Abstract
Objective
To identify specific risk factors for epilepsy for individuals born extremely preterm.
Study Design
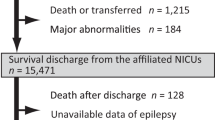
In a prospective cohort study, at 10-year follow-up, children were classified as having epilepsy or seizures not associated with epilepsy. We evaluated for association of perinatal factors using time-oriented, multinomial logistic regression models.
Results
Of the 888 children included in the study, 66 had epilepsy and 39 had seizures not associated with epilepsy. Epilepsy was associated with an indicator of low socioeconomic status, maternal gestational fever, early physiologic instability, postnatal exposure to hydrocortisone, cerebral white matter disease and severe bronchopulmonary dysplasia. Seizure without epilepsy was associated with indicators of placental infection and inflammation, and hypoxemia during the first 24 postnatal hours.
Conclusions
In children born extremely preterm, epilepsy and seizures not associated with epilepsy have different risk profiles. Though both profiles included indicators of infection and inflammation, the profile of risk factors for epilepsy included multiple indicators of endogenous vulnerability.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Guerrini R. Epilepsy in children. Lancet. 2006;367:499–524.
Hoppenbrouwers T. Sudden infant death syndrome, sleep, and seizures. J Child Neurol. 2015;30:904–11.
Russ S, Larson K, Halfon N. A national profile of childhood epilepsy and seizure disorder. Pediatrics. 2012;129:256–64.
Camfield P, Camfield C. Incidence, prevelance and aetiology of seizures and epilepsy in children. Epileptic Dis. 2015;17:117–23.
Douglass LM, Kuban K, Tarquinio D, Schraga L, Jonas R, Heeren T, et al. A novel parent questionnaire for the detection of seizures in children. Pediatr Neurol. 2016;54:64–9.
Falchi M, Palmas G, Pisano T, Meloni M, Gaspa G, Puddu M, et al. Incidence of epilepsy in extremely low-birthweight infants (<1,000 g): A population study of central and southern Sardinia. 2009. Epilepsia. 2009;50:37–40.
Ishikawa T, Kishi S, Inukai K, Kono C, Kitoh H, Awaya A, et al. Subsequent epilepsy in very-low birthweight infants: a long term follow-up study from birth. Epilepsia. 1995;36:435–9.
Sun Y, Vestergaard M, Pedersen CB, Christensen J, Basso O, Olsen J. Gestational age, birth weight, intrauterine growth and risk for epilepsy. Am J Epidemiol. 2008;167:262–70.
Meeraus WH, Petersen I, Gilbert R. Association between antibiotic prescribing in pregnancy and cerebral palsy or epilepsy in children born at term: a cohort study using the Health Improvement Network. PLoS ONE. 2015;10:e0122034.
Warrington JP. Placental ischemia increases seizure susceptibility and cerebrospinal fluid cytokines. Physiol Rep. 2015;3:e12634.
Ko HS, Cheon JY, Choi SK, Lee HW, Lee A, Park IY, et al. Placental histologic patterns and Neonatal seizure, in preterm premature rupture of membrane. J Matern Fetal Neonatal Med. 2017;30:793–800.
Walsh S, Donnan J, Fortin Y, Sikora L, Morrissey A, Collins K, et al. A systematic review of the risks factors associated with the onset and natural progression of epilepsy. Neurotoxicology. 2017;61:64–77.
Crump C, Sundquist K, Winkleby M, Sundquist J. Preterm birth and risk of epilepsy in Swedish adults. Neurology. 2011;77:1376–82.
Larpthaveesarp A, Ferriero DM, Gonzalez FF. Growth factors for the treatment of ischemic brain injury (growth factor treatment). Brain Sci. 2015;5:165–77.
Hirst JJ, Cumberland AL, Shaw JC, Bennett GA, Kelleher MA, Walker DW, et al. Loss of neurosteroid-mediated protection following stress during fetal life. J Ster Biochem Mol Biol. 2016;160:181–8.
Gille C, Dreschers S, Leiber A, Lepiorz F, Krusch M, Grosse-Opphoff J, et al. The CD95/CD95L pathway is involved in phagocytosis-induced cell death of monocytes and may account for sustained inflammation in neonates. Pediatr Res. 2013;73(4 Pt 1):402–8.
Brochu ME, Girard S, Lavoie K, Sebire G. Developmental regulation of the neuroinflammatory responses to LPS and/or hypoxia-ischemia between preterm and term neonates: An experimental study. J Neuroinflam. 2011;8:55.
McElrath TF, Fichorova RN, Allred EN, Hecht JL, Ismail MA, Yuan H, et al. Blood protein profiles of infants born before 28 weeks differ by pregnancy complication. Am J Obstet Gynecol. 2011;204:418.e411–8.
Strunk T, Inder T, Wang X, Burgner D, Mallard C, Levy O. Infection-induced inflammation and cerebral injury in preterm infants. Lancet Infec Dis. 2014;14:751–62.
Martin CR, Dammann O, Allred EN, Patel S, O’Shea TM, Kuban KC, et al. Neurodevelopment of extremely preterm infants who had necrotizing enterocolitis with or without late bacteremia. J Pediatr. 2010;157:751–6.
Bose CL, Laughon MM, Allred EN, O’Shea TM, Van Marter LJ, Ehrenkranz RA, et al. Systemic inflammation associated with mechanical ventilation among extremely preterm infants. Cytokine. 2013;61:315–22.
Larroque B, Ancel PY, Marret S, Marchand L, Andre M, Arnaud C, et al. Neurodevelopmental disabilities and special care of 5-year-old children born before 33 weeks of gestation (the EPIPAGE study): a longitudinal cohort study. Lancet. 2008;371:813–20.
De Groote I, Vanhaesebrouck P, Bruneel E, Dom L, Durein I, Hasaerts D, et al. for the Extremely Preterm Infants in Belgium (EPIBEL) Study Group. Outcomes at 3 years of age in a population-based cohort of extremely preterm infants. Obstet Gynecol. 2007;110:855–64.
O’Shea TM, Allred EN, Dammann O, Hirtz D, Kuban KC, Paneth N, et al. for ELGAN study Investigators. The ELGAN study of the brain and related disorders in extremely low gestational age newborns. Early Hum Dev. 2009;85:719–25.
Joseph RM, O’Shea TM, Allred EN, Heeren T, Hirtz D, Jara H. et al. ELGAN Study Investigators. Neurocognitive and academic outcomes at age 10 years of extremely preterm newborns. Pediatrics. 2016;137:e20154343.
Holcroft CJ, Blakemore KJ, Allen M, Graham EM. Association of prematurity and neonatal infection with neurologic morbidity in very low birth weight infants. Obstet Gynecol. 2003;101:1249–53.
Hirschberger RG, Kuban KCK, O’Shea TM, Joseph RM, Heeren T, Douglass LM, et al. for ELGAN Study Investigators. Co-occurrence and severity of neurodevelopmental burden (cognitive impairment, cerebral palsy, autism spectrum disorder, and epilepsy) at age ten years in children born extremely preterm. Pediatr Neurol. 2018;79:45–52.
Schiariti V, Farrell K, Houbé JS, Lisonkova S. Period prevalence of epilepsy in children in BC: a population-based study. Can J Neurol Sci. 2009;36:36–41.
Sidenvall R, Heijbel J, Blomquist HK, Nyström L, Forsgren L. An incident case-control study of first unprovoked afebrile seizures in children: a population-based study of pre- and perinatal risk factors. Epilepsia. 2001;42:1261–5.
Vestergaard M, Wisborg K, Henriksen TB, Secher NJ, Ostergaard JR, Olsen J. Prenatal exposure to cigarettes, alcohol, and coffee and the risk for febrile seizures. Pediatrics. 2005;116:1089–94.
Spencer NJ, Blackburn CM, Read JM. Disabling chronic conditions in childhood and socioeconomic disadvantage: a systematic review and meta-analyses of observational studies. BMJ Open. 2015;5:e007062.
Whitehead NS. The relationship of socioeconomic status to preterm contractions and preterm delivery. Matern Child Health J. 2012;16:1645–56.
Miller SL, Huppi PS, Mallard C. The consequences of fetal growth restriction on brain structure and neurodevelopmental outcome. J Physiol. 2016;594:807–23.
Hair NL, Hanson JL, Wolfe BL, Pollak SD. Association of child poverty, brain development, and academic achievement. JAMA Pediatr. 2015;169:822–9.
de Vries EE, van den Munckhof B, Braun KP, van Royen-Kerkhof A, de Jager W, Jansen FE. Inflammatory mediators in human epilepsy: A systematic review and meta-analysis. Neurosci Biobeh Rev. 2016;63:177–90.
Koh S. Role of Neuroinflammation in evolution of childhood epilepsy. J Child Neurol. 2018;33:64–72.
Choi J, Nordli DR, Alden TD, DiPatri A, Laux L, Kelley K, et al. Cellular injury and neuroinflammation in children with chronic intractable epilepsy. J Inflamm. 2009;6:38.
Wu CS, Pedersen LH, Miller JE, Sun Y, Streja E, Uldall P, et al. Risk of cerebral palsy and childhood epilepsy related to infections before or during pregnancy. PLoS ONE. 2013;8:e57552.
Vestergaard M, Christensen J, Ness RB, Haggerty CL, Olsen J. Preeclampsia and risk for epilepsy in offspring. Pediatrics. 2008;122:1072–8.
Botet F, Figueras J, Carbonell-Estrany X, Narbona E. The impact of clinical maternal chorioamnionitis on neurological and psychological sequelae in very-low-birth weight infants: a case-control study. J Perinat Med. 2011;39:203–8.
Lu HY, Zhang Q, Wang QX, Lu JY. Contribution of histological chorioamnionitis and fetal inflammatory response syndrome to increased risk of brain injury in infants with preterm premature rupture of membranes. Pediatr Neurol. 2016;61:94–8.
Butler T, Li Y, Tsui W, Friedman D, Maoz A, Wang X, et al. Transient and chronic seizure‐induced inflammation in human focal epilepsy. Epilepsia. 2016;57:e191–4.
Resch B, Resch E, Maurer-Fellbaum U, Pichler-Stachl E, Riccabona M, Hofer N, et al. The whole spectrum of cystic periventricular leukomalacia of the preterm infant: results from a large consecutive case series. Child’s Nerv Syst. 2015;31:1527–32.
Leviton A, Allred EN, Kuban KC, Hecht JL, Onderdonk AB, O’Shea TM, et al. Microbiologic and histologic characteristics of the extremely preterm infant’s placenta predict white matter damage and later cerebral palsy. The ELGAN study. Pediatr Res. 2010;67:95–101.
Empana JP, Subtil D, Truffert P. In-hospital mortality of newborn infants born before 33 weeks of gestation depends on the initial level of neonatal care: the EPIPAGE study. Acta Pædiatrica. 2013;92:346–51.
Profit J, Sharek PJ, Kan P, Rigdon J, Desai M, Nisbet CC, et al. Teamwork in the NICU setting and its association with healthcare-associated infections in very low birth weight infants. Am J Perinatol. 2017;34:1032–40.
McDonald JW, Levine JM, Qu Y. Multiple classes of the oligodendrocyte lineage are highly vulnerable to excitotoxicity. Neuroreport. 1998;9:2757–62.
Skaper SD. The biology of neurotrophins, signalling pathways, and functional peptide mimetics of neurotrophins and their receptors. CNS Neurol Dis Drug Targ. 2008;7:46–62.
Victor S, Appleton RE, Beirne M, Marson AG, Weindling AM. Effect of carbon dioxide on background electrical activity and fractional oxygen extraction in very low birth weight infants just after birth. Pediatr Res. 2005;58:579–85.
Fritz KI, Ashraf QM, Mishra OP, Delivoria-Papadopoulos M. Effect of moderate hypocapnia ventilation on nuclear DNA fragmentation and energy metabolism in the cerebral cortex of newborn piglets. Pediatr Res. 2001;50:586–9.
Ozsurekci Y, Aykac K. Oxidative stress related diseases in newborns. Oxid Med Cell Longev. 2016;2016:2768365.
Humphreys P, Deonandan R, Whiting S, Barrowman N, Matzinger MA, Briggs V, et al. Factors associated with epilepsy in children with periventricular leukomalacia. J Child Neurol. 2007;22:598–605.
Resić B, Tomasović M, Kuzmanić-Samija R, Lozić M, Resić J, Solak M. Neurodevelopmental outcome in children with periventricular leukomalacia. Coll Antropol. 2008;32(Suppl 1):143–7.
Leviton A, Gressens P. Neuronal damage accompanies perinatal white-matter damage. Trends Neurosci. 2007;30:473–8.
Acknowledgements
We gratefully acknowledge the contributions of their subjects, and their subjects’ families, as well as those of their colleagues. Participating institutions (site principal investigator and colleagues): Baystate Medical Center, Springfield MA (Rachana Singh, Bhavesh Shah, Debby Klein); Beth Israel Deaconess Medical Center, Boston MA (Camilia R. Martin, Colleen Hallisey, Caitlin Hurley, Miren Creixell); Brigham & Women’s Hospital, Boston MA (Linda J. Van Marter); Children’s Hospital, Boston MA (Alan Leviton, Kathleen Lee, Anne McGovern, Elizabeth Allred, Jill Gambardella, Susan Ursprung, Ruth Blomquist); Massachusetts General Hospital, Boston MA (Robert Insoft, Jennifer G. Wilson, Maureen Pimental); New England Medical Center, Boston MA (Cynthia Cole, John Fiascone, Janet Madden, Ellen Nylen, Anne Furey); U Mass Memorial Health Center, Worcester, MA (Francis Bednarek[deceased], Mary Naples, Beth Powers); Yale-New Haven Hospital, New Haven CT (Richard Ehrenkranz [deceased], Joanne Williams, Elaine Romano); Forsyth Hospital, Baptist Medical Center, Winston-Salem NC (T. Michael O’Shea, Debbie Gordon, Teresa Harold, Gail Hounsell, Debbie Hiatt); University Health Systems of Eastern Carolina, Greenville NC (Stephen Engelke, Sherry Moseley, Linda Pare, Donna Smart, Joan Wilson); North Carolina Children’s Hospital, Chapel Hill NC (Carl Bose, Gennie Bose, Janice Wereszczak); DeVos Children’s Hospital, Grand Rapids MI (Mariel Portenga, Dinah Sutton); Sparrow Hospital, Lansing MI (Padmani Karna, Carolyn Solomon); University of Chicago Hospital, Chicago IL (Michael D. Schreiber, Grace Yoon); William Beaumont Hospital, Royal Oak MI (Daniel Batton, Beth Kring).
Funding
This study was supported by grants from the National Institute of Neurological Disorders and Stroke (5U01NS040069–05; 2R01NS040069 − 06A2), the National Institute of Child Health and Human Development (5P30HD018655–34), and the Office of the National Institutes of Health Director (1UG3OD023348–01).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Financial disclosure for authors
The authors have no financial relationships relevant to this article to disclose.
Supplementary information
Rights and permissions
About this article
Cite this article
Singh, R., Douglass, L.M., O’Shea, T.M. et al. Antecedents of epilepsy and seizures among children born at extremely low gestational age. J Perinatol 39, 774–783 (2019). https://doi.org/10.1038/s41372-019-0355-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0355-4