Abstract
Objective
To determine the impact of premedication for tracheal intubation (TI) on adverse TI associated events, severe oxygen desaturations, and first attempt success
Study design
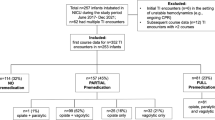
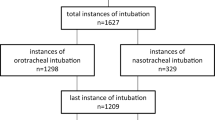
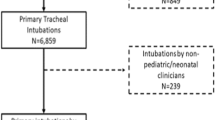
Retrospective cohort study in neonatal intensive care units (NICU) participating in the National Emergency Airway Registry for Neonates from 10/2014 to 6/2017. Premedication for TI was categorized as sedation with neuromuscular blockade, sedation only, or no medication.
Results
2260 TIs were reported from 11 NICUs. Adverse TI associated events occurred less often in sedation with neuromuscular blockade group (10%) as compared to sedation only (29%), or no medication group (23%), p < 0.001. The adjusted odds ratio (aOR) for adverse TI associated events were: sedation with neuromuscular blockade aOR 0.48 (95%CI 0.34–0.65, p < 0.001) compared to no medication.
Conclusion
Use of sedation with neuromuscular blockade was associated with favorable TI outcomes. This study supports the recommendation for the standard use of sedation with neuromuscular blockade in non-emergency TIs.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Foglia EE, Ades A, Napolitano N, Leffelman J, Nadkarni V, Nishisaki A. Factors associated with adverse events during tracheal intubation in the NICU. Neonatology. 2015;108:23–29.
Maheshwari R, Tracy M, Badawi N, Hinder M. Neonatal endotracheal intubation: how to make it more baby friendly. J Paediatr Child Health. 2016;52:480–6.
Venkatesh V, Ponnusamy V, Anandaraj J, Chaudhary R, Malviya M, Clarke P, et al. Endotracheal intubation in a neonatal population remains associated with a high risk of adverse events. Eur J Pediatr. 2011;170:223–7.
Foglia EAA, Sawyer T, Glass K, Singh N, Jung P, Quek BH, et al. Neonatal intubation practice and outcomes: an international registry study. Pediatrics. 2019;143:e20180902.
van Hasselt TJ. Question 1 What is the best sedative to give as premedication for neonatal intubation? Arch Dis Child. 2017;102:780–3.
Sauer CW, Kong JY, Vaucher YE, Finer N, Proudfoot JA, Boutin MA, et al. Intubation attempts increase the risk for severe intraventricular hemorrhage in preterm infants-A retrospective cohort study. J Pediatr. 2016;177:108–13.
Krick J, Gray M, Umoren R, Lee G, Sawyer T. Premedication with paralysis improves intubation success and decreases adverse events in very low birth weight infants: a prospective cohort study. J Perinatol. 2018;38:681–6.
Le CN, Garey DM, Leone TA, Goodmar JK, Rich W, Finer NN. Impact of premedication on neonatal intubations by pediatric and neonatal trainees. J Perinatol. 2014;34:458–60.
Kumar P, Denson SE, Mancuso TJ, Committee on F, Newborn SoA, Pain M. Premedication for nonemergency endotracheal intubation in the neonate. Pediatrics. 2010;125:608–15.
Bissuel M, Deguines C, Tourneux P. A national survey on pain management before tracheal intubation in neonates in French type III maternity units. Arch Pediatr. 2013;20:123–9.
Chaudhary R, Chonat S, Gowda H, Clarke P, Curley A. Use of premedication for intubation in tertiary neonatal units in the United Kingdom. Paediatr Anaesth. 2009;19:653–8.
Raban MS, Joolay Y, Horn AR, Harrison MC. Newborns should be receiving premedication before elective intubation. South African Med J. 2014;104:846–9.
Wheeler B, Broadbent R, Reith D. Premedication for neonatal intubation in Australia and New Zealand: a survey of current practice. J Paediatr Child Health. 2012;48:997–1000.
Durrmeyer X, Daoud P, Decobert F, Boileau P, Renolleau S, Zana-Taieb E, et al. Premedication for neonatal endotracheal intubation: results from the epidemiology of procedural pain in neonates study. Pediatr Crit Care Med. 2013;14:e169–175.
Barrington K. Premedication for endotracheal intubation in the newborn infant. Paediatrics & child health. 2011;16:159–71.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Kurth T, Walker AM, Glynn RJ, Chan KA, Gaziano JM, Berger K, et al. Results of multivariable logistic regression, propensity matching, propensity adjustment, and propensity-based weighting under conditions of nonuniform effect. Am J Epidemiol. 2006;163:262–70.
Fahnenstich H, Steffan J, Kau N, Bartmann P. Fentanyl-induced chest wall rigidity and laryngospasm in preterm and term infants. Crit Care Med. 2000;28:836–9.
Pacifici GM. Metabolism and pharmacokinetics of morphine in neonates: a review. Clinics. 2016;71:474–80.
Norman E, Wikstrom S, Hellstrom-Westas L, Turpeinen U, Hamalainen E, Fellman V. Rapid sequence induction is superior to morphine for intubation of preterm infants: a randomized controlled trial. J Pediatr. 2011;159:893–9 e891.
Ghanta S, Abdel-Latif ME, Lui K, Ravindranathan H, Awad J, Oei J. Propofol compared with the morphine, atropine, and suxamethonium regimen as induction agents for neonatal endotracheal intubation: a randomized, controlled trial. Pediatrics. 2007;119:e1248–1255.
Avino D, Zhang WH, De Ville A, Johansson AB. Remifentanil versus morphine-midazolam premedication on the quality of endotracheal intubation in neonates: a noninferiority randomized trial. J Pediatr. 2014;164:1032–7.
Feltman DM, Weiss MG, Nicoski P, Sinacore J. Rocuronium for nonemergent intubation of term and preterm infants. J Perinatol. 2011;31:38–43.
Ing CH, DiMaggio CJ, Malacova E, Whitehouse AJ, Hegarty MK, Feng T, et al. Comparative analysis of outcome measures used in examining neurodevelopmental effects of early childhood anesthesia exposure. Anesthesiology. 2014;120:1319–32.
Morriss FH Jr., Saha S, Bell EF, Colaizy TT, Stoll BJ, Hintz SR, et al. Surgery and neurodevelopmental outcome of very low-birth-weight infants. JAMA Pediatr. 2014;168:746–54.
Wallenstein MB, Birnie KL, Arain YH, Yang W, Yamada NK, Huffman LC, et al. Failed endotracheal intubation and adverse outcomes among extremely low birth weight infants. J Perinatol. 2016;36:112–5.
Attarian S, Tran LC, Moore A, Stanton G, Meyer E, Moore RP. The neurodevelopmental impact of neonatal morphine administration. Brain Sci. 2014;4:321–34.
Acknowledgements
We thank the NEAR4NEOS team and data coordinators at each participating site for their time, effort, and commitment. We thank Hayley Buffman, MPH and Stephanie Tuttle, MBA for their administrative support.
Funding
The current study is supported by NICHD 1R21HD089151. Drs. Ades, Sawyer, and Nishisaki and Ms. Napolitano are supported by NICHD 1R21HD089151. Dr. Nishisaki and Ms. Napolitano is supported by AHRQ 1R18HS024511.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ozawa, Y., Ades, A., Foglia, E.E. et al. Premedication with neuromuscular blockade and sedation during neonatal intubation is associated with fewer adverse events. J Perinatol 39, 848–856 (2019). https://doi.org/10.1038/s41372-019-0367-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0367-0
This article is cited by
-
Association of full premedication on tracheal intubation outcomes in the neonatal intensive care unit: an observational cohort study
Journal of Perinatology (2023)
-
Impact of multiple intubation attempts on adverse tracheal intubation associated events in neonates: a report from the NEAR4NEOS
Journal of Perinatology (2022)