Abstract
Transient receptor ion channels have emerged as immensely important channels/receptors in diverse physiological and pathological responses. Of particular interest is the transient receptor potential channel subfamily V member 4 (TRPV4), which is a polymodal, nonselective, calcium-permeant cation channel, and is activated by both endogenous and exogenous stimuli. Both neuronal and nonneuronal cells express functional TRPV4, which is responsive to a variety of biochemical and biomechanical stimuli. Emerging discoveries have advanced our understanding of the role of macrophage TRPV4 in numerous inflammatory diseases. In lung injury, TRPV4 mediates macrophage phagocytosis, secretion of pro-resolution cytokines, and generation of reactive oxygen species. TRPV4 regulates lipid-laden macrophage foam cell formation, the hallmark of atheroinflammatory conditions, in response to matrix stiffness and lipopolysaccharide stimulation. Accumulating data also point to a role of macrophage TRPV4 in the pathogenesis of the foreign body response, a chronic inflammatory condition, through the formation of foreign body giant cells. Deletion of TRPV4 in macrophages suppresses the allergic and nonallergic itch in a mouse model, suggesting a role of TRPV4 in skin disease. Here, we discuss the current understanding of the role of macrophage TRPV4 in various inflammatory conditions.
Similar content being viewed by others
Introduction
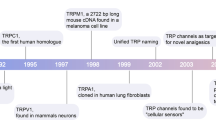
Transient receptor potential vanilloid type 4 (TRPV4) ion channels are nonselective, mechanosensitive, transmembrane Ca2+-permeable cation channels that are ubiquitously expressed in numerous cell types including macrophages [1,2,3,4,5,6,7,8,9,10,11,12,13,14]. TRPV4 channels are activated by a diverse array of biochemical and biomechanical stimuli including mechanical deformation [15,16,17], osmotic stimuli [18,19,20], heat [21,22,23,24], and by exogenous or endogenous chemical stimuli [6, 25,26,27,28]. TRPV4 is associated with numerous physiological functions such as osmolarity sensing in kidneys, sheer-stress sensing in arteries, neurological responses, and the regulation of osteogenesis [1, 29,30,31,32]. In mice, absence of TRPV4 is linked to altered pressure/vasodilatory responses, osmosensing, sensory and motor neuropathies, and the development of fibrosis in lung, skin, and cornea [29,30,31,32,33,34].
Various biochemical factors including cytokines, chemokines, modified low-density lipoprotein (LDL), and bacterial lipopolysaccharide (LPS) are active in eliciting macrophage-mediated inflammatory responses [10, 35,36,37,38,39,40,41,42,43,44]. Emerging reports from our laboratory and others have shown that critical proinflammatory macrophage responses such as phagocytosis, migration, foam cell formation, expression of inflammatory proteins, and proliferation are sensitive to changes in stiffness of their surrounding matrix [10, 36,37,38,39,40,41,42,43]. Therefore, it is important to identify the mechanosensing plasma membrane macrophage receptor/channel by which biomechanical signals are transduced and propagated into cells to drive the generation of inflammatory and other cellular responses. Since TRPV4 is a mechanosensitive channel, and is activated by both biochemical and biomechanical stimuli, it was hypothesized that under certain pathophysiological conditions macrophage TRPV4 may act as a proinflammatory molecule. Intriguingly, emerging data from our laboratory and others have shown that the macrophage TRPV4 is involved in a variety of inflammatory diseases including acute lung injury/acute respiratory disease syndrome, atherosclerosis, foreign body response (FBR), skin disease, and fibrosis [10, 30, 34, 41, 43, 45,46,47,48,49,50]. Although, the precise mechanism by which TRPV4 orchestrates the pathophysiology of these diseases is not fully understood, these studies suggest that TRPV4 plays a critical role in regulating various inflammatory responses like cytokine production, foam cell formation, giant cell formation, and phagocytosis.
Ca2+ is an essential second messenger responsible for modulating an array of cellular responses in numerous cell types, including macrophages. Ca2+-dependent signaling is associated with various macrophage inflammatory responses including atherogenesis, migration, phagocytosis, and foam cell formation [51,52,53,54,55,56]. The maintenance of macrophage Ca2+ homeostasis is in part mediated by ion channels and pumps, and its dysregulation can lead to numerous pathophysiological conditions [57, 58]. Importantly, TRPV4-dependent generation of Ca2+ influx has multifarious roles in different cell types including macrophages [1, 2, 5, 6, 11, 14, 29,30,31,32,33, 41, 59]. The current review specifically focuses on the role of macrophage TRPV4 in mediating inflammatory responses.
Pulmonary diseases
Among the present-day lifesaving interventions for acute respiratory distress syndrome, positive pressure mechanical ventilation is one of the most commonly used. However, mechanical ventilation with excessive tidal volumes can in turn contribute to ventilator-induced lung injury (VILI) characterized by a rapid increase in vascular permeability, cytokine release, and inflammatory cell infiltration [60, 61]. Interestingly, it was found that Ca2+ entry through TRPV4 initiates the increase in permeability during VILI in isolated mouse lungs [30]. Although earlier studies suggested a possible role of alveolar macrophages in increasing lung permeability in VILI, Hamanaka et al. were the first to identify the mechanical ventilation induced stretch activated TRPV4-dependent lung injury response in alveolar macrophages [46, 62, 63]. Alveolar macrophages from TRPV4 KO mice, after being activated by high volume ventilation, had decreased production of reactive oxygen (ROS) and nitrogen species (RNS), suggesting that TRPV4-dependent generation of ROS and RNS led to the formation of peroxynitrite, which accounted for the increased permeability. Furthermore, in the VILI model, TRPV4 was found to be linked with various macrophage responses such as spreading, phagocytosis, adhesion, and motility. TRPV4 KO mice failed to develop VILI, but the instillation of WT macrophages into TRPV4 KO mice restored the development of the lung injury, suggesting that mechanical activation of TRPV4 in alveolar macrophages plays a critical role in VILI [46]. Similarly, in a murine high tidal volume ventilation model of lung injury, blocking TRPV4 attenuated both the increase in pulmonary barrier permeability and the increase in proinflammatory cytokine expression by M1 macrophages [64].
Macrophage phagocytosis is a complex phenomenon that has evolved in multicellular organisms as a defense mechanism against foreign particles and pathogens, and as a housekeeping mechanism to clear out apoptotic cells during development and adult life [65,66,67,68]. Recently it was shown that LPS-triggered phagocytosis by macrophages of non-opsonized particles in vitro and of opsonized particles in vitro and in vivo was mediated by TRPV4, and that matrix stiffness >25 kPa (mimicking inflamed or fibrotic lungs) augmented this response [41]. Furthermore, this study showed that TRPV4 was essential for LPS-stimulated expression of various cytokines. Taken together, this work suggests a novel role of TRPV4 in macrophage phagocytosis, which could be consequential in physiological functions like resolution of lung inflammation, maintenance of tissue homeostasis, and defense against pulmonary infection and fibrosis. Overall, this study suggests that TRPV4 is sensitized by changes in matrix stiffness as a result of inflamed and/or infected lung, and cooperates with soluble factors including LPS to promote various macrophage responses including phagocytosis.
Tissue injury due to inflammation can lead to the release of an array of proteases such as trypsin, thrombin, and elastases [69, 70]. Protease activating receptor 2 (PAR2) is a G protein coupled receptor that is expressed in alveolar macrophages, endothelial cells, and epithelial cells involved in modulating inflammatory responses, obesity, and metabolism, and can be activated by several proteases [71, 72]. Recently, Rayees et al. identified an anti-inflammatory role of PAR2 in alveolar macrophages by suppression of toll-like receptor 4 (TLR4)-induced inflammation [73]. Mechanistically, PAR2-mediated cAMP generation inhibited TRPV4-dependent Ca2+ signaling in alveolar macrophages to resolve TLR-elicited inflammation. Depletion of TRPV4 using siRNA or other antagonists in PAR2 null mice blocked Ca2+ entry, and also reduced the levels of proinflammatory cytokines and levels of phosphorylation of NFκB and NFAT. Blockade of TRPV4 in PAR2 null mouse alveolar macrophages after LPS challenge promoted the resolution of inflammation and reversed lung injury [73]. Taken together, this study suggests that TRPV4 plays an essential role in mediating inflammation in TLR4-induced responses in alveolar macrophages.
Recent work by Li et al. showed that TRPV4 plays a crucial role in LPS-induced acute lung injury by regulating the calcineurin/NFATc3 signaling pathway [74]. They found that blocking TRPV4 function prevented pneumoedema in LPS-induced lung injury, and resulted in reduced production of proinflammatory molecules TNF-α, IL-6, and ROS. Further, they showed that TRPV4 activated macrophages through Ca2+ influx in LPS-induced lung injury. Specifically, they demonstrated that TRPV4 deficiency inhibited LPS-induced calcineurin activation, blocked nuclear translocation of NFATc3 in macrophages, and inhibited release of proinflammatory cytokines. Collectively, these data suggest that TRPV4-mediated Ca2+ influx activates the downstream calcineurin/NFATc3 signaling pathway, which mediates the inflammatory response in acute lung injury.
Atherosclerosis
Atherosclerosis, a leading contributor to mortality and morbidity around the world, is a progressive disease that is characterized by chronic inflammatory responses and fibrofatty lesions in large arteries; atherosclerosis is the principal cause of cerebral and myocardial infarction [75,76,77,78,79]. Injury to vascular endothelium marks the beginning of atherogenesis, which is characterized by trapping of LDL particles in arteries, followed by the expression of numerous inflammatory/adhesion molecules on the surface of endothelial cells [75,76,77,78,79]. Monocytes and T-lymphocytes attach to these molecules, and transmigrate into the arterial intima, where the monocytes differentiate into tissue macrophages, and upregulate expression of scavenger receptors [75,76,77,78,79]. Uptake of oxidized/modified LDL particles by scavenger receptors leads to the formation of macrophage foam cells, a critical atheroinflammatory process in atherosclerosis development [44, 56, 75,76,77,78,79,80]. The accumulating foam cells along with other cell debris, calcium, lipids, and extracellular matrix form fibro-atheromatous plaques [75,76,77,78,79]. Over the past decade, evidence of the role of inflammation in atherosclerosis, and its associated complications, has continued to grow [75,76,77,78,79, 81]. Earlier studies show that increases in overall oxidative stress attributed to chronic inflammatory conditions can aggravate the process of atherogenesis [75,76,77,78,79].
Ca2+ signaling is known to control a diverse array of macrophage functions including phagocytosis, foam cell formation, proliferation, migration, and adhesion [51,52,53,54,55,56,57,58]. Recent studies also report a role of matrix stiffness in the regulation of macrophage function [10, 36,37,38,39,40,41,42,43]. Macrophages are known to express an intricate system of ion channels/pumps that is involved in maintaining cellular calcium homeostasis [57, 58]. Our published data show that TRPV4 is required for oxLDL internalization by macrophages, and for subsequent formation of macrophage foam cells, and that loss of TRPV4 function (either genetic or pharmacological) abrogates foam cell formation [10]. Interestingly, emerging data support a role for a biomechanical factor, e.g., matrix stiffness, in the modulation of numerous proatherogenic macrophage functions, vascular elasticity, and atherogenesis [10, 36,37,38,39,40,41,42,43]. Our group showed that mechanical stimuli like matrix stiffness or scratch-induced macrophage foam cell formation was TRPV4 dependent, and this was particularly important as it mimicked the physiological conditions of atherosclerosis [10]. Future studies will determine how changes in matrix stiffness can lead to activation of mechanosensitive TRPV4 channels in a positive feed-forward manner to promote atheroinflammatory processes in vivo.
Approximately 50% of cardiovascular disease patients lack classic risk factors like hyperlipidemia, smoking, hypertension, and diabetes [76,77,78,79, 82]. Both clinical and experimental studies have shown that infection of microbial pathogens including P. gingivalis may serve as an additional risk factor in atherosclerosis [83,84,85,86,87,88,89,90]. Interestingly, recent studies suggest an association between periodontal disease and the generation of stiffness in arterial tissues [88, 90]. P. gingivalis, a predominant causative agent of periodontal disease, has been previously reported to accelerate proatherogenic processes in animal models, exerting its effect through various mechanisms including release of LPS, modulating binding/internalization of oxLDL, macrophage foam cell formation, and infiltration of M1 macrophages [83,84,85,86,87,88,89,90]. Published data from our group has recently shown that TRPV4 mechanosensing plays a role in P. gingivalis-LPS-triggered augmentation of oxLDL-induced macrophage foam cell formation [43]. Overall our results suggest that TRPV4 integrates LPS and matrix stiffness-induced responses during infection, and elicits Ca2+ influx, which mediates macrophage oxLDL uptake and foam cell formation. Although it was found that decreased foam cell formation in TRPV4 deficient macrophages was independent of CD36 (a major scavenger receptor for oxLDL) expression, there was increased co-localization of TRPV4 and CD36 in response to increasing matrix stiffness and LPS. Collectively, these data led us to postulate that increased matrix stiffness in LPS exposed macrophages causes co-localization and crosstalk of TRPV4 and CD36 leading to increased foam cell formation. These findings implicate a possible connection between periodontal infection, TRPV4, and eventual development of atherosclerosis.
Previously, Xu et al. reported an atheroprotective function of TRPV4, in which TRPV4 function in endothelial cells is associated with activation of eNOS and inhibition of monocyte adhesion to endothelial cells [91]. In contrast, deficiency of TRPV4 functions has been linked to numerous atheroinflammatory responses including endothelial dysfunction, reduced macrophage foam cell generation, and vascular diseases [9, 10, 27, 92]. Despite the past findings, an in vivo model supporting these in vitro findings is still missing. ApoE deficient mice have been associated with the development of hypercholesterolemia due to the poor lipoprotein metabolism and clearance, and are an established murine model of atherosclerosis [93, 94]. Thus, for gaining better mechanistic understanding of the link between TRPV4 and atherosclerosis, it is critical to elucidate the in vivo role of this channel utilizing an ApoE/TRPV4 double knockout mouse model, and to determine the responsible molecular mechanisms.
Foreign body response
The FBR is an end stage chronic inflammatory host reaction following implantation of a biomaterial, prosthesis, or medical device into soft tissues; FBR may cause harm to or death of the patient [95,96,97,98,99,100,101]. The events leading to the development of the FBR include adsorption of plasma proteins on the biomaterial, activation of complement system, macrophage recruitment and activation, generation of destructive foreign body giant cells (FBGC), and formation of fibrous tissue, which encapsulates the implant [95,96,97,98,99,100,101]. Despite the clinical importance of the condition, a thorough molecular understanding of the FBR is still lacking. Macrophages play a central role in development and progression of FBR through their expression of inflammatory proteins, formation of FBGCs, remodeling of the extracellular matrix, and encapsulation of the implant [95,96,97,98,99,100,101]. Previous reports by our group and others have shown that various macrophage functions such as phagocytosis, adhesion, and migration are responsive to changes in matrix stiffness, suggesting that biomechanical factors may play a role in the FBR [10, 36,37,38,39,40,41,42,43]. Recently, we reported that genetic ablation of TRPV4, a mechanosensitive channel, protects mice from FBR-related events [49]. TRPV4 deficient mice showed diminished collagen production, reduced macrophage accumulation, and reduced FBGC formation compared with WT mice in a subcutaneous biomaterial implantation model. Furthermore, we showed that genetic deficiency or pharmacologic inhibition of TRPV4 reduced cytokine-induced FBGC formation, which was restored by lentivirus-mediated TRPV4 reintroduction. Altogether, these results suggest an important, previously unsuspected role for TRPV4 in FBR. Delineation of the underlying TRPV4 activation and subsequent mechanism may identify attractive targets for future therapeutic intervention for FBR.
Fibrosis and chronic itch
The role of TRPV4 in fibrosis and chronic itch is an emerging area of research, and many groups including ours are interested in determining how this mechanosensitive Ca2+-permeant channel regulates various lung and skin-related pathologies. Fibrosis or scar formation cause chronic pathological conditions in lung, heart, kidney, skin, and liver, which are characterized by accumulation of myofibroblasts, epithelial–mesenchymal transition (EMT), and secretion of extracellular matrix proteins [102,103,104,105]. Tissue injury and exacerbated/uncontrolled myofibroblast differentiation are critical steps in the pathogenesis of fibrosis [102,103,104,105]. Various immune cells, specifically inflammatory monocytes and tissue-resident macrophages are key drivers of tissue regeneration and fibrosis [106]. Following tissue damage, monocytes/macrophages undergo phenotypic and functional transitions enabling their participation in various phases of tissue repair [106]. However, aberrant macrophage responses can lead to uncontrolled tissue repair due to sustained production of inflammatory mediators, growth factors, lack of M2 macrophages, excessive EMT, exacerbated myofibroblast generation, and aberrant activity of stem or tissue progenitor cells [106]. Previously, we reported that TRPV4 is associated with skin and lung fibrosis [11, 13, 14]. TRPV4 regulates both biochemical (Transforming growth factor β1)- and biomechanical (matrix stiffness) stimulus-induced lung and dermal myofibroblast differentiation, which is associated with fibrosis development in scleroderma, and contributes to the development of in vivo pulmonary and skin fibrosis in murine models [11, 14, 33]. We also showed that TRPV4 plays an important role in EMT in both human and murine primary keratinocytes [107]. However, the specific role of macrophage TRPV4 in fibrosis has not been determined. Development of cell-type specific animal models might shed more light into this relatively less explored area of research.
Chronic itch, a symptom of numerous skin disorders, is still poorly understood at the molecular level, and treatments are largely ineffective [108, 109]. Previous studies have identified hypotonicity and metabolites of the mevalonate pathway as activators of TRPV4-mediated nociception [110, 111]. However, Luo et al. in a recently published report, showed that the osmosensitive TRPV4 channels are selectively expressed in dermal macrophages and keratinocytes, and deletion of TRPV4 in macrophages and keratinocytes suppressed allergic and nonallergic itch in mice [109]. Skin biopsy samples from chronic idiopathic pruritus patients also had significantly higher expression of TRPV4 compared with healthy controls. Furthermore, their studies show that 5-hydroxytryptamine signaling is a critical downstream component of TRPV4-mediated allergic and nonallergic itch
Okada et al. used a corneal alkali burn wound healing model to determine the role of TRPV4 in corneal fibrosis [34]. They found higher TRPV4 expression in stromal cells after activation by alkali burn compared with the WT. They found that stromal opacification, due to development of fibrosis, was markedly reduced in TRPV4 KO mice. Immunohistochemistry data showed that TRPV4 KO mice failed to exhibit the expected fibrosis-associated increase in numbers of polymorphonuclear leukocytes and accumulation of macrophages. Furthermore, the data showed that macrophage release of interleukin-6 was reduced. Reciprocal bone marrow transplantation studies between WT and TRPV4 KO chimeric mouse models showed that reduced fibrosis and inflammation in TRPV4 KO mice were attributable in part to the loss of TRPV4 expression in macrophages. Altogether, these results suggest that alkali-induced corneal fibrosis and inflammation were, in part, dependent on macrophage TRPV4.
Conclusions
Inflammation is a vital part of the immunological response to injury and infection. However, it can also lead to tissue injury or destruction if unchecked. The role of TRPV4 in inflammatory diseases is being studied by several groups. In the setting of pulmonary diseases, macrophage TRPV4 has been seen to modulate both inflammatory and anti-inflammatory functions through its role in phagocytosis, release of cytokines, and regulation of signaling processes. TRPV4 was shown to be a novel regulator of matrix stiffness and LPS-induced oxLDL-mediated macrophage foam cell formation, a critical atheroinflammatory process in atherosclerosis. Emerging evidence also suggests a role of macrophage TRPV4 in FBR, fibrosis, and chronic allergic and nonallergic itch. Elucidation of the precise role and mechanism of macrophage TRPV4 in inflammatory conditions will be important for developing targeted therapeutics for the resolution of inflammatory diseases.
References
Liedtke W. Molecular mechanisms of TRPV4-mediated neural signaling. Ann N Y Acad Sci. 2008;1144:42–52.
Liedtke W, Friedman JM. Abnormal osmotic regulation in trpv4-/- mice. Proc Natl Acad Sci USA. 2003;200:13698–703.
Liedtke W, Tobin DM, Bargmann CI, Friedman JM. Mammalian TRPV4 (VR-OAC) directs behavioral responses to osmotic and mechanical stimuli in Caenorhabditis elegans. Proc Natl Acad Sci USA. 2003;100:14531–6.
Suzuki M, Mizuno A, Kodaira K, Imai M. Impaired pressure sensation in mice lacking TRPV4. J Biol Chem. 2003;278:22664–8.
Everaerts W, Nilius B, Owsianik G. The vanilloid transient receptor potential channel TRPV4: from structure to disease. Prog Biophys Mol Biol. 2010;103:2–17.
Garcia-Elias A, Mrkonjić S, Jung C, Pardo-Pastor C, Vicente R, Valverde MA. The trpv4 channel. Handb Exp Pharmacol. 2014;222:293–319.
Auer-Grumbach M, Olschewski A, Papić L, Kremer H, McEntagart ME, Uhrig S, et al. Alterations in the ankyrin domain of TRPV4 cause congenital distal SMA, scapuloperoneal SMA and HMSN2C. Nat Genet. 2010;42:160–4.
Adapala RK, Thoppil RJ, Luther DJ, Paruchuri S, Meszaros JG, Chilian WM, et al. TRPV4 channels mediate cardiac fibroblast differentiation by integrating mechanical and soluble signals. J Mol Cell Cardiol. 2013;54:45–52.
Du J, Wang X, Li J, Guo J, Liu L, Yan D, et al. Increasing TRPV4 expression restores flow-induced dilation impaired in mesenteric arteries with aging. Sci Rep. 2016;6:22780.
Goswami R, Merth M, Sharma S, Alharbi MO, Aranda-Espinoza H, Zhu X, et al. TRPV4 calcium-permeable channel is a novel regulator of oxidized LDL-induced macrophage foam cell formation. Free Radic Biol Med. 2017;110:142–50.
Goswami R, Cohen J, Sharma S, Zhang DX, Lafyatis R, Bhawan J, et al. TRPV4 ion channel is associated with scleroderma. J Investig Dermatol. 2016;137:962–5.
Köhler R, Heyken WT, Heinau P, Schubert R, Si H, Kacik M, et al. Evidence for a functional role of endothelial transient receptor potential V4 in shear stress-induced vasodilatation. Arterioscler Thromb Vasc Biol. 2006;26:1495–502.
Lamandé SR, Yuan Y, Gresshoff IL, Rowley L, Belluoccio D, Kaluarachchi K, et al. Mutations in TRPV4 cause an inherited arthropathy of hands and feet. Nat Genet. 2011;43:1142–6.
Sharma S, Goswami R, Merth M, Cohen J, Lei KY, Zhang DX, et al. TRPV4 ion channel is a novel regulator of dermal myofibroblast differentiation. Am J Physiol Cell Physiol. 2017;312:C562–C572.
Mochizuki T, Sokabe T, Araki I, Fujishita K, Shibasaki K, Uchida K, et al. The TRPV4 cation channel mediates stretch-evoked Ca2+ influx and ATP release in primary urothelial cell cultures. J Biol Chem. 2009;284:21257–64.
Thodeti CK, Matthews B, Ravi A, Mammoto A, Ghosh K, Bracha AL, et al. TRPV4 channels mediate cyclic strain-induced endothelial cell reorientation through integrin to integrin signalling. Circ Res. 2009;104:1123–30.
Loukin S, Zhou X, Su Z, Saimi Y, Kung C. Wild-type and brachyolmia-causing mutant TRPV4 channels respond directly to stretch force. J Biol Chem. 2010;285:27176–81.
Strotmann R, Harteneck C, Nunnenmacher K, Schultz G, Plant TD. OTRPC4, a nonselective cation channel that confers sensitivity to extracellular osmolarity. Nat Cell Biol. 2000;2:695–702.
Liedtke W, Choe Y, Marti-Renom MA, Bell AM, Denis CS, Sali A, et al. Vanilloid receptor-related osmotically activated channel (VROAC), a candidate vertebrate osmoreceptor. Cell. 2000;103:525–35.
O’Neil RG, Heller S. The mechanosensitive nature of TRPV channels. Pflugers Arch. 2005;451:193–203.
Güler A, Lee H, Shimizu I, Caterina MJ. Heat-evoked activation of TRPV4 (VR-OAC). J Neurosci. 2002;22:6408–14.
Vriens J, Watanabe H, Janssen A, Droogmans G, Voets T, Nilius B. Cell swelling, heat, and chemical agonists use distinct pathways for the activation of the cation channel TRPV4. Proc Natl Acad Sci USA. 2004;101:396–401.
Chung MK, Lee H, Caterina MJ. Warm temperatures activate TRPV4 in mouse 308 keratinocytes. J Biol Chem. 2003;278:32037–46.
Chung MK, Lee H, Mizuno A, Suzuki M, Caterina MJ. TRPV3 and TRPV4 mediate warmth-evoked currents in primary mouse keratinocytes. J Biol Chem. 2004;279:21569–75.
Grace MS, Lieu T, Darby B, Abogadie FC, Veldhuis N, Bunnett NW, et al. The tyrosine kinase inhibitor bafetinib inhibits PAR2-induced activation of TRPV4 channels in vitro and pain in vivo. Br J Pharmacol. 2014;171:3881–94.
Zheng X, Zinkevich NS, Gebremedhin D, Gauthier KM, Nishijima Y, Fang J, et al. Arachidonic acid-induced dilation in human coronary arterioles: convergence of signaling mechanisms on endothelial TRPV4-mediated Ca2 entry. J Am Heart Assoc. 2013;2:e000080.
Zhang DX, Mendoza SA, Bubolz AH, Mizuno A, Ge ZD, Li R, et al. Transient receptor potential vanilloid type 4-deficient mice exhibit impaired endothelium-dependent relaxation induced by acetylcholine in vitro and in vivo. Hypertension. 2009;53:532–8.
Oláh A, Tóth BI, Borbíró I, Sugawara K, Szöllõsi AG, Czifra G, et al. Cannabidiol exerts sebostatic and anti-inflammatory effects on human sebocytes. J Clin Investig. 2014;124:3713–24.
Thorneloe KS, Cheung M, Bao W, Alsaid H, Lenhard S, Jian MY, et al. An orally active TRPV4 channel blocker prevents and resolves pulmonary edema induced by heart failure. Sci Transl Med. 2012;4:159ra148.
Hamanaka K, Jian MY, Weber DS, Alvarez DF, Townsley MI, Al-Mehdi AB, et al. TRPV4 initiates the acute calcium-dependent permeability increase during ventilator-induced lung injury in isolated mouse lungs. Am J Physiol Lung Cell Mol Physiol. 2007;293:L923–32.
Everaerts W, Zhen X, Ghosh D, Vriens J, Gevaert T, Gilbert JP, et al. Inhibition of the cation channel TRPV4 improves bladder function in mice and rats with cyclophosphamide-induced cystitis. Proc Natl Acad Sci USA. 2010;107:19084–9.
Masuyama R, Vriens J, Voets T, Karashima Y, Owsianik G, Vennekens R, et al. TRPV4-mediated calcium influx regulates terminal differentiation of osteoclasts. Cell Metabol. 2008;8:257–65.
Rahaman SO, Grove LM, Paruchuri S, Southern BD, Abraham S, Niese KA, et al. TRPV4 mediates myofibroblast differentiation and pulmonary fibrosis in mice. J Clin Investig. 2014;124:5225–38.
Okada Y, Shirai K, Miyajima M, Reinach PS, Yamanaka O, Sumioka T, et al. Loss of TRPV4 function suppresses inflammatory fibrosis induced by alkali-burning mouse corneas. PLoS One. 2016;11:e0167200.
Mosser DM, Edwards JP. Exploring the full spectrum of macrophage activation. Nat Rev Immunol. 2008;8:958–69.
Blakney AK, Swartzlander MD, Bryant SJ. The effects of substrate stiffness on the in vitro activation of macrophages and in vivo host response to poly(ethylene glycol)-based hydrogels. J Biomed Mater Res. 2012;100:1375–86.
Hansen L, Taylor WR. Is increased arterial stiffness a cause or consequence of atherosclerosis? Atherosclerosis. 2016;249:226–7.
Hind LE, Dembo M, Hammer DA. Macrophage motility is driven by frontal-towing with a force magnitude dependent on substrate stiffness. Integr Biol. 2015;7:447–53.
Van Goethem E, Poincloux R, Gauffre F, Maridonneau-Parini I, Le Cabec V. Matrix architecture dictates three-dimensional migration modes of human macrophages: differential involvement of proteases and podosome-like structures. J Immunol. 2010;184:1049–61.
Previtera ML, Sengupta A. Substrate stiffness regulates proinflammatory mediator production through TLR4 activity in macrophages. PLoS One. 2015;10:e0145813.
Scheraga RG, Abraham S, Niese KA, Southern BD, Grove LM, Hite RD, et al. TRPV4 mechanosensitive ion channel regulates lipopolysaccharide-stimulated macrophage phagocytosis. J Immunol. 2016;196:428–36.
Adlerz KM, Aranda-Espinoza H, Hayenga HN. Substrate elasticity regulates the behavior of human monocyte-derived macrophages. Eur Biophys J. 2016;45:301–9.
Gupta N, Goswami R, Alharbi MO, Biswas D, Rahaman SO. TRPV4 is a regulator in P. gingivalis lipopolysaccharide-induced exacerbation of macrophage foam cell formation. Physiol Rep. 2019;7:e14069.
Rahaman SO, Lennon DJ, Febbraio M, Podrez EA, Hazen SL, Silverstein RL. A CD36-dependent signaling cascade is necessary for macrophage foam cell formation. Cell Metabol. 2006;4:211–21.
Balakrishna S, Song W, Achanta S, Doran SF, Liu B, Kaelberer MM, et al. TRPV4 inhibition counteracts edema and inflammation and improves pulmonary function and oxygen saturation in chemically induced acute lung injury. Am J Physiol Lung Cell Mol Physiol. 2014;307:L158–72.
Hamanaka K, Jian MY, Townsley MI, King JA, Liedtke W, Weber DS, et al. TRPV4 channels augment macrophage activation and ventilator-induced lung injury. Am J Physiol Lung Cell Mol Physiol. 2010;299:L353–62.
Zhu G, Gulsvik A, Bakke P, Ghatta S, Anderson W, Lomas DA, et al. Association of TRPV4 gene polymorphisms with chronic obstructive pulmonary disease. Hum Mol Genet. 2009;18:2053–62.
Henry CO, Dalloneau E, Pérez-Berezo MT, Plata C, Wu Y, Guillon A, et al. In vitro and in vivo evidence for an inflammatory role of the calcium channel TRPV4 in lung epithelium: potential involvement in cystic fibrosis. Am J Physiol Lung Cell Mol Physiol. 2016;311:L664–75.
Goswami R, Arya R, Biswas D, Zhu X, Rahaman SO. Transient receptor potential Vanilloid 4 (TRPV4) is required for foreign body response and giant cell formation. Am J Pathol. 2019;S0002-9440:30101–4. https://doi.org/10.1016/j.ajpath.2019.04.016.
Luo J, Feng J, Yu G, Yang P, Mack MR, Du J, et al. Transient receptor potential vanilloid 4-expressing macrophages and keratinocytes contribute differentially to allergic and nonallergic chronic itch. J Allergy Clin Immunol. 2017;141:608–19.
Melendez AJ, Tay HK. Phagocytosis: a repertoire of receptors and Ca(2+) as a key second messenger. Biosci Rep. 2008;28:287–98.
Nunes P, Demaurex N. The role of calcium signaling in phagocytosis. J Leukoc Biol. 2010;88:57–68.
Fleckenstein-Grün G, Thimm F, Czirfuzs A, Matyas S, Frey M. Experimental vasoprotection by calcium antagonists against calcium-mediated arteriosclerotic alterations. J Cardiovasc Pharmacol. 1994;24:S75–S84.
Shi H, Severs NJ, Robenek H. Effects of calcium on the migration and recruitment of macrophages and macrophage-derived foam cells. FASEB J. 1996;10:491–501.
Yang X, Zhang Y, Huang Y, Yang F. Changes of transmembrane Ca2+ gradient in the formation of macrophage-derived foam cells. Biosci Rep. 2000;20:1–12.
Rahaman SO, Zhou G, Silverstein RL. Vav protein guanine nucleotide exchange factor regulates CD36 protein-mediated macrophage foam cell formation via calcium and dynamin-dependent processes. J Biol Chem. 2011;286:36011–9.
Tang L, Gamal El-Din TM, Payandeh J, Martinez GQ, Heard TM, Scheuer T, et al. Structural basis for Ca2+ selectivity of a voltage-gated calcium channel. Nature. 2013;505:56–61.
Eisenhut M, Wallace H. Ion channels in inflammation. Pflugers Arch. 2011;461:401–21.
O’Conor CJ, Leddy HA, Benefield HC, Liedtke WB, Guilak F. TRPV4-mediated mechanotransduction regulates the metabolic response of chondrocytes to dynamic loading. Proc Natl Acad Sci. USA. 2014;111:1316–21.
Dos Santos CC, Slutsky AS. Invited review: mechanisms of ventilator-induced lung injury: a perspective. J Appl Physiol. 2000;89:1645–55.
Parker JC, Hernandez LA, Peevy K. Mechanisms of ventilator induced injury. Crit Care Med. 1993;21:131–43.
Eyal FG, Hamm CR, Parker JC. Reduction in alveolar macrophages attenuates acute ventilator induced lung injury in rats. Intensive Care Med. 2007;33:1212–8.
Frank JA, Wray CM, McAuley DF, Schwendener R, Matthay MA. Alveolar macrophages contribute to alveolar barrier dysfunction in ventilator-induced lung injury. Am J Physiol Lung Cell Mol Physiol. 2006;291:L1191–L1198.
Pairet N, Mang S, Fois G, Keck M, Kühnbach M, Gindele J, et al. TRPV4 inhibition attenuates stretch-induced inflammatory cellular responses and lung barrier dysfunction during mechanical ventilation. PLoS One. 2018;13:e0196055.
Martinez FO, Gordon S. The M1 and M2 paradigm of macrophage activation: time for reassessment. F1000Prime Rep. 2014;3:13.
Murray PJ, Wynn TA. Protective and pathogenic functions of macrophage subsets. Nat Rev Immunol. 2011;11:723–37.
Eddens T, Kolls JK. Host defenses against bacterial lower respiratory tract infection. Curr Opin Immunol. 2012;24:424–30.
Barth K, Remick DG, Genco CA. Disruption of immune regulation by microbial pathogens and resulting chronic inflammation. J Cell Physiol. 2013;228:1413–22.
Coughlin SR. Protease-activated receptors in hemostasis, thrombosis and vascular biology. J Throm. Haemost. 2005;3:1800–14.
Kaneider NC, Leger AJ, Agarwal A, Nguyen N, Perides G, Derian C, et al. ‘Role reversal’ for the receptor PAR1 in sepsis-induced vascular damage. Nat Immunol. 2007;8:1303–12.
Churg A, Wang X, Wang RD, Meixner SC, Pryzdial EL, Wright JL. Alpha1-antitrypsin suppresses TNF-alpha and MMP-12 production by cigarette smoke-stimulated macrophages. Am J Respir Cell Mol Biol. 2007;37:144–51.
Mihara K, Ramachandran R, Saifeddine M, Hansen KK, Renaux B, Polley D, et al. Thrombin-mediated direct activation of proteinase-activated receptor-2: another target for thrombin signaling. Mol Pharmacol. 2016;89:606–14.
Rayees S, Joshi JC, Tauseef M, Anwar M, Baweja S, Rochford I, et al. PAR2-mediated cAMP generation suppresses TRPV4-dependent Ca2+ signaling in alveolar macrophages to resolve TLR4-induced inflammation. Cell Rep. 2019;27:793–805.
Li M, Fang XZ, Zheng YF, Xie YB, Ma XD, Liu XT, et al. Transient receptor potential vanilloid 4 is a critical mediator in LPS mediated inflammation by mediating calcineurin/NFATc3 signaling. Biochem Biophys Res Commun. 2019;S0006-291X:30642–4.
Glass CK, Witztum JL. Atherosclerosis. the road ahead. Cell. 2001;104:503–16.
Lusis AJ. Atherosclerosis. Nature. 2000;407:233–41.
Moore KJ, Tabas I. The cellular biology of macrophages in atherosclerosis. Cell. 2011;145:341–55.
Moore KJ, Sheedy FJ, Fisher EA. Macrophages in atherosclerosis: a dynamic balance. Nat Rev Immunol. 2013;13:709–21.
McLaren JE, Michael DR, Ashlin TG, Ramji DP. Cytokines, macrophage lipid metabolism and foam cells: Implications for cardiovascular disease therapy. Prog Lipid Res. 2011;50:331–47.
Rahaman SO, Swat W, Febbraio M, Silverstein RL. Vav family Rho guanine nucleotide exchange factors regulate CD36-mediated macrophage foam cell formation. J Biol Chem. 2011;286:7010–7.
Libby P. Inflammation in atherosclerosis. Nature. 2002;420:868–74.
Thomas MR, Lip GY. Novel risk markers and risk assessments for cardiovascular disease. Circ Res. 2017;120:133–49.
Hayashi C, Viereck J, Hua N, Phinikaridou A, Madrigal AG, Gibson FC 3rd, et al. Porphyromonas gingivalis accelerates inflammatory atherosclerosis in the innominate artery of ApoE deficient mice. Atherosclerosis. 2011;215:52–9.
Fukasawa A, Kurita-Ochiai T, Hashizume T, Kobayashi R, Akimoto Y, Yamamoto M. Porphyromonas gingivalis accelerates atherosclerosis in C57BL/6 mice fed a high-fat diet. Immunopharmacol Immunotoxicol. 2012;34:470–6.
Chukkapalli SS, Velsko IM, Rivera-Kweh MF, Zheng D, Lucas AR, Kesavalu L. Polymicrobial oral infection with four periodontal bacteria orchestrates a distinct inflammatory response and atherosclerosis in ApoE null mice. PLoS One. 2015;10:e0143291.
Qi M, Miyakawa H, Kuramitsu HK. Porphyromonas gingivalis induces murine macrophage foam cell formation. Microb Pathog. 2003;35:259–67.
Teeuw WJ, Slot DE, Susanto H, Gerdes VE, Abbas F, D’Aiuto F, et al. Treatment of periodontitis improves the atherosclerotic profile: a systematic review and meta-analysis. J Clin Periodontol. 2014;41:70–9.
Houcken W, Teeuw WJ, Bizzarro S, Alvarez Rodriguez E, Mulders TA, van den Born BJ, et al. Arterial stiffness in periodontitis patients and controls. a case-control and pilot intervention study. J Hum Hypertens. 2016;30:24–9.
Kebschull M, Demmer RT, Papapanou PN. “Gum bug, leave my heart alone!“epidemiologic and mechanistic evidence linking periodontal infections and atherosclerosis. J Dent Res. 2010;89:879–902.
Schmitt A, Carra MC, Boutouyrie P, Bouchard P. Periodontitis and arterial stiffness: a systematic review and meta-analysis. J Clin Periodontol. 2015;42:977–87.
Xu S, Liu B, Yin M, Koroleva M, Mastrangelo M, Ture S, et al. A novel TRPV4-specific agonist inhibits monocyte adhesion and atherosclerosis. Oncotarget. 2016;7:37622–35.
Ye L, Kleiner S, Wu J, Sah R, Gupta RK, Banks AS, et al. TRPV4 is a regulator of adipose oxidative metabolism, inflammation, and energy homeostasis. Cell. 2012;151:96–110.
Zhang SH, Reddick RL, Piedrahita JA, Maeda N. Spontaneous hypercholesterolemia and arterial lesions in mice lacking apolipoprotein E. Science. 1992;258:468–71.
Jawien J. The role of an experimental model of atherosclerosis: apoE-knockout mice in developing new drugs against atherogenesis. Curr Pharm Biotechnol. 2012;13:2435–9.
Ratner BD. A pore way to heal and regenerate: 21st century thinking on biocompatibility. Regen Biomater. 2016;3:107–10.
Major MR, Wong VW, Nelson ER, Longaker MT, Gurtner GC. The foreign body response: at the interface of surgery and bioengineering. Plast Reconstr Surg. 2015;135:1489–98.
Velnar T, Bunc G, Klobucar R, Gradisnik L. Biomaterials and host versus graft response: a short review. Bosn J Basic Med Sci. 2016;16:82–90.
Anderson JM, Rodriguez A, Chang DT. Foreign body reaction to biomaterials. Semin Immunol. 2008;20:86–100.
Moore LB, Kyriakides TR. Molecular characterization of macrophage-biomaterial interactions. Adv Exp Med Biol. 2015;865:109–22.
Browne S, Pandit A. Biomaterial-mediated modification of the local inflammatory environment. Front Bioeng Biotechnol. 2015;3:67.
Brown BN, Ratner BD, Goodman SB, Amar S, Badylak SF. Macrophage polarization: an opportunity for improved outcomes in biomaterials and regenerative medicine. Biomaterials. 2012;33:3792–802.
Castelino FV, Varga J. Emerging cellular and molecular targets in fibrosis: implications for scleroderma pathogenesis and targeted therapy. Curr Opin Rheumatol. 2014;26:607–14.
Ho YY, Lagares D, Tager AM, Kapoor M. Fibrosis–a lethal component of systemic sclerosis. Nat Rev Rheumatol. 2014;10:390–402.
Trojanowska M. Noncanonical transforming growth factor β signaling in scleroderma fibrosis. Curr Opin Rheumatol. 2009;21:623–9.
Tschumperlin DJ. Fibroblasts and the ground they walk on. Physiology. 2013;28:380–90.
Wynn TA, Vannella KM. Macrophages in tissue repair, regeneration, and fibrosis. Immunity. 2016;44:450–62.
Sharma S, Goswami R, Zhang DX, Rahaman SO. TRPV4 regulates matrix stiffness and TGFβ1-induced epithelial-mesenchymal transition. J Cell Mol Med. 2019;23:761–74.
Matterne U, Strassner T, Apfelbacher CJ, Diepgen TL, Weisshaar E. Measuring the prevalence of chronic itch in the general population: development and validation of a questionnaire for use in large scale studies. Acta Derm Venereol. 2009;89:250–6.
Luo J, Feng J, Liu S, Walters ET, Hu H. Molecular and cellular mechanisms that initiate pain and itch. Cell Mol Life Sci. 2015;72:3201–23.
Alessandri-Haber N, Yeh JJ, Boyd AE, Parada CA, Chen X, Reichling DB, et al. Hypotonicity induces TRPV4-mediated nociception in rat. Neuron. 2003;39:497–511.
Bang S, Yoo S, Yang TJ, Cho H, Hwang SW. Nociceptive and pro-inflammatory effects of dimethylallyl pyrophosphate via TRPV4 activation. Br J Pharmacol. 2012;166:1433–43.
Acknowledgements
SOR was supported by a NIH grant (1R01EB024556-01), and NSF grant (CMMI-1662776).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dutta, B., Arya, R.K., Goswami, R. et al. Role of macrophage TRPV4 in inflammation. Lab Invest 100, 178–185 (2020). https://doi.org/10.1038/s41374-019-0334-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41374-019-0334-6
This article is cited by
-
Recent research advances in pain mechanisms in McCune–Albright syndrome thinking about the pain mechanism of FD/MAS
Journal of Orthopaedic Surgery and Research (2024)
-
TRP Channels in Stroke
Neuroscience Bulletin (2023)
-
Blockage of TRPV4 Downregulates the Nuclear Factor-Kappa B Signaling Pathway to Inhibit Inflammatory Responses and Neuronal Death in Mice with Pilocarpine-Induced Status Epilepticus
Cellular and Molecular Neurobiology (2023)
-
Role of sonic hedgehog signaling pathway in the regulation of ion channels: focus on its association with cardio-cerebrovascular diseases
Journal of Physiology and Biochemistry (2023)
-
Mechanosensing and Mechanosignal Transduction in Atherosclerosis
Current Atherosclerosis Reports (2023)