Abstract
Objective
To investigate factors associated with development of severe retinopathy of prematurity (ROP) in extremely preterm (EP) infants.
Study design
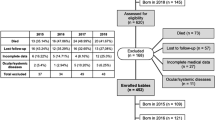
This retrospective cohort study included 213 EP infants (22 + 0 to 27 + 6 weeks gestation) who were admitted to the neonatal intensive care unit of Osaka Women’s and Children’s Hospital between 2009 and 2017. Multivariable logistic regression analysis was used to identify neonatal factors associated with severe ROP requiring treatment.
Result
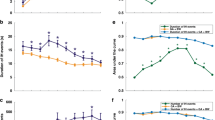
After adjustments for gestational age (GA), birth weight, sex, red blood cell transfusion, average SpO2, and fluctuations of SpO2 from birth to 32 weeks postmenstrual age, fluctuations of SpO2 (odds ratio [OR]: 2.10, 95% confidence interval [CI]: 1.03–4.27), and low GA (OR: 0.95, 95% CI: 0.91–0.98) were significantly associated with severe ROP.
Conclusions
Fluctuations of SpO2 from birth to 32 weeks postmenstrual age and low GA were significantly associated with development of severe ROP requiring treatment in EP infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Kono Y, Mishina J, Yonemoto N, Kusuda S, Fujimura M. Neonatal correlates of adverse outcomes in very low-birthweight infants in the NICU Network. Pediatr Int. 2011;53:930–5.
Takeuchi A, Koeda T, Takayanagi T, Sato K, Sugino N, Bonno M, et al. Reading difficulty in school-aged very low birth weight infants in Japan. Brain Dev. 2016;38:800–6.
Molloy CS, Anderson PJ, Anderson VA, Doyle LW. The long-term outcome of extremely preterm (<28 weeks' gestational age) infants with and without severe retinopathy of prematurity. J Neuropsychol. 2016;10:276–94.
Hartnett ME, Penn JS. Mechanisms and management of retinopathy of prematurity. N. Engl J Med. 2012;367:2515–26.
Chan-Ling T, C B, Stone J. The effect of oxygen on vasoformative cell division: evidence that ‘physiological hypoxia’ is the stimulus for normal retinal vasculogenesis. Investig Ophthalmol Vis Sci. 1995;36:1201–14.
Tin W, Milligan DW, Pennefather P, Hey E. Pulse oximetry, severe retinopathy, and outcome at one year in babies of less than 28 weeks gestation. Arch Dis Child Fetal Neonatal Ed. 2001;84:F106–110.
Noori S, Patel D, Friedlich P, Siassi B, Seri I, Ramanathan R. Effects of low oxygen saturation limits on the ductus arteriosus in extremely low birth weight infants. J Perinatol. 2009;29:553–7.
Carlo WA, Finer NN, Walsh MC, Rich W, Gantz MG, Laptook AR, et al. Target ranges of oxygen saturation in extremely preterm infants. N. Engl J Med. 2010;362:1959–69.
Tarnow-Mordi WO, Darlow B, Doyle L. Target ranges of oxygen saturation in extremely preterm infants. N Engl J Med. 2010;363:1285.
Finer NN, Carlo WA, Walsh MC, Rich W, Gantz MG, Laptook AR, et al. Early CPAP versus surfactant in extremely preterm infants. N. Engl J Med. 2010;362:1970–9.
Stenson B, Brocklehurst P, Tarnow-Mordi W. Increased 36-week survival with high oxygen saturation target in extremely preterm infants. N Engl J Med. 2011;364:1680–2.
Penn JS, Henry MM, Tolman BL. Exposure to alternating hypoxia and hyperoxia causes severe proliferative retinopathy in the newborn rat. Pediatr Res. 1994;36:724–31.
Michaelson IC. The mode of development of the vascular system of the retina, with some observations on its significance for certain retinal diseases. Trans Ophthalmol Soc UK. 1948;68:137–80.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Early Treatment For Retinopathy Of Prematurity Cooperative Group. Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol. 2003;121:1684–94.
Kim SJ, Port AD, Swan R, Campbell JP, Chan RVP, Chiang MF. Retinopathy of prematurity: a review of risk factors and their clinical significance. Surv Ophthalmol. 2018;63:618–37.
Siswanto JE, Ronoatmodjo S, Adisasmita A, Soemantri A, Sitorus RS, Sauer PJJ. Risk factors for the development and progression of retinopathy of prematurity in preterm infants in Indonesia. J Neonatal Perinatal Med. 2019. https://doi.org/10.3233/NPM-190233.
Anderson CG, Benitz WE, Madan A. Retinopathy of prematurity and pulse oximetry: a national survey of recent practices. J Perinatol. 2004;24:164–8.
Supplemental therapeutic oxygen for prethreshold retinopathy of 375 prematurity (STOP-ROP), a randomized, controlled trial. I: primary outcomes. Pediatrics. 2000;105:295–310.
Patz AEA, Eastham A, Higginbotham DH, Kleh T. Oxygen studies in retrolental fibroplasia. Am J Ophthalmol. 1953;36:1511–22.
Ashton NWB, Serpell G. Effect of oxygen on developing retinal vessels with particular reference to the problem of retrolental fibroplasia. Br J ophthalmol. 1954;38:397–432.
Saito Y, Omoto T, Cho Y, Hatsukawa Y, Fujimura M, Takeuchi T. The progression of retinopathy of prematurity and fluctuation in blood gas tension. Graefes Arch Clin Exp Ophthalmol. 1993;231:151–6.
York JR, Landers S, Kirby RS, Arbogast PG, Penn JS. Arterial oxygen fluctuation and retinopathy of prematurity in very-low-birth-weight infants. J Perinatol. 2004;24:82–87.
Biglan AW, Brown DR, Reynolds JD, Milley JR. Risk factors associated with retrolental fibroplasia. Ophthalmology. 1984;91:1504–11.
Katzman G, Satish M, Krishnan V. Hypoxemia and retinopathy of prematurity. Pediatrics. 1987;80:972.
Cunningham S, Fleck BW, Elton RA, McIntosh N. Transcutaneous oxygen levels in retinopathy of prematurity. Lancet. 1995;346:1464–5.
Das A, Mhanna M, Sears J, Houdek JW, Kumar N, Gunzler D, et al. Effect of fluctuation of oxygenation and time spent in the target range on retinopathy of prematurity in extremely low birth weight infants. J Neonatal Perinat Med. 2018;11:257–63.
Di Fiore JM, Bloom JN, Orge F, Schutt A, Schluchter M, Cheruvu VK, et al. A higher incidence of intermittent hypoxemic episodes is associated with severe retinopathy of prematurity. J Pediatr. 2010;157:69–73.
Gunn TR, Easdown J, Outerbridge EW, Aranda JV. Risk factors in retrolental fibroplasia. Pediatrics. 1980;65:1096–1100.
Pillekamp F, Hermann C, Keller T, von Gontard A, Kribs A, Roth B. Factors influencing apnea and bradycardia of prematurity - implications for neurodevelopment. Neonatology. 2007;91:155–61.
Poets CF, Roberts RS, Schmidt B, Whyte RK, Asztalos EV, Bader D, et al. Association between intermittent hypoxemia or bradycardia and late death or disability in extremely preterm infants. Jama. 2015;314:595–603.
Di Fiore JM, Martin RJ, Li H, Morris N, Carlo WA, Finer N, et al. Patterns of oxygenation, mortality, and growth status in the surfactant positive pressure and oxygen trial cohort. J Pediatr. 2017. https://doi.org/10.1016/j.jpeds.2017.01.057.
Raffay TM, Dylag AM, Sattar A, Abu Jawdeh EG, Cao S, Pax BM, et al. Neonatal intermittent hypoxemia events are associated with diagnosis of bronchopulmonary dysplasia at 36 weeks postmenstrual age. Pediatr Res. 2019;85:318–23.
Di Fiore JM, Dylag AM, Honomichl RD, Hibbs AM, Martin RJ, Tatsuoka C, et al. Early inspired oxygen and intermittent hypoxemic events in extremely premature infants are associated with asthma medication use at 2 years of age. J Perinatol. 2019;39:203–11.
McGregor ML, Bremer DL, Cole C, McClead RE, Phelps DL, Fellows RR, et al. Retinopathy of prematurity outcome in infants with prethreshold retinopathy of prematurity and oxygen saturation >94% in room air: the high oxygen percentage in retinopathy of prematurity study. Pediatrics. 2002;110:540–4.
Acknowledgements
The authors thank Drs Masashi Hotta, Yasuka Kimoto, Eriko Iwasaki, Makoto Tamura, Kazue Morikawa, Natsuko Yamamichi, and the medical staff working in the neonatal intensive care unit at Osaka Women’s and Children’s Hospital for their support during this study. We thank Ryan Chastain-Gross, Ph.D., from Edanz Group (https://en-author-services.edanzgroup.com) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Contributions
YI and KH conceptualized and designed the study, contributed to data analysis, and drafted the manuscript. MN, NM, SH, YF, YH, and KW reviewed results and gave conceptual suggestions. All authors reviewed the draft manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Imanishi, Y., Hirata, K., Nozaki, M. et al. Effect of fluctuation of oxygenation on the development of severe retinopathy of prematurity in extremely preterm infants. J Perinatol 40, 515–521 (2020). https://doi.org/10.1038/s41372-019-0571-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0571-y
This article is cited by
-
Oxygen saturation histogram classification system to evaluate response to doxapram treatment in preterm infants
Pediatric Research (2023)
-
Automated oxygen control for very preterm infants and neurodevelopmental outcome at 2 years−a retrospective cohort study
European Journal of Pediatrics (2023)