Abstract
Objective
To classify NICU interventions for parental distress and quantify their effectiveness.
Study design
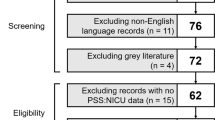
We systematically reviewed controlled studies published before 2017 measuring NICU parental distress, defined broad intervention categories, and used random-effects meta-analysis to quantify treatment effectiveness.
Results
Among 1643 unique records, 58 eligible trials predominantly studied mothers of preterm infants. Interventions tested in 22 randomized trials decreased parental distress (p < 0.001) and demonstrated improvement beyond 6 months (p < 0.005). In subgroup analyses, complementary/alternative medicine and family-centered instruction interventions each decreased distress symptoms (p < 0.01), with fathers and mothers improving to similar extents. Most psychotherapy studies decreased distress individually but did not qualify for meta-analysis as a group.
Conclusion
NICU interventions modestly reduced parental distress. We identified family-centered instruction as a target for implementation and complementary/alternative medicine as a target for further study. Investigators must develop psychosocial interventions that serve NICU parents at large, including fathers and parents of full-term infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Sanders MR, Hall SL. Trauma-informed care in the newborn intensive care unit: promoting safety, security and connectedness. J Perinatol. 2018;38:3–10.
Bonanno GA, Westphal M, Mancini AD. Resilience to loss and potential trauma. Annu Rev Clin Psychol. 2011;7:511–35.
Schappin R, Wijnroks L, Uniken Venema MM, Jongmans MJ. Rethinking stress in parents of preterm infants: a meta-analysis. PLoS ONE. 2013;8:e54992.
Woodward LJ, Bora S, Clark CA, Montgomery-Honger A, Pritchard VE, Spencer C, et al. Very preterm birth: maternal experiences of the neonatal intensive care environment. J Perinatol. 2014;34:555–61.
Boulais J, Vente T, Daley M, Ramesh S, McGuirl J, Arzuaga B. Concern for mortality in the neonatal intensive care unit (NICU): parent and physician perspectives. J Perinatol. 2018;38:718–27.
Jeffcoate JA, Humphrey ME, Lloyd JK. Role perception and response to stress in fathers and mothers following pre-term delivery. Soc Sci Med. 1979;13A:139–45.
Treyvaud K. Parent and family outcomes following very preterm or very low birth weight birth: a review. Semin Fetal Neonatal Med. 2014;19:131–5.
Hoffman C, Dunn DM, Njoroge WFM. Impact of postpartum mental illness upon infant development. Curr Psychiatry Rep. 2017;19:100.
Garthus-Niegel S, Ayers S, Martini J, von Soest T, Eberhard-Gran M. The impact of postpartum post-traumatic stress disorder symptoms on child development: a population-based, 2-year follow-up study. Psychol Med. 2017;47:161–70.
Huhtala M, Korja R, Lehtonen L, Haataja L, Lapinleimu H, Rautava P, et al. Associations between parental psychological well-being and socio-emotional development in 5-year-old preterm children. Early Hum Dev. 2014;90:119–24.
United States Department of Health and Human Services. Health Resources and Services Administration/Maternal and Child Health Bureau. Child health USA 2013. Rockville, MD: U.S. Department of Health and Human Services; 2013.
Hynan MT, Mounts KO, Vanderbilt DL. Screening parents of high-risk infants for emotional distress: rationale and recommendations. J Perinatol. 2013;33:748–53.
Yildiz PD, Ayers S, Phillips L. The prevalence of posttraumatic stress disorder in pregnancy and after birth: a systematic review and meta-analysis. J Affect Disord. 2017;208:634–45.
Lefkowitz DS, Baxt C, Evans JR. Prevalence and correlates of posttraumatic stress and postpartum depression in parents of infants in the Neonatal Intensive Care Unit (NICU). J Clin Psychol Med Settings. 2010;17:230–7.
Cyr-Alves H, Macken L, Hyrkas K. Stress and symptoms of depression in fathers of infants admitted to the NICU. J Obstet Gynecol Neonatal Nurs. 2018;47:146–57.
Shaw RJ, Bernard RS, Deblois T, Ikuta LM, Ginzburg K, Koopman C. The relationship between acute stress disorder and posttraumatic stress disorder in the neonatal intensive care unit. Psychosomatics. 2009;50:131–7.
Aftyka A, Rybojad B, Rosa W, Wrobel A, Karakula-Juchnowicz H. Risk factors for the development of post-traumatic stress disorder and coping strategies in mothers and fathers following infant hospitalisation in the neonatal intensive care unit. J Clin Nurs. 2017;26:4436–45.
Philpott LF, Leahy-Warren P, FitzGerald S, Savage E. Stress in fathers in the perinatal period: a systematic review. Midwifery. 2017;55:113–27.
Hynan MT, Hall SL. Psychosocial program standards for NICU parents. J Perinatol. 2015;35(Suppl 1):S1–4.
Brecht C, Shaw RJ, Horwitz SM, John NH. Effectiveness of therapeutic behavioral interventions for parents of low birth weight premature infants: a review. Infant Ment Health J. 2012;33:651–65.
Benzies KM, Magill-Evans JE, Hayden KA, Ballantyne M. Key components of early intervention programs for preterm infants and their parents: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2013;13(Suppl 1):S10.
Kraljevic M, Warnock FF. Early educational and behavioral RCT interventions to reduce maternal symptoms of psychological trauma following preterm birth: a systematic review. J Perinat Neonatal Nurs. 2013;27:311–27.
Mendelson T, Cluxton-Keller F, Vullo GC, Tandon SD, Noazin S. NICU-based interventions to reduce maternal depressive and anxiety symptoms: a meta-analysis. Pediatrics. 2017;139;1–12.
Zhang X, Kurtz M, Lee SY, Liu H. Early intervention for preterm infants and their mothers: a systematic review. J Perinat Neonatal Nurs. 2014;1–14.
Sisson H, Jones C, Williams R, Lachanudis L. Metaethnographic synthesis of fathers’ experiences of the neonatal intensive care unit environment during hospitalization of their premature infants. J Obstet Gynecol Neonatal Nurs. 2015;44:471–80.
DeMier RL, Hynan MT, Harris HB, Manniello RL. Perinatal stressors as predictors of symptoms of posttraumatic stress in mothers of infants at high risk. J Perinatol. 1996;16:276–80.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100.
Holditch-Davis D, Miles MS, Weaver MA, Black B, Beeber L, Thoyre S, et al. Patterns of distress in African-American mothers of preterm infants. J Dev Behav Pediatr. 2009;30:193–205.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Palmer TM, Sterne JAC (editors) Meta-analysis in stata: an updated collection from the Stata Journal. College Station, TX: Stata Press; 2016.
Hall SL, Ryan DJ, Beatty J, Grubbs L. Recommendations for peer-to-peer support for NICU parents. J Perinatol. 2015;35(Suppl 1):S9–13.
O’Brien K, Bracht M, Macdonell K, McBride T, Robson K, O’Leary L, et al. A pilot cohort analytic study of Family Integrated Care in a Canadian neonatal intensive care unit. BMC Pregnancy Childbirth. 2013;13(Suppl 1):S12.
Fawole OA, Dy SM, Wilson RF, Lau BD, Martinez KA, Apostol CC, et al. A systematic review of communication quality improvement interventions for patients with advanced and serious illness. J Gen Intern Med. 2013;28:570–7.
National Center for Complementary and Integrative Health. 2016 strategic plan: exploring the science of complementary and integrative health. 2016. https://nccih.nih.gov/sites/nccam.nih.gov/files/NCCIH_2016_Strategic_Plan.pdf
Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1–23.
Burke S. Systematic review of developmental care interventions in the neonatal intensive care unit since 2006. J Child Health Care. 2018;22:269–86.
Conde-Agudelo A, Diaz-Rossello JL. Kangaroo mother care to reduce morbidity and mortality in low birthweight infants. Cochrane Database Syst Rev. 2016;8:Cd002771.
Clarke-Pounder JP, Boss RD, Roter DL, Hutton N, Larson S, Donohue PK. Communication intervention in the neonatal intensive care unit: can it backfire? J Palliat Med. 2015;18:157–61.
Shaw RJ, St John N, Lilo E, Jo B, Benitz W, Stevenson DK, et al. Prevention of traumatic stress in mothers of preterms: 6-month outcomes. Pediatrics. 2014;134:e481–488.
Shaw RJ, St John N, Lilo EA, Jo B, Benitz W, Stevenson DK, et al. Prevention of traumatic stress in mothers with preterm infants: a randomized controlled trial. Pediatrics. 2013;132:e886–894.
Hynan MT, Steinberg Z, Baker L, Cicco R, Geller PA, Lassen S, et al. Recommendations for mental health professionals in the NICU. J Perinatol. 2015;35(Suppl 1):S14–18.
Yogman M, Garfield CF. Fathers’ roles in the care and development of their children: the role of pediatricians. Pediatrics. 2016;138:e1–e15.
Acknowledgements
The authors wish to thank Bethany Myers for library guidance, Sitaram Vangala for statistical guidance, Isabell Purdy for intervention-classification input, and Catherine Mogil for critical feedback. Database services provided by the NIH/NCATS grant UL1TR000124.
Funding
This study was supported by a UCLA Mattel Children’s Discovery and Innovation Institute Seed Grant. This study was supported exclusively by intramural funding.
Author information
Authors and Affiliations
Contributions
AS conceptualized, designed, and supervised the study, led the data collection and qualitative synthesis, carried out the quantitative synthesis and final analyses, drafted and revised the final manuscript, and approved the final manuscript as submitted. SF collected data, carried out initial analyses, revised the final manuscript, and approved the final manuscript as submitted. SSN collected data, carried out initial analyses, revised the final manuscript, and approved the final manuscript as submitted. EL collected data, carried out initial analyses, revised the final manuscript, and approved the final manuscript as submitted. DMT conceptualized the study, oversaw the quantitative analysis, revised the final manuscript, and approved the final manuscript as submitted. LZ conceptualized the study, oversaw the qualitative analysis, revised the final manuscript, and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sabnis, A., Fojo, S., Nayak, S.S. et al. Reducing parental trauma and stress in neonatal intensive care: systematic review and meta-analysis of hospital interventions. J Perinatol 39, 375–386 (2019). https://doi.org/10.1038/s41372-018-0310-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0310-9
This article is cited by
-
Evaluation of the telemedical health care network “SAFE BIRTH” for pregnant women at risk, premature and sick newborns and their families: study protocol of a cluster-randomized controlled stepped-wedge trial
BMC Health Services Research (2024)
-
Care intervention on psychological outcomes among patients admitted to intensive care unit: an umbrella review of systematic reviews and meta-analyses
Systematic Reviews (2023)
-
Evaluation of parental stress in neonatal intensive care unit in Iran: a national study
BMC Nursing (2023)
-
Mindfulness and Relaxation-Based Interventions to Reduce Parental Stress, Anxiety and/or Depressive Symptoms in the Neonatal Intensive Care Unit: A Systematic Review
Journal of Clinical Psychology in Medical Settings (2023)
-
Protecting the infant-parent relationship: special emphasis on perinatal mood and anxiety disorder screening and treatment in neonatal intensive care unit parents
Journal of Perinatology (2022)