory methods [16]. Newer generation techniques, such as LC-MS/MS, now enable us to proteomically differentiate the two forms of amyloid with high accuracy and precision—even when present in the same specimen.
There is an increasing appreciation for the importance of detecting ATTR-type amyloid in patients, given that overall survival is poor following the diagnosis, with a median survival of only 3.6 years [18]. Importantly, however, new classes of pharmaceuticals are available that help to stabilize the protein and reduce all-cause mortality while improving the quality of life [19, 20]. This puts enormous pressure on clinicians and pathologists alike to not only identify amyloid but also to accurately determine its type so specific therapy can be provided.
The significance of IAA (AANF-type amyloid) is less clear. Recently, Bhakhri et al. [21] reported finding IAA in ~16% of surgically resected atrial appendages. Further, they found increased perioperative death and lower 1-year survival in patients with immunohistochemically detected IAA vs. those that had none.
The histomorphological and clinical differences between the two amyloid types have not been systematically studied in a routine surgical pathology setting. To our knowledge, this is the first study to evaluate the microscopic differentiation between the two amyloid types in surgically resected atrial appendages, using definitive proteomic typing and to evaluate the prognostic significance of the findings. Our results revealed four key observations.
AANF has specific histomorphology (unlike other cardiac amyloids)
While trends have been described when assessing the morphology and pattern of deposition of the different types of cardiac amyloid, they have not proven specific enough for diagnostic purposes. In the present study, the amyloid identified in atrial appendages had one of two morphologic patterns: “filamentous” and “nonfilamentous.” Importantly, both varieties meet the morphological criteria to be called amyloid, including staining characteristics (with Congo red and SAB) and ultrastructural examination.
The morphologically distinct filamentous deposits of AANF amyloid may be identified with confidence on routine H&E and SAB staining. For this reason, expensive typing methodologies need not necessarily need to be employed when only this pattern is identified.
There are sex and site-specific trends to AANF deposition
AANF deposits more commonly in women than men and more often in the left atrial appendage than the right. The left-sided predilection of AANF is curious and may be related to anatomic or physiologic factors. It is possible, for instance, that left atrial myocytes have a greater endocrine function (and thereby greater ability to produce ANF) than right-sided atrial myocytes.
The likelihood of detecting amyloid is related in part to which appendage is resected. Lower prevalences have been reported when the RAA has been solely evaluated (16%) [6]. Similarly, we observed a lower prevalence in RAA than LAA, with nearly a 2:1 ratio of LAA amyloid to RAA amyloid.
Amyloid is also more commonly found in women, indicating that women appear to be more likely to develop AANF-type amyloid than men (56% of women vs. 39% men). The reason for this is not immediately apparent, though some have proposed a sex-specific hormonal mechanisms that may explain increased ANF production in women [22]. These sex- and site-specific trends may assist the surgical pathologist in recognizing samples at “high-risk” for being involved by atrial amyloidosis.
AANF-type atrial amyloidosis is common and increases with age
Incidental discovery of amyloid within surgically resected atrial appendages is common, occurring in 46% of the presented cohort. This is consistent with previously reported literature, which also documented a prevalence of 46% [5], in which both atrial appendages were studied. The vast majority (>90%) of our cases represented AANF-type amyloid. The likelihood of finding amyloid in a surgically resected atrial appendage is also directly proportional to the age of the patient from which it came. Interestingly, we did identify a 31-year-old woman with chronic AF with AANF-type amyloid, representing the youngest patient reported with such. Notably, she did have return of her AF following surgery.
Amyloid type is predictive of clinical course
The presence of amyloidosis—irrespective of type—within surgically excised atrial appendages has relevant prognostic implications. Such patients are more likely to have experienced stroke or TIA, possibly related to their increased likelihood of having an AA preoperatively. Postoperatively, patients with atrial amyloid are more likely to experience recurrence of their AA when compared with their non-amyloid counterparts. Interestingly, the amount of amyloid did not appear to correlate with pre or postoperative arrhythmia status.
In terms of survival, individuals with AANF amyloid had similar outcomes at 1 and 9 years when compared with those individuals who did not have amyloid. This stands in contradistinction to recently described poor postoperative outcomes in those with IAA [21].
Study limitations
All patients included in our study underwent cardiac surgery; hence, our study population was a specific subset of patients with severe cardiac conditions requiring open heart surgery. Results should be interpreted within this limited patient population.
Conclusions
This study provides rational for the routine histological evaluation of surgically resected atrial appendages in the surgical laboratory. Amyloid is common within atrial appendages, and its type has significant prognostic value. Careful morphologic inspection can obviate the need for expense typing of the relatively common finding of AANF-type amyloidosis. Nevertheless, should the pathologist have question as to whether ATTR-type amyloid is present, typing is recommended owing to the type-specific therapies now available to patients.
References
Castonguay MC, Wang Y, Gerhart JL, Miller DV, Stulak JM, Edwards WD, et al. Surgical pathology of atrial appendages removed during the cox-maze procedure: a review of 86 cases (2004 to 2005) with implications for prognosis. Am J Surg Pathol. 2013;37:890–7.
Saito T, Tamura K, Uchida D, Saito T, Togashi M, Nitta T, et al. Histopathological features of the resected left atrial appendage as predictors of recurrence after surgery for atrial fibrillation in valvular heart disease. Circ J. 2007;71:70–8.
Thijssen VL, Ausma J, Liu GS, Allessie MA, van Eys GJ, Borgers M. Structural changes of atrial myocardium during chronic atrial fibrillation. Cardiovasc Pathol. 2000;9:17–28.
Wijffels MC, Kirchhof CJ, Dorland R, Allessie MA. Atrial fibrillation begets atrial fibrillation. A study in awake chronically instrumented goats. Circulation. 1995;92:1954–68.
Leone O, Boriani G, Chiappini B, Pacini D, Cenacchi G, Martin Suarez S, et al. Amyloid deposition as a cause of atrial remodelling in persistent valvular atrial fibrillation. Eur Heart J. 2004;25:1237–41.
Rocken C, Peters B, Juenemann G, et al. Atrial amyloidosis: an arrhythmogenic substrate for persistent atrial fibrillation. Circulation. 2002;106:2091–7.
Steiner I, Hajkova P. Patterns of isolated atrial amyloid: a study of 100 hearts on autopsy. Cardiovasc Pathol. 2006;15:287–90.
Cornwell GG 3rd, Murdoch WL, Kyle RA, Westermark P, Pitkanen P. Frequency and distribution of senile cardiovascular amyloid. A clinicopathologic correlation. Am J Med. 1983;75:618–23.
Hodkinson HM, Pomerance A. The clinical significance of senile cardiac amyloidosis: a prospective clinico-pathological study. Q J Med. 1977;46:381–7.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines andthe Heart Rhythm Society. Circulation. 2014;130:2071–104.
Podduturi V, Armstrong DR, Hitchcock MA, Roberts WC, Guileyardo JM. Isolated atrial amyloidosis and the importance of molecular classification. Proc (Bayl Univ Med Cent). 2013;26:387–9.
Vrana JA, Gamez JD, Madden BJ, Theis JD, Bergen HR 3rd, Dogan A. Classification of amyloidosis by laser microdissection and mass spectrometrybased proteomic analysis in clinical biopsy specimens. Blood. 2009;114:4957–9.
Theis JD, Dasari S, Vrana JA, Kurtin PJ, Dogan A. Shotgun-proteomics-based clinical testing for diagnosis and classification of amyloidosis. J Mass Spectrom. 2013;48:1067–77.
Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S, et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Europace. 2010;12:1360–420.
Fuster V, Ryden LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, et al. ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2011;123:e269–367.
Westermark P, Johansson B, Natvig JB. Senile cardiac amyloidosis: evidence of two different amyloid substances in the ageing heart. Scand J Immunol. 1979;10:303–8.
Baxter GF. The natriuretic peptides. Basic Res Cardiol. 2004;99:71–5.
Grogan M, Scott CG, Kyle RA, Zeldenrust SR, Gertz MA, Lin G, et al. Natural history of wild-type transthyretin cardiac amyloidosis and risk stratification using a novel staging system. J Am Coll Cardiol. 2016;68:1014–20.
Maurer MS, Schwartz JH, Gundapaneni B, Elliott PM, Merlini G, Waddington-Cruz M, et al. Tafamidis treatment for patients with transthyretin amyloid cardiomyopathy. N Engl J Med. 2018;379:1007–16.
Ruberg FL, Grogan M, Hanna M, Kelly JW, Maurer MS. Transthyretin amyloid cardiomyopathy: JACC state-of-the-art review. J Am Coll Cardiol. 2019;73:2872–91.
Bhakhri K, Volpi S, Gori D, Goddard M, Ali JM, De Silva R Isolated atrial amyloid: a potential contributor to morbidity and mortality following cardiac surgery. Interact Cardiovasc Thorac Surg. 2019.
Babiker FA, De Windt LJ, van Eickels M, Thijssen V, Bronsaer RJ, Grohe C, et al. 17beta-estradiol antagonizes cardiomyocyte hypertrophy by autocrine/paracrine stimulation of a guanylyl cyclase A receptor-cyclic guanosine monophosphate-dependent protein kinase pathway. Circulation. 2004;109:269–76.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fayyaz, A.U., Bois, M.C., Dasari, S. et al. Amyloidosis in surgically resected atrial appendages: a study of 345 consecutive cases with clinical implications. Mod Pathol 33, 764–774 (2020). https://doi.org/10.1038/s41379-019-0407-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-019-0407-5
This article is cited by
-
Transthyretin derived amyloid deposits in the atrium and the aortic valve: insights from multimodality evaluations and mid-term follow up
BMC Cardiovascular Disorders (2023)