Abstract
Pathological staging of primary anorectal mucosal melanoma is often performed according to the American Joint Commission on Cancer (AJCC) guidelines for cutaneous melanoma, as an anorectal melanoma-specific staging system does not exist. However, it remains unknown whether prognostic factors derived for cutaneous melanoma also stratify risk in anorectal melanoma. We retrospectively determined correlations between clinicopathological parameters and disease-specific survival in 160 patients. Patients were grouped by clinical stage at presentation (localized disease, regional or distant metastases). Cox proportional hazards regression models determined associations with disease-specific survival. We also summarized the somatic mutations identified in a subset of tumors analyzed for hotspot mutations in cancer-associated gene panels. Most of the patients were white (82%) and female (61%). The median age was 62 years. With a median follow-up of 1.63 years, median disease-specific survival was 1.75 years, and 121 patients (76%) died of anorectal melanoma. Patients presenting with regional (34%) or distant metastases (24%) had significantly shorter disease-specific survival compared to those with disease localized to the anorectum (42%). Of the 71 anorectal melanoma tumors analyzed for hotspot genetic alterations, somatic mutations involving the KIT gene (24%) were most common followed by NRAS (19%). Increasing primary tumor thickness, lymphovascular invasion, and absence of regression also correlated with shorter disease-specific survival. Primary tumor parameters correlated with shorter disease-specific survival in patients presenting with localized disease (tumor thickness) or regional metastases (tumor thickness, absence of regression, and lymphovascular invasion), but not in patients presenting with distant metastases. Grouping of patients according to a schema based on modifications of the 8th edition AJCC cutaneous melanoma staging system stratified survival in anorectal melanoma. Our findings support stage-specific associations between primary tumor parameters and disease-specific survival in anorectal melanoma. Moreover, the AJCC cutaneous melanoma staging system and minor modifications of it predicted survival among anorectal melanoma patients.
Similar content being viewed by others
Introduction
Primary anorectal melanoma accounts for ~1.5% of all melanomas and 16.5% of all mucosal melanomas [1, 2], and represents the second most common subtype of mucosal melanoma after sinonasal. In a SEER database study of anorectal melanoma patients in the United States from 1973–2011, the annual anorectal melanoma incidence was 0.343 cases per 1 million (0.259 in men and 0.407 in women) and has steadily increased over time [2, 3]. Anorectal melanoma is an aggressive melanoma subtype with 5-year overall survival rates estimated between 14% [4] to 30% [5, 6] and an estimated median overall survival of 9–19 months [3, 7,8,9]. Among mucosal melanoma subtypes, anorectal melanoma exhibits the shortest interval to disease progression and the highest rate of metastasis [10].
Mucosal melanomas, including melanomas arising in the sinonasal, anorectal, and genitourinary mucosa, present unique clinical and pathological challenges distinct from cutaneous melanoma. Mucosal melanomas arise in non-keratinizing epithelia (squamous, columnar, or junctional) in anatomic locations less amenable to examination, commonly lack pigmentation and frequently simulate common benign processes (e.g., sinonasal polyps, hemorrhoids)—all of which compromise early detection [8, 9]. The higher density of lymphovascular structures in mucosal sites also provides greater access to, and thus, may increase the likelihood of systemic dissemination of tumor cells. Taken together, it is not surprising that mucosal melanoma patients more commonly present with regional and/or distant metastases (~35–50%) compared to only 11% of patients with cutaneous melanoma at diagnosis [11]. Surgical extirpation of mucosal melanoma can also be challenging because of the less distinctive microanatomic boundaries in mucosal sites compared to skin; and anatomic and functional constraints such as sphincter preservation impact approaches to local control. Mucosal melanomas also harbor unique molecular-genetic alterations reflecting their origin in anatomic sites protected from exposure to ultraviolet light [12,13,14]. Finally, mucosal melanomas may have lower response rates to immune checkpoint blockade therapy compared to cutaneous melanoma [3, 13, 15,16,17].
Identifying risk stratification systems that accurately reflect the unique biology of anorectal melanoma remains an important challenge. Clinical stage at presentation, as defined by Ballantyne [18], is one predictor of survival in anorectal melanoma, and in previous studies, patients with localized disease (i.e., restricted to the anorectum) had longer survival compared to those that presented with regional and/or distant metastases [2, 8, 10, 18,19,20,21]. However, the Ballantyne system lacks granularity, particularly regarding risk stratification among patients with early-stage disease. In addition, owing to the rarity of anorectal melanoma, few studies have assessed the association between discrete pathological variables of the primary tumor and clinical outcomes [22,23,24]. Further, most prior studies have grouped the various subtypes of mucosal melanoma (sinonasal, genitourinary, and anorectal) together, precluding assessment of prognostic variables that may be unique to a given subtype [10]. As such, these studies were neither designed nor sufficiently powered to determine the relative contribution of conventional prognostic factors specifically in anorectal melanoma or to consider these in the context of stage at presentation [10].
Taken together, there is a critical unmet need to delineate the clinicopathological parameters that accurately predict the biological behavior of anorectal melanoma—particularly among patients presenting with localized and regional metastatic disease. Delineation of patients at highest risk for disease progression could identify populations that might benefit from early therapeutic intervention, such as neoadjuvant therapy or entry into clinical trials. Conversely, identification of individuals at low risk for relapse could spare such patients toxicities associated with additional treatments, and support surveillance-based approaches. Thus, we retrospectively determined associations between clinicopathological parameters of primary tumor and metastatic disease and disease-specific survival in 160 patients with anorectal melanoma.
Materials and methods
Selection of cases
The study was approved by the Institutional Review Board of The University of Texas MD Anderson Cancer Center. The pathology archives were searched to identify patients with anorectal melanoma referred to MD Anderson at some point during their care, during the period from March 1986 through October 2012 (n = 254). This time period was selected in order to ensure adequate follow-up for surviving patients and to avoid the potential impact on survival due to novel (targeted/immuno-) therapies. Data collected from all patients were examined for completeness and patients were selected for inclusion in the final analyses based on the availability of both: (i) hematoxylin-eosin (H&E)-stained slides of primary tumors (for reevaluation of histologic parameters, particularly in older cases) and/or detailed pathology reports (issued by one of the coauthors) documenting histopathological parameters that included at least primary tumor thickness, ulceration status, and mitotic rate (as required for staging of cutaneous melanoma according to criteria in the 8th [25] and/or 7th [26] editions of the American Joint Commission On Cancer Staging Manuals), and (ii) carefully annotated demographic, clinical management, and follow-up data (minimum of 4 years for surviving patients). Overall, 160 patients met these criteria and were included in the final analyses. Some patients in the current study may have been included in prior reports from MD Anderson [5, 7, 27], but the overall results here reported are not duplicated.
Clinical, histopathological, and mutational data
For each patient, the following demographic/clinical data were collected: date and age at diagnosis; sex; ethnicity; anatomic location of primary tumor (rectum, located above the dentate line; anorectal junction, referring to the area of anal sinuses, valves and papillae, [i.e., the level of the dentate line]; anal canal, referring to the smooth anoderm or squamous zone located below the dentate line; and anal verge, referring to the anocutaneous junction); details of regional metastases (date of diagnosis, clinically occult or clinically evident), anatomic site, type of lymph node(s) removed (sentinel or non-sentinel), number of all lymph nodes removed and number of lymph nodes involved by metastatic melanoma, size of metastatic deposit, microanatomic location of the metastatic focus within the lymph node, and presence of extranodal extension; treatment approach, including type(s) of surgery for primary anorectal melanoma and regional lymph nodes as well as non-surgical therapies (radiation and systemic); details of distant metastases (date of diagnosis, anatomic location, and lactate dehydrogenase level at diagnosis, when available); and date and cause of death, when applicable.
H&E-stained slides of the primary tumor were reviewed/evaluated for each case by at least one dermatopathologist (PN, MTT, VGP, JLC, DI, CAT, AHD, WLW, and AJL). Discrepancies with outside diagnoses were adjudicated in a consensus conference setting with the majority opinion prevailing. The following primary tumor histopathological parameters were recorded: histologic type, tumor thickness [28] measured from top of the granular layer of squamous epithelium/columnar epithelium of colonic mucosa, or base of the ulcer to the deepest point of invasion and was categorized according to American Joint Commission on Cancer (AJCC) 8th edition pathological T-category criteria (T1: ≤1.0 mm; T2: 1.1–2.0 mm; T3: 2.1–4.0 mm; T4: >4.0 mm); level of rectal wall invasion (lamina propria, submucosa, muscularis propria, or serosa and beyond); vertical growth phase [29]; radial growth phase; mitotic rate of the invasive component [30], determined using the hot spot approach (highest number of mitotic figures in the invasive component/mm2) [31]; tumor-associated epithelial ulceration [32]; regression, defined as spontaneous partial or complete disappearance of a previously documented melanoma with associated dermal fibrosis, dilated vessels and a variable density of pigmented macrophages without evidence to suggest these changes were due to therapeutic interventions or external trauma [33]; lymphovascular invasion [34]; perineural invasion [35]; microscopic satellitosis [36]; tumor-infiltrating lymphocytes [37] (absent, non-brisk, or brisk); precursor melanocytic nevus [38]; predominant cytology (epithelioid, nevoid, spindled, or mixed); and ‘final resection margin’ status after completion of all local surgical procedures (negative, involved by in situ melanoma, or involved by invasive melanoma). As we could not consistently demonstrate an obvious histopathologic origin from either glandular or squamous mucosa, we relied on the grossly defined anatomic landmarks as defined above to designate anatomic location.
We used a modified Ballantyne staging system [18] to assign clinical stage at presentation, defined as the period up to 120 days from the date of diagnosis to include imaging studies and definitive surgical management. The patients were grouped as follows: group L (patients with localized disease confined to the anorectum), which included patients with clinically negative lymph nodes that were not evaluated pathologically (LcN0) and patients with pathologically-negative lymph nodes (LpN0); group R (patients with regional lymph node metastases), which included patients with clinically occult regional metastases (RpN+ with pathologically confirmed microscopic metastasis) and clinically evident regional metastases (RcN+ determined by clinical evaluation/imaging); and group D (patients with distant metastases).
Group L patients were classified according to four systems: (i) the AJCC 8th edition [25] for cutaneous melanoma: stage I versus stage II; (ii) AJCC 8th edition T-categories for cutaneous melanoma [39]; (iii) modified T-categories based on three groups of different tumor thickness, thin: ≤1.0 mm (T1); intermediate: >1.0 to 4.0 mm (T2/3) and thick: >4.0 mm (T4); and (iv) the tumor thickness-mitotic rate system, previously derived for stratification of primary vulvar melanomas [40] (Supplemental Table 1).
For mutational analyses, areas containing predominantly viable tumor tissue were identified on H&E-stained slides and the corresponding formalin-fixed paraffin-embedded (FFPE) tissue was manually macrodissected from mirror-image unstained slides for genomic DNA extraction, which was then analyzed for mutations by PCR-based DNA sequencing or PCR-based primer extension or pyrosequencing of select exons of specific genes (KIT, NRAS and/or BRAF) (n = 53) or PCR-based primer extension assay of 12 genes (n = 9) or next generation sequencing-based assay 46 genes (AmpliSeq Cancer Panel, Life Technologies; San Francisco, CA, USA) (n = 9) [41]. Genomic alterations, including pathogenic mutations and potential germline variants were identified and recorded.
Statistical analysis
The clinical and histopathological characteristics were summarized using descriptive statistics. Fisher’s exact test was used to determine the associations between histopathological and clinical characteristics [42]. Median follow-up period was quantified used the Kaplan–Meier estimated potential follow-up method [43]. Overall survival was defined as the time interval from the date of diagnosis to the date of death due to any cause. Disease-specific survival was defined as the time interval from the date of diagnosis to the date of death directly related to the progression of anorectal melanoma. Patients who were free of anorectal melanoma at the time of death were censored in the analysis of disease-specific survival. The survival curves for overall survival and disease-specific survival were estimated by the Kaplan–Meier method [44]. Log-rank tests were used to assess the significance of differences in disease-specific survival between groups [45]. Univariate Cox proportional hazards regression models were used to determine the association of clinicopathological characteristics with disease-specific survival or overall survival [46]. A multivariable Cox proportional hazards model for disease-specific survival was obtained by first including all covariates with p-value < 0.10 from univariate Cox models and then performing a stepwise selection using a threshold of 0.05 for the significance level of the Wald chi-square to identify covariates to be retained in the final model. The Bayesian Information Criterion was used to compare the performance of staging systems and the model with a lower value was preferred considering both model fitting and model size. No adjustments were made for the multiple comparisons. We used R version 3.1.1 (R Core Team 2014) to conduct all analyses.
Results
Demographic characteristics of primary anorectal melanoma
The clinicopathological characteristics of patients included in the analysis (n = 160) are summarized in Table 1. Overall, 61% were women and the majority (82%) were white. The median age at diagnosis was 62 years (range: 26–89 years). Tumor thickness was >4.0 mm in 118 (73.7%) patients, with a median of 6.9 mm; 141 (88.1%) tumors were ulcerated. Sixty-two tumors (38.8%) extended into the submucosa, 28 (17.5%) extended into the muscularis propria, and 18 (11.2%) extended into the serosa and beyond.
The initial diagnostic biopsy procedure was polypectomy or hemorrhoidectomy in the majority of the patients (Supplemental Fig. 1). Sixty-six of 126 patients that underwent surgical management of anorectal melanoma had their surgeries performed at MD Anderson; wide excision and regional lymph node dissection were most frequent. Ninety patients that had achieved negative margins after planned excisional surgery (Table 1), of which seven developed local recurrence. Final margins of 15 and 50 patients were positive for melanoma in situ and invasive melanoma, respectively. Adjuvant radiation therapy was administered for disease control to the primary site only (45 patients) or to the primary and regional nodal basin (23 patients) (Supplemental Fig. 2). A variety of approaches to systemic therapy were employed in the neoadjuvant and adjuvant settings (Supplemental Fig. 2).
Overall, 131 of 160 patients had died during follow-up, most (n = 121, 92.4%) due to progression of anorectal melanoma; 11 were lost to follow-up. The median follow-up of the 8 patients that were alive at their last encounter was 5.0 years (range: 0.4–20.8 years). The median overall survival was 1.8 years, and median disease-specific survival was 1.8 years (95% CI: 1.6–2.2 years) (Supplemental Fig. 4). The 5-year disease-specific survival was 22% (95% CI: 16–30%). Most patients in our cohort presented with metastatic disease at diagnosis (Table 1), including 34% with regional nodal metastases and 24% with distant metastases (irrespective of regional disease); 42% had disease confined to the anorectum.
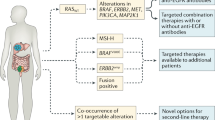
Seventy-one anorectal melanoma tumors (54 primaries, 14 regional metastases, 2 distant metastases, 1 unknown source) from patients in this cohort were evaluated for frequently reported (hotspot) mutations (Fig. 1, Table 2 and Supplemental Fig. 3). Among the genes evaluated, the frequency of mutations was 24% KIT (16 of 68 evaluated tumors, and the L576P point mutation was most common; n = 5), 19% NRAS (6 of 31; most commonly affecting codons Q61 and G12; n = 2 each), 2% BRAF (1 of 47; an activating K601E mutation).
Genomic mutations in anorectal melanoma. a, Prevalence of hotspot mutations in 71 cases of anorectal melanoma. Fractions indicate number of cases in which mutations were detected (numerator) compared to the number of cases evaluated (denominator) for each gene. Among tumors with KIT mutations, three cases had point mutations involving two different codons (black), while 13 had mutations involving only one (gray)
Associations between clinicopathological parameters and disease-specific survival
Clinical stage at presentation (Fig. 2a) significantly correlated with disease-specific survival (p < 0.001) on univariate analysis (Table 3, Fig. 2b). Patients presenting with regional metastases (median 1.81 years, hazard ratio [HR] = 1.52; p = 0.05) or distant metastases (median 1.25 years, HR = 3.24; p < 0.001) had shorter disease-specific survival compared to patients presenting with localized disease (median 2.39 years). Five-year disease-specific survival rates were 32%, 18%, and 6% for patients presenting with localized, regional, and distant disease, respectively (Supplemental Fig. 4). In addition, the following primary tumor parameters correlated with shorter disease-specific survival on univariate analysis among all patients: tumor thickness, either categorized by cut-offs in the 8th edition AJCC Staging Manual for cutaneous melanoma (p = 0.01) or when considered as a continuous variable (HR = 1.03; p < 0.001) (Fig. 3a); lymphovascular invasion (HR = 2.19; p < 0.001; Fig. 3b); perineural invasioin (HR = 1.68; p = 0.04; Fig. 3c); and final surgical margins positive for invasive melanoma (HR = 2.4; p < 0.001; Fig. 3d) (Table 2). The presence of primary tumor regression correlated with longer disease-specific survival (HR = 0.37; p = 0.01; Fig. 3e). Ulceration, mitotic rate, and level of rectal wall invasion did not correlate with disease-specific survival (Fig. 3f–h). Multivariable models (Table 3) were constructed considering only factors that were significant on univariate analysis. These showed that the presence of distant metastases (HR = 2.71; p < 0.001), increased tumor thickness (as a continuous variable) (HR = 1.02; p = 0.004), and lymphovascular invasion (HR = 1.83; p = 0.003) independently correlated with shorter disease-specific survival, while primary tumor regression independently correlated with longer disease-specific survival (HR = 0.28; p = 0.001).
Stratification of anorectal melanoma patients according to clinical stage at presentation. a Classification of patients using a modified Ballantyne clinical staging system. The patients were classified initially according to anatomic sites of involvement as having localized disease, regional metastases, or distant metastases. Patients with localized disease and regional disease were further subdivided on the basis of nodal status. b Kaplan–Meier estimates of disease-specific survival (DSS) based on clinical stage at presentation
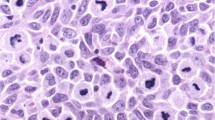
Disease-specific survival (DSS) in patients with anorectal melanoma stratified according to primary tumor histopathologic parameters. Each pair of images consists of a representative micrograph of a histopathologic feature of anorectal melanoma (left) and the respective Kaplan–Meier disease-specific survival estimates (right). a Tumor thickness, measured according to American Joint Commission on Cancer (AJCC) 8th edition cut-offs for cutaneous melanoma: T1 ≤ 1.0 mm, T2 > 1.0–2.0 mm, T3 > 2.0–4.0 mm, T4 > 4.0 mm (arrow- tumor thickness measured perpendicular to the surface along the thickest aspect of anorectal melanoma involving colonic mucosa; H&E, 20×). b Lymphovascular invasion (H&E, 400×). c Perineural invasion of nerve fibers (H&E, 400×). d Margin status, (−): negative, (+) IS: positive for in situ (IS), (+) Inv: positive for invasive melanoma; pictured: involvement of resection margin by invasive melanoma (H&E, 200×). e Histologic regression (H&E, 200×). f Tumor-associated ulceration, characterized by absence of epithelium overlying melanoma and associated fibrinous exudate on the mucosal surface (H&E, 200×). g Mitotic figures/mm2 (×4, arrows) within the invasive component (H&E, 400×). h Level of rectal wall invasion by melanoma, LP lamina propria, SM submucosa, MP muscularis propria and ≥S serosa and beyond; pictured: MP invasion (H&E, 20×). NI not identified, P present
Stage-specific associations between clinicopathological parameters and disease-specific survival
Because clinical stage was among the most robust predictors of disease-specific survival in our cohort (Fig. 2, Table 3), we next considered factors associated with disease-specific survival among patients grouped separately according to their clinical stage at presentation (Fig. 2a), to determine stage-specific associations between histopathological parameters and disease-specific survival (Table 4). This analysis also incorporated measurements of disease burden among patients with metastases, including the number of regional lymph nodes involved by melanoma; clinical detectability (by imaging studies or pathological examination) for patients with regional metastasis; and serum lactate dehydrogenase levels and the location/number of anatomic sites involved for patients with distant metastasis. Of the primary tumor pathological parameters evaluated, tumor thickness, lymphovascular invasion and regression correlated with disease-specific survival among L and among R patients (Table 4). Parameters of regional (number of nodes involved and whether these were clinically evident or occult) and distant (lactate dehydrogenase levels, site and number of organs involved) metastatic disease burden did not significantly correlate with disease-specific survival among group R and D patients, respectively.
Multivariable models (Table 5) were constructed for each stage group considering only factors that were significant on univariate analysis. Among group L patients, only tumor thickness as a continuous variable (HR = 1.08; p = 0.001) independently correlated with shorter disease-specific survival in the multivariable model. In the LcN0 subgroup, tumor thickness as a continuous variable (HR = 1.14; p = 0.03) and age ≥62 years (HR = 4.35; p = 0.02) independently correlated with shorter disease-specific survival. In the LpN0 subgroup, only lymphovascular invasion (HR = 2.97; p = 0.006) independently correlated with shorter disease-specific survival. Among group R patients, tumor thickness as a continuous variable (HR = 1.04; p = 0.001) and lymphovascular invasion (HR = 2.23; p = 0.02) independently correlated with shorter disease-specific survival, while presence of regression (HR = 0.16; p = 0.004) independently correlated with longer disease-specific survival in the multivariable model. In the RpN+subgroup, tumor thickness as a continuous variable (HR = 1.16; p = 0.01) and lymphovascular invasion (HR = 6.4; p = 0.008) independently correlated with shorter disease-specific survival. In the RcN+subgroup, ulceration independently correlated with longer disease-specific survival (HR = 0.21; p = 0.02), while perineural invasion correlated with shorter disease-specific survival (HR = 2.98; p = 0.05). Among patients who did not present with distant metastases, (groups L + R; Fig. 2b), tumor thickness as a continuous variable (HR = 1.04; p < 0.001) and lymphovascular invasion (HR = 1.85; p = 0.03) independently correlated with shorter disease-specific survival, whereas primary tumor regression (HR = 0.12; p = 0.005) independently correlated with longer disease-specific survival.
Risk stratification of patients with localized anorectal melanoma
Whereas metastatic disease at presentation strongly correlated with shorter disease-specific survival, with few other features of the primary tumor impacting disease-specific survival in this setting, patients presenting with localized anorectal melanoma showed significant variability in their disease-specific survival. Therefore, we performed additional focused analyses on group L patients (Fig. 2) to compare candidate risk models. First, we applied the 8th edition cutaneous melanoma AJCC staging system (and modifications thereof) by grouping these patients according to (i) a two-group system: stage I (T1a through T2a) versus stage II (T2b through T4b); (ii) eight individual T-sub-categories; and (iii) a modified cutaneous melanoma T-category criteria to map to 3 tumor thickness groups: ‘thin’ (T1), ‘intermediate’ (T2/3) and ‘thick’ (T4) (Supplemental Table 1). Grouping of patients according to AJCC cutaneous melanoma stage I/II delineated two groups of patients with a trend to distinct disease-specific survival, but this did not achieve statistical significance (p = 0.1) (Fig. 4a, Table 6). Although there were too few events within some of the individual T-sub-categories to assess disease-specific survival, overall survival could be stratified according to the 8T-sub-categories (Fig. 4b, Table 6), albeit with significant overlap of the Kaplan–Meier-curves (p = 0.14). In contrast, the 3-category grouping based on modified tumor thickness ranges significantly differentiated disease-specific survival among anorectal melanoma patients with localized disease (p = 0.03) (Fig. 4c, Table 6).
Risk stratification of patients with localized anorectal melanoma using T-categories. Kaplan–Meier plots of group L anorectal melanoma patients only for a disease-specific survival using American Joint Commission on Cancer (AJCC) stage (stage I: T1a to T2a; stage II: T2b to T4b), b overall survival according to the AJCC 8th-edition T-category system (T1a to T4b), c disease-specific survival using modified tumor thickness system (thin: tumor thickness ≤ 1.0 mm [T1]; intermediate: tumor thickness > 1.0–4.0 mm [T2/3]; thick: tumor thickness > 4.0 mm [T4]) and, overall survival for tumor thickness-mitotic rate system (T1: tumor thickness ≤ 2.0 mm and mitotic rate < 2/mm2; T2: tumor thickness > 2.0 mm and mitotic rate ≥ 2/mm2) [40]
We recently reported a 2-tier prognostic model (tumor thickness-mitotic rate system, Supplemental Table 1) [40] that accurately risk-stratified patients with primary vulvar melanoma according to primary tumor thickness and mitotic rate. To determine if this system also stratified risk among other mucosal melanoma subtypes, we categorized the group L anorectal melanoma patients according to the tumor thickness-mitotic rate system (Supplemental Table 1), and observed a trend towards statistical significance (p = 0.1) for overall survival (Fig. 4d, Table 6).
Since risk stratification based predominantly on tumor thickness, either as a 3-group approach or a 2-group AJCC cutaneous melanoma-based staging system approach, appeared to stratify disease-specific survival among group L patients, we evaluated their performance on the whole cohort of 160 anorectal melanoma patients in the context of the overall AJCC 8th edition cutaneous melanoma staging system (i.e., assessed together with stage III and IV anorectal melanoma patients; Fig. 5a, b). Both systems significantly stratified disease-specific survival when considering all anorectal melanoma patients together, with comparable Bayesian Information Criterion values for each (Table 7).
Comparison of risk stratification of all anorectal melanoma patients using two staging systems derived from the 8th edition American Joint Commission on Cancer (AJCC) cutaneous melanoma criteria. A, 8th edition AJCC stage system for cutaneous melanoma, B, Combination of modified tumor thickness and AJCC stage systems
Discussion
Our study represents the largest single-institution retrospective study of anorectal melanoma patients and encapsulates the disease course typical in the pre-targeted/ immunotherapy era. Mutational analyses in a subset of our patient cohort confirmed a high incidence of KIT mutations in anorectal melanoma (16 of 68 patients)—a frequency similar to prior reports [13, 14], supporting that our patient cohort appropriately reflects the biological spectrum of anorectal melanoma in the population. Our study is the first to describe stage-specific clinicopathological prognostic parameters in this disease. The 5-year disease-specific survival was 22% (95% CI: 16–30%) in our cohort, which is similar to or slightly higher than previously reported 5-year disease-specific survival [47]. Clinical stage at presentation (defined as localized disease, regional metastases, or distant metastases) [18] robustly correlated with disease-specific survival. In addition, tumor thickness, lymphovascular invasion, and regression correlated with disease-specific survival in the complete cohort. Interestingly, patients whose final resection margins were positive for melanoma in situ had disease-specific survival similar to those with negative margins (Fig. 3d). This could be due to a number of different factors. First, 13/15 (87%) patients with margins positive for melanoma in situ eventually developed metastasis, which would ultimately determine patient outcome. In addition, since immunohistochemical studies were not routinely used in the assessment of margin status, margins with more subtle involvement may have been under-called. Additional significant associations between disease-specific survival and discrete histopathological parameters were identified in a stage-specific fashion.
Among patients with disease localized to the anorectum (group L), greater tumor thickness correlated with shorter disease-specific survival. However, correlations observed between tumor thickness within the discrete subgroups were inconsistent. For example, tumor thickness independently correlated with disease-specific survival among LcN0 patients, but not among LpN0 patients. This discrepancy might be at least partially attributed to the overall small number of patients in our cohort. Moreover, it is possible that presence of lymphovascular invasion in LpN0 patients may be a more prognostically relevant variable than tumor thickness, which is also supported by the higher hazard ratio in univariate analysis (2.97 higher risk for disease-specific survival when lymphovascular invasion was present compared to 1.06 for increased tumor thickness as a continuous variable). Median tumor thickness has been reported to be greater for anorectal melanoma compared to other mucosal melanoma subtypes [10], and the relationship between tumor thickness and patient outcome in anorectal melanoma has generally confirmed worse outcome with increasing tumor thickness [5, 22, 23, 48,49,50,51,52]. However, the use of different tumor thickness cut-offs obscures direct comparison of results across the different reports. Some studies stratified anorectal melanoma according to the AJCC T-category criteria for cutaneous melanoma [23, 48], while others applied specific numerical cut-offs, including 4.00 mm [5], or 10.0 mm [52]. In addition, previous anorectal melanoma studies did not stratify patients according to clinical stage at presentation when determining relationships between primary tumor parameters. Taken together, studies on larger anorectal melanoma patient cohorts that incorporate stage at presentation are needed to define consensus criteria regarding the relationship between tumor thickness and patient survival.
Among patients with regional (lymph node) metastases (group R), greater tumor thickness and lymphovascular invasion correlated with shorter disease-specific survival (particularly among those with clinically occult regional lymph node metastases, RpN+). Our observed correlation between tumor thickness and disease-specific survival among anorectal melanoma patients with clinically occult regional lymph node metastases (RpN+) is consistent with the recent modifications to the 8th edition AJCC for cutaneous melanoma, in which T-category was integrated with the N-category to assign stage III subgroups [39]. However, the prognosis among RcN+patients is likely driven by their greater metastatic disease burden compared to RpN+ patients, and thus, the tumor thickness of the primary melanoma is possibly less critical in this disease setting. The significance of ulceration correlating with longer disease-specific survival in RcN+ patients is unclear, but may be attributable to limitations of statistical analysis on a small cohort of patients. In our anorectal melanoma cohort, regression was present in 11.3% of primary tumors and correlated with longer disease-specific survival among all patients and improved disease-specific survival among those presenting with clinically evident regional metastasis (RcN+). Although a recent meta-analysis revealed lower rates of sentinel lymph node metastasis in cutaneous melanoma with regression, the prognostic significance of primary tumor regression in cutaneous melanoma remains controversial and poorly understood [33, 53]. In our previous study of vulvar melanoma, regression was present in 25% of cases and also correlated with longer disease-specific survival [40], suggesting that an association between regression and improved patient survival may be common across anogenital mucosal melanoma subtypes. Of note, since mucosal melanoma may respond less favorably to immune checkpoint blockade therapy compared to cutaneous melanoma [3, 13, 15,16,17], the relationship between regression, the composition and density of the tumor-associated immune infiltrate, and response to immune-modulatory therapy among mucosal melanoma remains a provocative question. Analyses in contemporary patient datasets that include tumor burden, comprehensive immune profiling, and tumor mutational burden are necessary to address this systematically.
Among patients presenting with clinically evident regional or distant metastases, we found no meaningful correlations between most primary tumor parameters (including conventional high-risk features such as greater tumor thickness and lymphovascular invasion) and disease-specific survival. This is mostly similar to cutaneous melanoma in which the prognosis of these patients is largely driven by their advanced stage [54]. However, measures of regional disease burden (satellitosis, the number of nodes involved and whether these were clinically evident or occult) also did not independently correlate with disease-specific survival among patients with regional metastases. However, among the 55 patients in our cohort with regional metastases, 25% (14/55) underwent comparatively limited evaluation of the extent of their regional disease burden (without a formal pathological enumeration of the number and extent of regional lymph node burden) (Supplemental Table 2). Further, indices of distant metastatic disease burden, including lactate dehydrogenase levels and site(s) of distant metastasis (including central nervous system involvement), also did not correlate with disease-specific survival among patients with distant metastases. However, our cohort included only 38 patients presenting with distant metastases, significantly limiting the power of these analyses. Additional studies utilizing larger number of anorectal melanoma patients with regional and distant disease are likely needed to further evaluate the prognostic role of metastatic disease burden in anorectal melanoma.
Our primary goal was to optimize risk stratification of anorectal melanoma patients by integrating relevant clinicopathological variables, particularly among those presenting with localized disease. Although a formal staging system for anorectal melanoma does not exist, most studies have applied the Ballantyne clinical system [6, 10, 18, 24, 49, 55,56,57,58,59,60,61]. For anorectal melanoma patients who presented with localized disease, we found that a 3-group system based on minor modifications of the AJCC 8th edition tumor thickness cut-offs for cutaneous melanoma (thin: T1, intermediate: T2-3 and thick: T4) most robustly stratified disease-specific survival (Fig. 3, Table 6), followed by the 2-group system also based on 8th edition AJCC for cutaneous melanoma cut-offs (Stage I: T1a to T2a versus Stage II: T2b to T4b). The 3-group modified ‘tumor thickness’ system was derived based on our initial observation that although tumor thickness correlated with disease-specific survival among all anorectal melanoma patients, there was considerable overlap between T2 and T3 patients (Fig. 2a) and also predicted disease-specific survival among patients with localized anorectal melanoma. When applied to the entire cohort in conjunction with AJCC stage III and IV patients, both the ‘stage’ and the modified ‘tumor thickness’ systems accurately risk-stratified patients according to disease-specific survival, supporting the application of 8th edition AJCC cut-offs for cutaneous melanoma to patients with anorectal melanoma.
Compared to the 2-group system based on 8th edition AJCC cutaneous melanoma stage I and II and the tumor thickness-mitotic rate system, the 3-group system based on modified tumor thickness alone delineated a third group of patients that were at intermediate risk for progression (Fig. 3d). Whether this group of patients and those designated with “thick” melanomas may benefit from more frequent follow-up and/or potential adjuvant therapy(ies) compared to the “thin” melanoma patients should be explored further. Taken together, our study supports that the 8th edition AJCC staging system for cutaneous melanoma (or slight modifications of it) represents a robust approach for risk stratification among patients with anorectal melanoma, including those with localized disease. Since there were too few events within some of the individual T-sub-categories to assess disease-specific survival, only overall survival could be derived for AJCC 8th edition T-category and tumor thickness-mitotic rate system. Additional studies utilizing larger patient cohorts are required to validate these observations.
There are several limitations to our study. First, this was a retrospective study and due to the long interval of time studied (since 1986), patients in our cohort were treated with a broad array of clinical and surgical management strategies; some patients were treated elsewhere, while majority had their disease management at MD Anderson (Supplemental Fig. 2). Our study was not powered to detect differences related to the different treatment strategies used or responses to such therapies. Additionally, only 6 patients in our cohort had tumor thickness ≤1.0 mm; therefore, the data on thin melanomas is quite limited in the current study. We note that the median tumor thickness in our series (6.9 mm) was less than that reported in prior large series on anorectal melanoma (range: 7.3–12.0 mm from 286 patients) [22, 48, 49, 52], supporting that our patient cohort reflects the anorectal melanoma disease spectrum typically encountered in clinical practice. A further limitation was the mutational analyses; the assays used to identify mutations in our cohort of anorectal melanoma was derived from our routine clinical practice. Thus, the assay platforms and the number of genes evaluated varied over time and were not comprehensive. Only a few cases tested carried mutations, so we were underpowered to determine whether discrete molecular-genetic alterations correlated with patient outcome; such investigations are warranted going forward.
In conclusion, our analysis of clinicopathological parameters in 160 anorectal melanoma patients supports the prognostic significance of tumor thickness in patients with clinically localized disease, while meaningful associations were not identified in anorectal melanoma patients with distant or clinically evident regional metastases. Classification according to minor modifications (modified tumor thickness) of the AJCC 8th edition cutaneous melanoma staging system robustly stratifies patients with localized anorectal melanoma. Our study supports the rationale to evaluate these systems in additional larger cohorts of anogenital melanoma patients. To support ongoing and future planned efforts, we strongly recommend that all prognostic indicators for primary cutaneous melanoma also be recorded in the diagnosis and stratification of risk for primary anorectal melanoma.
References
Callahan A, Anderson WF, Patel S, Barnholtz-Sloan JS, Bordeaux JS, Tucker MA, et al. Epidemiology of anorectal melanoma in the United States: 1992 to 2011. Dermatol Surg. 2016;42:94–9.
Chen H, Cai Y, Liu Y, He J, Hu Y, Xiao Q, et al. Incidence, surgical treatment, and prognosis of anorectal melanoma from 1973 to 2011: a population-based SEER analysis. Medicine. 2016;95:1–8.
Taylor JP, Stem M, Yu D, Chen SY, Fang SH, Gearhart SL, et al. Treatment strategies and survival trends for anorectal melanoma: is it time for a change? World J Surg. 2019;43:1809–19.
Ragnarsson-Olding BK, Nilsson PJ, Olding LB, Nilsson BR. Primary ano-rectal malignant melanomas within a population-based national patient series in Sweden during 40 years. Acta Oncol. 2009;48:125–31.
Kelly P, Zagars GK, Cormier JN, Ross MI, Guadagnolo BA. Sphincter-sparing local excision and hypofractionated radiation therapy for anorectal melanoma: a 20-year experience. Cancer. 2011;117:4747–55.
Brady MS, Kavolius JP, Quan SH. Anorectal melanoma. A 64-year experience at Memorial Sloan-Kettering Cancer Center. Dis Colon Rectum. 1995;38:146–51.
Ross M, Pezzi C, Pezzi T, Meurer D, Hickey R, Balch C. Patterns of failure in anorectal melanoma. A guide to surgical therapy. Arch Surg. 1990;125:313–6.
Ranjith S, Muralee M, Sajeed A, Arun PM, Cherian K, Nair CK, et al. Anorectal melanoma: experience from a tertiary cancer care centre in South India. Ann R Coll Surg Engl. 2017;100:1–5.
Hicks CW, Pappou EP, Magruder JT, Gazer B, Fang S, Wick EC, et al. Clinicopathologic presentation and natural history of anorectal melanoma: a case series of 18 patients. JAMA Surg. 2014;149:608–11.
Heppt MV, Roesch A, Weide B, Gutzmer R, Meier F, Loquai C, et al. Prognostic factors and treatment outcomes in 444 patients with mucosal melanoma. Eur J Cancer. 2017;81:36–44.
Cronin KA, Lake AJ, Scott S, Sherman RL, Noone AM, Howlader N, et al. Annual report to the nation on the status of cancer, part I: National cancer statistics. Cancer. 2018;124:2785–800.
Aulmann S, Sinn HP, Penzel R, Gilks CB, Schott S, Hassel JC, et al. Comparison of molecular abnormalities in vulvar and vaginal melanomas. Mod Pathol. 2014;27:1386–93.
Santi R, Simi L, Fucci R, Paglierani M, Pepi M, Pinzani P, et al. KIT genetic alterations in anorectal melanomas. J Clin Pathol. 2015;68:130–4.
Yang HM, Hsiao SJ, Schaeffer DF, Lai C, Remotti HE, Horst D, et al. Identification of recurrent mutational events in anorectal melanoma. Mod Pathol. 2017;30:286–96.
Faure M, Rochigneux P, Olive D, Taix S, Brenot-Rossi I, Gilabert M. Hyperprogressive disease in anorectal melanoma treated by PD-1 inhibitors. Front Immunol. 2018;9:797.
Shoushtari AN, Munhoz RR, Kuk D, Ott PA, Johnson DB, Tsai KK, et al. The efficacy of anti-PD-1 agents in acral and mucosal melanoma. Cancer. 2016;122:3354–62.
Dodds TJ, Wilmott JS, Jackett LA, Lo SN, Long GV, Thompson JF, et al. Primary anorectal melanoma: clinical, immunohistology and DNA analysis of 43 cases. Pathology. 2019;51:39–45.
Ballantyne AJ. Malignant melanoma of the skin of the head and neck. Anal 405 cases Am J Surg. 1970;120:425–31.
Chang AE, Karnell LH, Menck HR. The National Cancer Data Base report on cutaneous and noncutaneous melanoma: a summary of 84,836 cases from the past decade. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer. 1998;83:1664–78.
Pessaux P, Pocard M, Elias D, Duvillard P, Avril MF, Zimmerman P, et al. Surgical management of primary anorectal melanoma. Br J Surg. 2004;91:1183–7.
Ishizone S, Koide N, Karasawa F, Akita N, Muranaka F, Uhara H, et al. Surgical treatment for anorectal malignant melanoma: report of five cases and review of 79 Japanese cases. Int J Colorectal Dis. 2008;23:1257–62.
Weyandt GH, Eggert AO, Houf M, Raulf F, Brocker EB, Becker JC. Anorectal melanoma: surgical management guidelines according to tumour thickness. Br J Cancer. 2003;89:2019–22.
Che X, Zhao DB, Wu YK, Wang CF, Cai JQ, Shao YF, et al. Anorectal malignant melanomas: retrospective experience with surgical management. World J Gastroenterol. 2011;17:534–9.
Yen CI, Chen HH, Chiang SF, Yeh CY, Chen JS, Hsieh PS, et al. Anorectal melanoma: review of 22 consecutive cases. Hepatogastroenterology. 2013;60:89–93.
Gershenwald JE, Scolyer RA, Hess KR, et al. Melanoma of the skin. In: Amin MB, et al., editors. AJCC cancer staging manual 8 edn. Switzerland: Springer; 2017. pp. 563–85.
Balch CM, Gershenwald JE, Atkins MB, Buzaid AC, Cascinelli N, Cochran AJ. Melanoma of the skin. In: Edge SB, Byrd DR, Compton CC, et al., editors. AJCC cancer staging manual, 7th edn. New York: Springer International Publishing; 2010. pp. 325–46.
Ballo MT, Gershenwald JE, Zagars GK, Lee JE, Mansfield PF, Strom EA, et al. Sphincter-sparing local excision and adjuvant radiation for anal-rectal melanoma. J Clin Oncol. 2002;20:4555–8.
Breslow A. Prognosis in cutaneous melanoma: tumor thickness as a guide to treatment. Pathol Annu. 1980;15:1–22.
Clark WH Jr., Elder DE, Dt Guerry, Braitman LE, Trock BJ, Schultz D, et al. Model predicting survival in stage I melanoma based on tumor progression. J Natl Cancer Inst. 1989;81:1893–904.
Thompson JF, Soong SJ, Balch CM, Gershenwald JE, Ding S, Coit DG, et al. Prognostic significance of mitotic rate in localized primary cutaneous melanoma: an analysis of patients in the multi-institutional American Joint Committee on Cancer melanoma staging database. J Clin Oncol. 2011;29:2199–205.
Tetzlaff MT, Curry JL, Ivan D, Wang WL, Torres-Cabala CA, Bassett RL, et al. Immunodetection of phosphohistone H3 as a surrogate of mitotic figure count and clinical outcome in cutaneous melanoma. Mod Pathol. 2013;26:1153–60.
Balch CM, Wilkerson JA, Murad TM, Soong SJ, Ingalls AL, Maddox WA. The prognostic significance of ulceration of cutaneous melanoma. Cancer. 1980;45:3012–7.
Aung PP, Nagarajan P, Prieto VG. Regression in primary cutaneous melanoma: etiopathogenesis and clinical significance. Lab Invest. 2017;97:657–68.
Kashani-Sabet M, Sagebiel RW, Ferreira CM, Nosrati M, Miller JR 3rd. Vascular involvement in the prognosis of primary cutaneous melanoma. Arch Dermatol. 2001;137:1169–73.
Baer SC, Schultz D, Synnestvedt M, Elder DE. Desmoplasia and neurotropism. Progn Var patients stage I melanoma Cancer. 1995;76:2242–7.
Kimsey TF, Cohen T, Patel A, Busam KJ, Brady MS. Microscopic satellitosis in patients with primary cutaneous melanoma: implications for nodal basin staging. Ann Surg Oncol. 2009;16:1176–83.
Schatton T, Scolyer RA, Thompson JF, Mihm MC Jr. Tumor-infiltrating lymphocytes and their significance in melanoma prognosis. Methods Mol Biol. 2014;1102:287–324.
Damsky WE, Bosenberg M. Melanocytic nevi and melanoma: unraveling a complex relationship. Oncogene. 2017;36:5771–92.
Gershenwald JE, Scolyer RA, Hess KR, Sondak VK, Long GV, Ross MI, et al. Melanoma staging: evidence-based changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67:472–92.
Nagarajan P, Curry JL, Ning J, Piao J, Torres-Cabala CA, Aung PP, et al. Tumor thickness and mitotic rate robustly predict melanoma-specific survival in patients with primary vulvar melanoma: a retrospective review of 100 cases. Clin Cancer Res. 2017;23:2093–104.
Stockman DL, Curry JL, Torres-Cabala CA, Watson IR, Siroy AE, Bassett RL, et al. Use of clinical next-generation sequencing to identify melanomas harboring SMARCB1 mutations. J Cutan Pathol. 2015;42:308–17.
Upton J. Fisher’s Exact Test. J R Stat Soc Ser A. 1991;192:395–402.
Schemper M, Smith TL. A note on quantifying follow-up in studies of failure time. Control Clin Trials. 1996;17:343–6.
Kaplan E, Meier P. Nonparametric estimator from incomplete observations. J Am Stat Assoc. 1958;53:457–81.
Harrington DP, Fleming TR. A class of rank test procedures for censored survival data. Biometrika. 1982;69:553–66.
Cox D. Regression models and life tables. J R Stat Soc: Ser B. 1972;34:187–220.
Thibault C, Sagar P, Nivatvongs S, Ilstrup DM, Wolff BG. Anorectal melanoma–an incurable disease? Dis Colon Rectum. 1997;40:661–8.
Bello DM, Smyth E, Perez D, Khan S, Temple LK, Ariyan CE, et al. Anal versus rectal melanoma: does site of origin predict outcome? Dis Colon Rectum. 2013;56:150–7.
Roumen RM. Anorectal melanoma in The Netherlands: a report of 63 patients. Eur J Surg Oncol. 1996;22:598–601.
Wanebo HJ, Woodruff JM, Farr GH, Quan SH. Anorectal melanoma. Cancer. 1981;47:1891–900.
Row D, Weiser MR. Anorectal melanoma. Clin Colon Rectal Surg. 2009;22:120–6.
Yeh JJ, Shia J, Hwu WJ, Busam KJ, Paty PB, Guillem JG, et al. The role of abdominoperineal resection as surgical therapy for anorectal melanoma. Ann Surg. 2006;244:1012–7.
Ribero S, Gualano MR, Osella-Abate S, Scaioli G, Bert F, Sanlorenzo M, et al. Association of histologic regression in primary melanoma with sentinel lymph node status: a systematic review and meta-analysis. JAMA Dermatol. 2015;151:1301–7.
Balch CM, Gershenwald JE, Soong SJ, Thompson JF, Ding S, Byrd DR, et al. Multivariate analysis of prognostic factors among 2,313 patients with stage III melanoma: comparison of nodal micrometastases versus macrometastases. J Clin Oncol. 2010;28:2452–9.
Cheung MC, Perez EA, Molina MA, Jin X, Gutierrez JC, Franceschi D, et al. Defining the role of surgery for primary gastrointestinal tract melanoma. J Gastrointest Surg. 2008;12:731–8.
Falch C, Stojadinovic A, Hann-von-Weyhern C, Protic M, Nissan A, Faries MB, et al. Anorectal malignant melanoma: extensive 45-year review and proposal for a novel staging classification. J Am Coll Surg. 2013;217:324–35.
Nilsson PJ, Ragnarsson-Olding BK. Importance of clear resection margins in anorectal malignant melanoma. Br J Surg. 2010;97:98–103.
Podnos YD, Tsai NC, Smith D, Ellenhorn JD. Factors affecting survival in patients with anal melanoma. Am Surg. 2006;72:917–20.
Ramakrishnan AS, Mahajan V, Kannan R. Optimizing local control in anorectal melanoma. Indian J Cancer. 2008;45:13–9.
Zhou HT, Zhou ZX, Zhang HZ, Bi JJ, Zhao P. Wide local excision could be considered as the initial treatment of primary anorectal malignant melanoma. Chin Med J (Engl). 2010;123:585–8.
Ren M, Lu Y, Lv J, Shen X, Kong J, Dai B, et al. Prognostic factors in primary anorectal melanoma: a Clinicopathologic study of 60 cases in China. Hum Pathol. 2018;79:77–85.
Acknowledgements
We thank Ms. Kim Anh-Vu and Ms. Stephanie Deming for their excellent assistance in preparing the figures and medical editing, respectively.
Funding
This publication is based on research supported by the Melanoma Research Alliance to PN (# 570806), from 2T32CA00966-24 to MAD, and the Groningen Melanoma and Sarcoma Foundation to LEN.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
MIR reports receiving speakers’ bureau honoraria from Amgen Inc., Merck, and Provectus Biopharmaceuticals and is a consultant/advisory board member for Amgen Inc., GlaxoSmithKline, and Merck. JEG has served as a consultant or advisory board member for Merck, Bristol-Myers Squibb, Novartis, Syndax, and Castle Biosciences, unrelated to the content of this manuscript. MTT is a consultant/advisory board member for Novartis LLC, Myriad Genetics, and Seattle Genetics. VGP is a consultant for Myriad Genetics. MAD is an advisory board member for BMS, Novartis, Roche/Genentech, Sanofi-Aventis, Vaccinex, Array and Syndax; a consultant for Nanostring; and PI of research grants to The University of Texas MD Anderson Cancer Center from BMS, Roche/Genentech, Sanofi-Aventis, Merck, Oncothyreon. The remaining authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Nagarajan, P., Piao, J., Ning, J. et al. Prognostic model for patient survival in primary anorectal mucosal melanoma: stage at presentation determines relevance of histopathologic features. Mod Pathol 33, 496–513 (2020). https://doi.org/10.1038/s41379-019-0340-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-019-0340-7
This article is cited by
-
Anorektales malignes Melanom
Die Dermatologie (2024)
-
Treatment outcomes and prognostic factors in 47 patients with primary anorectal malignant melanoma in the immune therapy era
Journal of Cancer Research and Clinical Oncology (2023)
-
Genetic alteration of Chinese patients with rectal mucosal melanoma
BMC Cancer (2021)
-
Distribution pattern of tumor infiltrating lymphocytes and tumor microenvironment composition as prognostic indicators in anorectal malignant melanoma
Modern Pathology (2021)