Abstract
Objective
To determine if prolonging gavage feedings in infants for ≥60 min is associated with decreased gastroesophageal reflux (GER) compared with bolus feeding using multiple-channel intraluminal impedance with pH probe (MII-pH).
Study design
Retrospective analysis of infants who underwent MII-pH between October 2009 and July 2018 and received gavage feedings. Infants were divided into two groups: bolus (<30 min) or prolonged (≥60 min). Symptoms, number of reflux events and percent time pH < 4 was compared.
Result
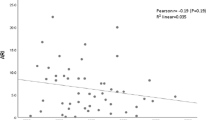
Fifty-eight infants underwent evaluation. Thirty-one (54%) received bolus gavage feedings and 27 (46%) received prolonged feedings. Groups differed in postmenstrual age. Total reflux episodes were significantly lower with prolonged feeding (median 19 vs. 28 episodes, p = 0.015), with no difference in acid exposure time. There was no significant difference in GER symptoms between the two groups.
Conclusion
Prolongation of gavage feedings was associated with decreased total numbers of GER events without reduction in GER symptoms.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Corvaglia L, Rotatori R, Ferlini M, Aceti A, Ancora G, Faldella G. The effect of body positioning on gastroesophageal reflux in premature infants: evaluation by combined impedance and pH monitoring. J Pediatr. 2007;151. https://doi.org/10.1016/j.jpeds.2007.06.014.
Omari TI, Barnett CP, Benninga MA, Lontis R, Goodchild L, Haslam RR, et al. Mechanisms of gastro-oesophageal reflux in preterm and term infants with reflux disease. Gut. 2002;51:475–9.
Frakaloss G, Burke G, Sanders MR. Impact of gastroesophageal reflux on growth and hospital stay in premature infants. J Pediatr Gastroenterol Nutr. 1998;26:146–50.
Murthy SV, Funderburk A, Abraham S, Epstein M, Dipalma J, Aghai ZH. Nasogastric feeding tubes may not contribute to gastroesophageal reflux in preterm infants. Am J Perinatol. 2018;35:643–7.
Funderburk A, Nawab U, Abraham S, Di Palma J, Epstein M, Aldridge H, et al. Temporal association between reflux-like behaviors and gastroesophageal reflux in preterm and term infants. J Pediatr Gastroenterol Nutr. 2016;62:556–61.
Grant L, Cochran D, EWER AK. Can pH monitoring reliably detect gastro-oesophageal reflux in preterm infants? Arch Dis Child—Fetal Neonatal Ed. 2002;85:155F–158.
Mousa HM, Rosen R, Woodley FW, Orsi M, Armas D, Faure C, et al. Esophageal impedance monitoring for gastroesophageal reflux. J Pediatr Gastroenterol Nutr 2011;52:129–39.
Schanler RJ, Shulman RJ, Lau C. Feeding strategies for premature infants: beneficial outcomes of feeding fortified human milk versus preterm formula. Pediatrics. 1999;103:1150–7.
Valman HB, Heath CD, Brown RJK. Continuous intragastric milk feeds in infants of low birth weight. Br Med J. 1972;3:547–50.
Wilson SSP, Paes J, Gray S. B. Cisapride: a review of the evidence supporting its use in premature infants with feeding intolerance. Neonatal Netw. 1997;16:17–64.
Jadcherla SR, Slaughter JL, Stenger MR, Klebanoff M, Kelleher K, Gardner W. Practice variance, prevalence, and economic burden of premature infants diagnosed with GERD. Hosp Pediatr. 2013;3:335–41.
Lopez-Alonso M, Moya MJ, Cabo JA, Ribas J, del Carmen Macias M, Silny J, et al. Twenty-four-hour esophageal impedance-ph monitoring in healthy preterm neonates: rate and characteristics of acid, weakly acidic, and weakly alkaline gastroesophageal reflux. Pediatrics. 2006;118:e299–308.
Rossor T, Lingam I, Douiri A, Bhat R, Greenough A. Detection of gastro-oesophageal reflux in the neonatal unit. Acta Paediatr Int J Paediatr. 2018;107:1535–40.
De Rose DU, Cresi F, Romano V, Barone G, Fundaro C, Filoni S, et al. Can MII-pH values predict the duration of treatment for GERD in preterm infants? Early Hum Dev. 2014;90:501–5.
Omari T, Barnett C, Snel A, Davidson G, Haslam R, Bakewell M, et al. Mechanism of gastroesophageal reflux in premature infants with chronic lung disease. J Pediatr Surg. 1999;34:1795–8.
Noviski N, Yehuda Ben Y, Serour F, Gorenstein A, Mandelberg A. Does the size of nasogastric tubes affect gastroesophageal reflux in children? J Pediatr Gastroenterol Nutr. 1999;29:448–51.
Eichenwald EC. Diagnosis and management of gastroesophageal reflux in preterm infants. Pediatrics. 2018;142:e20181061.
Parker P, Stroop S, Greene H. A controlled comparison of continuous versus intermittent feeding in the treatment of infants with intestinal disease. J Pediatr. 1981;99:360–4.
Aynsley Green A, Adrian TE, Bloom SR. Feeding and the development of enteroinsular hormone secretion in the preterm infant: effects of continuous gastric infusions of human milk compared with intermittent boluses. Acta Paediatrica. 1982;71:379–83.
Léonard Mashako MN, Bernard C, Cezard JP, Chayvialle JA, Navarro J. Effect of total parenteral nutrition, constant rate enteral nutrition, and discontinuous oral feeding on plasma cholecystokinin immunoreactivity in children. J Pediatr Gastroenterol Nutr. 1987;6:948–52.
Jadcherla SR, Chan CY, Moore R, Malkar M, Timan CJ, Valentine CJ. Impact of feeding strategies on the frequency and clearance of acid and nonacid gastroesophageal reflux events in dysphagic neonates. J Parenter Enter Nutr. 2012;36:449–55.
Jadcherla SR, Gupta A, Fernandez S, Nelin LD, Castile R, Gest AL, et al. Spatiotemporal characteristics of acid refluxate and relationship to symptoms in premature and term infants with chronic lung disease. Am J Gastroenterol. 2008;103:720–8.
Jadcherla SR, Peng J, Chan CY, Moore R, Wei L, Fernandez S, et al. Significance of gastroesophageal refluxate in relation to physical, chemical, and spatiotemporal characteristics in symptomatic intensive care unit neonates. Pediatr Res. 2011;70:192–8.
Author information
Authors and Affiliations
Contributions
MTF conceptualized and designed the study, searched the literature, analyzed the data, drafted the initial manuscript, and approved the final manuscript as submitted. SA analyzed the data, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. JDP critically reviewed the data analysis, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. ME performed the data collection, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. JSG conceptualized and designed the study, critically reviewed the data analysis, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. ZHA conceptualized and designed the study, searched the literature, analyzed the data, critically reviewed and revised the manuscript, and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Favara, M.T., Abraham, S., DiPalma, J. et al. Prolonging gavage feeds for reduction of gastroesophageal reflux in infants. J Perinatol 40, 916–921 (2020). https://doi.org/10.1038/s41372-020-0630-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0630-4