Abstract
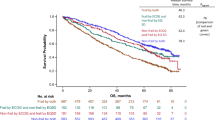
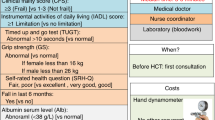
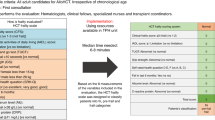
The frailty index (FI) is based on the principle that the more deficits an individual has, the greater their risk of adverse outcomes. It is expressed as a ratio of the number of deficits present to the total number of deficits considered. We developed an MDS-specific FI using a prospective MDS registry and assessed its ability to add prognostic power to conventional prognostic scores in MDS. The 42 deficits included in this FI included measurements of physical performance, comorbidities, laboratory values, instrumental activities of daily living, quality of life and performance status. Of 644 patients, 440 were eligible for FI calculation. The median FI score was 0.25 (range 0.05–0.67), correlated with age and IPSS/IPSS-R risk scores and discriminated overall survival. With a follow-up of 20 months, survival was 27 months (95% CI 24–30.4). By multivariate analysis, age >70, FI, transfusion dependence, and IPSS were significant covariates associated with OS. The incremental discrimination improvement of the frailty index was 37%. We derived a prognostic score with five risk groups and distinct survivals ranging from 7.4 months to not yet reached. If externally validated, the MDS-FI could be used as a tool to refine the risk stratification of current clinical prognostication models.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Ma X, Does M, Raza A, Mayne ST. Myelodysplastic syndromes: incidence and survival in the United States. Cancer. 2007;109:1536–42.
Klepin HD, Rao AV, Pardee TS. Acute myeloid leukemia and myelodysplastic syndromes in older adults. J Clin Oncol J Am Soc Clin Oncol. 2014;32:2541–52.
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89:2079–88.
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Solé F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120:2454–65.
Bejar R, Papaemmanuil E, Haferlach T, Garcia-Manero G, Maciejewski JP, Sekeres MA, et al. Somatic mutations in MDS patients are associated with clinical features and predict prognosis independent of the IPSS-R: analysis of combined datasets from the International Working Group for Prognosis in MDS-Molecular Committee. Blood. 2015;126:907.
Nazha A, Al-Issa K, Hamilton BK, Radivoyevitch T, Gerds AT, Mukherjee S, et al. Adding molecular data to prognostic models can improve predictive power in treated patients with myelodysplastic syndromes. Leukemia. 2017;31:2848–50.
Buckstein R, Wells RA, Zhu N, Leitch HA, Nevill TJ, Yee KWL, et al. Patient-related factors independently impact overall survival in patients with myelodysplastic syndromes: an MDS-CAN prospective study. Br J Haematol. 2016;174:88–101.
Handforth C, Clegg A, Young C, Simpkins S, Seymour MT, Selby PJ, et al. The prevalence and outcomes of frailty in older cancer patients: a systematic review. Ann Oncol J Eur Soc Med Oncol. 2015;26:1091–101.
Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. Sci World J. 2001;1:323–36.
Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatr. 2008;8:24.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ Can Med Assoc J J Assoc Med Can. 2005;173:489–95.
Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. 2007;62:722–7.
Bohannon RW, Peolsson A, Massy-Westropp N, Desrosiers J, Bear-Lehman J. Reference values for adult grip strength measured with a Jamar dynamometer: a descriptive meta-analysis. Physiotherapy. 2006;92:11–5.
Rantanen T, Volpato S, Ferrucci L, Heikkinen E, Fried LP, Guralnik JM. Handgrip strength and cause-specific and total mortality in older disabled women: exploring the mechanism. J Am Geriatr Soc. 2003;51:636–41.
Csuka M, McCarty DJ. Simple method for measurement of lower extremity muscle strength. Am J Med. 1985;78:77–81.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86.
Johnson JA, Coons SJ, Ergo A, Szava-Kovats G. Valuation of EuroQOL (EQ-5D) health states in an adult US sample. PharmacoEconomics. 1998;13:421–33.
Brooks R. EuroQol: the current state of play. Health Policy Amst Neth. 1996;37:53–72.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–76.
Hjermstad MJ, Fayers PM, Bjordal K, Kaasa S. Using reference data on quality of life-the importance of adjusting for age and gender, exemplified by the EORTC QLQ-C30 (+3). Eur J Cancer Oxf Engl 1990. 1998;34:1381–9.
Bruera E, Sala R, Rico MA, Moyano J, Centeno C, Willey J, et al. Effects of parenteral hydration in terminally ill cancer patients: a preliminary study. J Clin Oncol J Am Soc Clin Oncol. 2005;23:2366–71.
Berger AM, Mooney K, Alvarez-Perez A, Breitbart WS, Carpenter KM, Cella D, et al. Cancer-Related Fatigue, Version 2.2015. J Natl Compr Cancer Netw. 2015;13:1012–39.
Fritz S, Lusardi M. White paper: ‘walking speed: the sixth vital sign’. J Geriatr Phys Ther 2001. 2009;32:46–9.
Della Porta MG, Malcovati L. Clinical relevance of extra-hematologic comorbidity in the management of patients with myelodysplastic syndrome. Haematologica. 2009;94:602–6.
Chambless LE, Cummiskey CP, Cui G. Several methods to assess improvement in risk prediction models: extension to survival analysis. Stat Med. 2011;30:22–38.
Uno H, Tian L, Cai T, Kohane IS, Wei LJ. A unified inference procedure for a class of measures to assess improvement in risk prediction systems with survival data. Stat Med. 2013;32:2430–42.
Zipperer E, Pelz D, Nachtkamp K, Kuendgen A, Strupp C, Gattermann N, et al. The hematopoietic stem cell transplantation comorbidity index is of prognostic relevance for patients with myelodysplastic syndrome. Haematologica. 2009;94:729–32.
Della Porta MG, Malcovati L, Strupp C, Ambaglio I, Kuendgen A, Zipperer E, et al. Risk stratification based on both disease status and extra-hematologic comorbidities in patients with myelodysplastic syndrome. Haematologica. 2011;96:441–9.
Nazha A, Hu Z-H, Wang T, Hamilton BK, Majhail NS, Lindsley RC, et al. A personalized prediction model for outcomes after allogeneic hematopoietic stem cell transplant in patients with myelodysplastic syndromes: on behalf of the CIBMTR Chronic Leukemia Committee. Blood. 2018;132:206.
Fega KR, Abel GA, Motyckova G, Sherman AE, DeAngelo DJ, Steensma DP, et al. Non-hematologic predictors of mortality improve the prognostic value of the international prognostic scoring system for MDS in older adults. J Geriatr Oncol. 2015;6:288–98.
Sevindik OG, Guc Z, Kahraman S, Medeni Solmaz S, Katgi A, Acar C, et al. Hypoalbuminemia is a surrogate biomarker of poor prognosis in myelodysplastic syndrome even when adjusting for comorbidities. Leuk Lymphoma. 2015;56:2552–5.
Acknowledgements
The authors thank Celgene Canada and Crashley estate for national MDS financial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The national Canadian registry is financially supported by Celgene and Otsuka. RA.: Sponsored talks—Alexion. MMK: Consultant—Seattle Genetics (brentuximab vedotin), Honoraria—Novartis, Scientific Advisory Board—Janssen, Shire, Hoffman-La Roche, Sanofi Genzyme, Celgene. BL: Medical advisory boards and Speaker Bureau—Celgene, Pfizer, Novartis, AMGEN, Astellas, Otsuka, Jazz, Abbvie. MS: Advisory boards—Jazz, Pfizer, Novartis, Astellas, Celgene. HAL: Advisory boards, honoraria, research funding—Abbvie, Alexion, Celgene, Novartis, Advisory boards, honoraria—Otsuka. ESt-H: Advisory boards—BMS, Amgen, Celgene, Teva, Novartis, Speaker honoratrium—BMS, Sanofi, Novartis. NF: Research support—Boehringer Ingelheim, Roche, Pfizer, Merck, Honoraria—Roche, Novartis, Bristol Myers Squibb, Celgene, Pfizer, Scientific Advisory Board—Novartis, Pfizer, Lundbeck, Celgene, Janssen, Sanofi, Alexion, Roche, Ipsen, Takeda, Merck, Amgen, Bristol Myers Squibb, Astra Zeneca. AS: Advisory boards: Amgen, Janssen, Abbvie, Celgene, Sponsored talks—Janssen. KY: Research funding—Astex, Hoffman La Roche, MedImmune, Merck, Millenium, Roche/Genentech, Honoraria—Novartis, Pfizer, Board of Directors or advisory committees: Astellas, Celgene, Novartis, Pfizer, Takeda. JS: Advisory boards—Celgene, Novartis, Pfizer, Astellas, Abbvie, Amgen, speaking fees—Teva, Celgene, travel support—Pfizer. TN: Ad boards and Sponsored talks—Celgene, Alexion, Novartis, Ad boards—Paladin Labs, Otsuka. VB: Industry Research Funding—Gilead, Janssen, Roche, Ad boards—Abbvie, Astra Zeneca, Janssen, Gilead, Roche, Sponsored talk -CAPhO Abbvie, Academic Research Support—CIHR, LLSC, Research Manitoba and CancerCare Manitoba Foundation, Licensing Fees—BIOGEN and The Dana-Farber Cancer Institute. RB: Research funding support and honoraria for advisory board panels—Celgene, Research funding support—Otsuka. All other authors: no disclosures.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Starkman, R., Alibhai, S., Wells, R.A. et al. An MDS-specific frailty index based on cumulative deficits adds independent prognostic information to clinical prognostic scoring. Leukemia 34, 1394–1406 (2020). https://doi.org/10.1038/s41375-019-0666-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-019-0666-7