Abstract
Fetal growth restriction (FGR) affects about 5–10% pregnancies and is associated with poorer outcomes in the perinatal period. Additionally, long standing epidemiological data support its association with chronic diseases such as hypertension and diabetes. Cardiac and vascular adaptations in response to chronic hypoxemia due to utero-placental insufficiency are hallmarks of fetal adaptations. Investigators have attempted to identify these changes in the placenta at the microscopic and molecular level. The ex vivo dual perfusion model of the placenta enables the study of placental haemodynamics in growth-restricted pregnancies. Persistent arterial abnormalities (thickness and stiffness) noted on vascular ultrasound during fetal life through to the young-adult age group for those affected by FGR, seem to be a plausible link between in utero events and chronic circulatory diseases. Using these, this review reflects current thought on vascular maladaptive changes in the FGR cohorts and the role in investigating current and future therapeutics.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Rosenberg A. The IUGR newborn. Semin Perinatol. 2008;32:219–24.
Figueras F, Gratacós E. Update on the diagnosis and classification of fetal growth restriction and proposal of a stage-based management protocol. Fetal Diagn Ther. 2014;36:86–98.
Lees C, Marlow N, Arabin B, Bilardo CM, Brezinka C, Derks JB, et al. Perinatal morbidity and mortality in early-onset fetal growth restriction: cohort outcomes of the trial of randomized umbilical and fetal flow in Europe (TRUFFLE). Ultrasound Obstet Gynecol. 2013;42:400–8.
Martyn CN, Greenwald SE. Impaired synthesis of elastin in walls of aorta and large conduit arteries during early development as an initiating event in pathogenesis of systemic hypertension. Lancet. 1997;350:953–5.
Cheung YF, Taylor MJ, Fisk NM, Tsoi NS. Fetal origins of reduced arterial distensibility in the donor twin in twin-twin transfusion syndrome. Lancet. 2000;355:1157–8.
Dobrin PB. Mechanical properties of arteries. Physiol Rev. 1978;58:397–460.
Lurbe E, Torro MI, Carvajal E, Alvarez V, Redón J. Birth weight impacts on wave reflections in children and adolescents. Hypertension. 2003;41:646–50.
Sehgal A, Allison B, Gwini S, Menahem S, Miller S, Polglase G. Vascular aging and cardiac maladaptation in growth-restricted preterm infants. J Perinatol. 2018;38:92–97.
Sehgal A, Skilton MR, Crispi F. Human fetal growth restriction: a cardiovascular journey through to adolescence. J Dev Orig Health Dis. 2016;6:626–35.
Demicheva E, Crispi F. Long-term follow-up of intrauterine growth restriction: cardiovascular disorders. Fetal Diagn Ther. 2014;36:143–53.
Bradley TJ, Potts JE, Lee SK, Potts MT, De Souza AM, Sandor GG. Early changes in the biophysical properties of the aorta in pre-adolescent children born small for gestational age. J Pediatr. 2010;156:388–92.
Crispi F, Figueras F, Cruz-Lemini M, Bartrons J, Bijnens B, Gratacos E, et al. Cardiovascular programming in children born small for gestational age and relationship with prenatal signs of severity. Am J Obstet Gynecol. 2012;207:121.e1–.e9.
Miles KA, McDonnell BJ, Maki-Petaja KM, Cockcroft JR, Wilkinson IB, McEniery CM, et al. The impact of birth weight on blood pressure and arterial stiffness in later life: the Enigma Study. J Hypertens. 2011;29:2324–31.
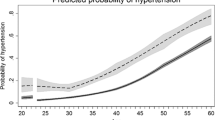
Gennser G, Rymark P, Isberg PE. Low birth weight and risk of high blood pressure in adulthood. Br Med J. 1988;296:1498–9.
Barker DJP, Osmond C, Golding J, Kuh D, Wadsworth MEJ. Growth in utero, blood pressure in childhood and adult life, and mortality from cardiovascular disease. Br Med J. 1989;298:564–7.
Chaddha V, Viero S, Huppertz B, Kingdom J. Developmental biology of the placenta and the origins of placental insufficiency. Semin Fetal Neonatal Med. 2004;9:357–69.
Sibley CP, Turner MA, Cetin I, Ayuk P, Boyd CA, D’Souza SW, et al. Placental phenotypes of intrauterine growth. Pediatr Res. 2005;58:827–32.
Kiserud T, Kessler J, Ebbing C, Rasmussen S. Ductus venosus shunting in growth-restricted fetuses and the effect of umbilical circulatory compromise. Ultrasound Obstet Gynecol. 2006;28:143–9.
Sala C, Campise M, Ambroso G, Motta T, Zanchetti A, Morganti A. Atrial natriuretic peptide and hemodynamic changes during normal human pregnancy. Hypertension. 1995;25:631–6.
Baschat AA. Pathophysiology of fetal growth restriction: implications for diagnosis and surveillance. Obstet Gynecol Surv. 2004;59:617–27.
Barker DJP. The fetal origins of adult hypertension. J Hypertens. 1992;10:S39–S44.
Folkow B. Physiological aspects of primary hypertension. Physiol Rev. 1982;62:347–504.
Sehgal A, Crispi F, Skilton M, De Boode W. Clinician performed ultrasound in fetal growth restriction: Fetal, neonatal, pediatric aspects. J Perinatol. 2017;37:1251–58.
Kingdom JCP, Kaufmann P. Oxygen and placental villous development: origins of fetal hypoxia. Placenta. 1997;18:613–21.
Mayhewa TM, Charnock-Jonesb DS, Kaufmannc P. Aspects of human fetoplacental vasculogenesis and angiogenesis: changes in complicated pregnancies. Placenta. 2004;25:127–39.
Khong TY, Mooney EE, Ariel I, Balmus NC, Boyd TK, Brundler MA, et al. Sampling and definitions of placental lesions amsterdam placental workshop group consensus statement. Arch Pathol Lab Med. 2016;140:698–713.
Salafia CM, Vintzileos AM, Silberman L, Bantham KF, Vogel CA. Placental pathology of idiopathic intrauterine growth retardation at term. Am J Perinatol. 1992;9:179–84.
Vedmedovska N, Rezeberga D, Teibe U, Melderis I, Donders GG. Placental pathology in fetal growth restriction. Eur J Obstet Gynecol Reprod Biol. 2011;155:36–40.
Mifsud W, Sebire NJF. Placental pathology in early-onset and late-onset fetal growth restriction. Fetal Diagn Ther. 2014;36:117–28.
Fox H, Sebire NJ. The placenta in abnormalities and disorders of the fetus. In: Fox H, Sebire NJ, editors. Pathology of the placenta: major problems in pathology. Vol. 7, 3 edn. Philadelphia: Saunders; 1991.
Sun CCJ, Revell VO, Belli AJ, Viscardi RM. Discrepancy in pathologic diagnosis of placental lesions. Arch Pathol Lab Med. 2002;126:706–9.
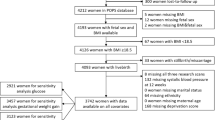
Sehgal A, Dahlstrom JE, Chan Y, Allison BJ, Miller SL, Polglase GR. Placental histopathology in preterm fetal growth restriction. J Paediatr Child Health. 2018. https://doi.org/10.1111/jpc.14251. [Epub ahead of print].
Salafia CM, Charles AK, Maas EM. Placenta and fetal growth restriction. Clin Obstet Gynecol. 2006;49:236–56.
Teasdale F. Idiopathic intrauterine growth retardation: histomorphometry of the human placenta. Placenta. 1984;5:83–92.
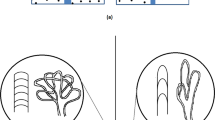
Kingdom J, Huppertz B, Seaward G, Kaufmann P. Development of the placental villous tree and its consequences for fetal growth. Eur J Obstet Gynecol Reprod Biol. 2000;92:35–43.
Junaid TO, Brownbill P, Chalmers N, Johnstone ED, Aplin JD. Fetoplacental vascular alterations associated with fetal growth restriction. Placenta. 2014;35:808–15.
Cotechini T, Hopman WJ, Graham CH. Inflammation-induced fetal growth restriction in rats is associated with altered placental morphometrics. Placenta. 2014;35:575–81.
Hagberg H, Gressens P, Mallard C. Inflammation during fetal and neonatal life: implications for neurologic and neuropsychiatric disease in children and adults. Ann Neurol. 2012;71:444–57.
Saji F, Samejima Y, Kamiura S, Sawai K, Shimoya K, Kimura T. Cytokine production in chorioamnionitis. J Reprod Immunol. 2000;47:185–96.
Lappas M, McCracken S, McKelvey K, Lim R, James J, Roberts CT, et al. Formyl peptide receptor-2 is decreased in foetal growth restriction and contributes to placental dysfunction. Mol Hum Reprod. 2018;24:94–109.
Harris LK. Could peptide-decorated nanoparticles provide an improved approach for treating pregnancy complications? Nanomedicine. 2016;11:2235–8.
King A, Ndifon C, Lui S, Widdows K, Kotamraju VR, Agemy L, et al. Tumor-homing peptides as tools for targeted delivery of payloads to the placenta. Sci Adv. 2016;2:e1600349.
Acharya G, Wilsgaard T, Berntsen GK, Maltau JM, Kiserud T. Doppler-derived umbilical artery absolute velocities and their relationship to fetoplacental volume blood flow: a longitudinal study. Ultrasound Obstet Gynecol. 2005;25:444–53.
Ghosh GS, Fu J, Olofsson P, Gudmundsson S. Pulsations in the umbilical vein during labor are associated with increased risk of operative delivery for fetal distress. Ultrasound Obstet Gynecol. 2009;34:177–81.
Turan S, Miller J, Baschat AA. Integrated testing and management in fetal growth restriction. Semin Perinatol. 2008;32:194–200.
Jones S, Bischof H, Lang I, Desoye G, Greenwood SL, Johnstone ED, et al. Dysregulated flow-mediated vasodilatation in the human placenta in fetal growth restriction. J Physiol. 2015;593:3077–92.
Kummu M, Sieppi E, Koponen J, Laatio L, Vähäkangas K, Kiviranta H, et al. Organic anion transporter 4 (OAT 4) modifies placental transfer of perfluorinated alkyl acids PFOS and PFOA in human placental ex vivo perfusion system. Placenta. 2015;36:1185–91.
Abumaree MH, Brownbill P, Burton G, Castillo C, Chamley L, Croy BA, et al. IFPA Meeting 2013 Workshop Report III: Maternal placental immunological interactions, novel determinants of trophoblast cell fate, dual ex vivo perfusion of the human placenta. Placenta. 2014;35:S15–19.
Brownbill P, Sebire N, McGillick EV, Ellery S, Murthi P. Ex vivo dual perfusion of the human placenta: disease simulation, therapeutic pharmacokinetics and analysis of off-target effects. Methods Mol Biol. 2018;1710:173–89.
Marzioni D, Tamagnone L, Capparuccia L, Marchini C, Amici A, Todros T, et al. Restricted innervation of uterus and placenta during pregnancy: evidence for a role of the repelling signal Semaphorin 3A. Dev Dyn. 2004;231:839–48.
Poston L. The control of blood flow to the placenta. Exp Physiol. 1997;82:377–87.
Bainbridge SA, Farley AE, McLaughlin BE, Graham CH, Marks GS, Nakatsu K, et al. Carbon monoxide decreases perfusion pressure in isolated human placenta. Placenta. 2002;23:563–9.
Cindrova-Davies T, Herrera EA, Niu Y, Kingdom J, Giussani DA, Burton GJ. Reduced cystathionine gamma-lyase and increased miR-21 expression are associated with increased vascular resistance in growth-restricted pregnancies: hydrogen sulfide as a placental vasodilator. Am J Pathol. 2013;182:1448–58.
Kulandavelu S, Whiteley KJ, Qu D, Mu J, Bainbridge SA, Adamson SL. Endothelial nitric oxide synthase deficiency reduces uterine blood flow, spiral artery elongation, and placental oxygenation in pregnant mice. Hypertension. 2012;60:231–8.
Magness RR, Shaw CE, Phernetton TM, Zheng J, Bird IM. Endothelial vasodilator production by uterine and systemic arteries. II. Pregnancy effects on NO synthase expression. Am J Physiol Heart Circ Physiol. 1997;272:H1730–H1740.
Wang X, Athayde N, Trudinger B. Maternal plasma from pregnant women with umbilical placental vascular disease does not affect endothelial cell mRNA expression of nitric oxide synthase. J Soc Gynecol Investig. 2004;11:149–53.
Kingdom JC, McQueen J, Connell JM, Whittle MJ. Fetal angiotensin II levels and vascular (type I) angiotensin receptors in pregnancies complicated by intrauterine growth retardation. Br J Obstet Gynaecol. 1993;100:476–82.
Brownbill P, Sibley CP. Regulation of transplacental water transfer: the role of fetoplacental venous tone. Placenta. 2006;27:560–7.
Rodríguez-López M, Cruz-Lemini M, Valenzuela-Alcaraz B, Garcia-Otero L, Sitges M, Bijnens B, et al. Descriptive analysis of the different phenotypes of cardiac remodelling in fetal growth restriction. Ultrasound Obstet Gynecol. 2017;50:207–14.
Veronese E, Tarroni G, Visentin S, Cosmi E, Linguraru MG, Grisan E. Estimation of prenatal aorta intima-media thickness from ultrasound examination. Phys Med Biol. 2014;59:6355–71.
Berry CL, Looker T. An alteration in the chemical structure of the aortic wall induced by a finite period of growth inhibition. J Anat. 1973;114:83–94.
Clarenbach CF, Thurnheer R, Kohler M. Vascular dysfunction in chronic obstructive pulmonary disease: current evidence and perspectives. Expert Rev Respir Med. 2012;6:37–43.
Polglase GR, Allison BJ, Coia E, Li A, Jenkin G, Malhotra A, et al. Altered cardiovascular function at birth in growth-restricted preterm lambs. Pediatr Res. 2016;80:538–46.
Mahomed FA. Remarks on arterio-capillary fibrosis and its clinical recognition. Lancet. 1877;110:232–4.
Akira M, Yoshiyuki S. Placental circulation, fetal growth and stiffness of the abdominal aorta in newborn infants. J Pediatr. 2006;148:49–53.
Boutouyrie P, Tropeano AI, Asmar R, Gautier I, Benetos A, Lacolley P, et al. Aortic stiffness is an independent predictor of primary coronary events in hypertensive patients: a longitudinal study. Hypertension. 2002;39:10–15.
Takenaka T, Mimura T, Kanno Y, Suzuki H. Quantification of arterial stiffness as a risk factor to the progression of chronic kidney diseases. Am J Nephrol. 2005;25:417–24.
Zanardo V, Visentin S, Bertin M, Zaninotto M, Trevisanuto D, Cavallin F, et al. Aortic wall thickness and amniotic fluid albuminuria in growth-restricted twin fetuses. Twin Res Hum Genet. 2013;16:720–6.
Zanardo V, Fanelli T, Weiner G, Fanos V, Zaninotto M, Visentin S. Intrauterine growth restriction is associated with persistent aortic wall thickening and glomerular proteinuria during infancy. Kidney Int. 2011;80:119–23.
Sehgal A, Gwini SM, Menahem S, Allison BJ, Miller SL, Polglase GR. Preterm growth restriction and bronchopulmonary dysplasia: the vascular hypothesis and related physiology. J Physiol. 2018. https://doi.org/10.1113/JP276040.
Costa EJ, Lopes RH, Lamy-Freund MT. Permeability of pure lipid bilayers to melatonin. J Pineal Res. 1995;19:123–6.
Hung MW, Yeung HM, Lau CF, Poon AMS, Tipoe GL, Fung ML. Melatonin attenuates pulmonary hypertension in chronically hypoxic rats. Int J Mol Sci. 2017;18:1125–35.
Thebaud B, Abman SH. Bronchopulmonary dysplasia: where have all the vessels gone? Roles of angiogenic growth factors in chronic lung disease. Am J Respir Crit Care Med. 2007;175:978–85.
Thebaud B, Ladha F, Michelakis ED, Sawicka M, Thurston G, Eaton F, et al. Vascular endothelial growth factor gene therapy increases survival, promotes lung angiogenesis, and prevents alveolar damage in hyperoxia induced lung injury: evidence that angiogenesis participates in alveolarization. Circulation. 2005;112:2477–86.
McGillick EV, Orgeig S, Morrison JL. Structural and molecular regulation of lung maturation by intratracheal VEGF administration in the normally grown and placentally restricted fetus. J Physiol. 2015;594:1399–420.
Rodriguez-Lopez M, Osorio L, Acosta-Rojas R, Figueras J, Cruz-Lemini M, Figueras F, et al. Influence of breastfeeding and postnatal nutrition on cardiovascular remodeling induced by fetal growth restriction. Pediatr Res. 2016;79:100–6.
Skilton MR, Ayer JG, Harmer JA, Webb K, Leeder SR, Marks GB, et al. Impaired fetal growth and arterial wall thickening. A randomized trial of omega-3 supplementation. Pediatrics. 2012;129:e698.
Dilworth MR, Andersson I, Renshall LJ, Cowley E, Baker P, Greenwood S, et al. Sildenafil increased fetal weight in a mouse model of FGR with a normal vascular phenotype. PLoS ONE. 2013;30:e77748. 8
Paauw ND, Terstappen F, Ganzevoort W, Joles JA, Gremmels H, Lely AT. Sildenafil during pregnancy: a preclinical meta-analysis on fetal growth and maternal blood pressure. Hypertension. 2017;70:998–1006.
Sharp A, Cornforth C, Jackson R, Harrold J, Turner MA, Kenny LC, et al. Maternal sildenafil for severe fetal growth restriction (STRIDER): a multicentre, randomised, placebo-controlled, double-blind trial. Lancet Child Adolesc Health. 2017;1016:S2352–4642.
Groom K, et al. 5PDE Inhibitors for Fetal Growth Restriction, the STRIDER Consortium and STRIDER NZAus. Perinatal Society of Australia and New Zealand Annual Meeting 2018.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Sehgal, A., Murthi, P. & Dahlstrom, J.E. Vascular changes in fetal growth restriction: clinical relevance and future therapeutics. J Perinatol 39, 366–374 (2019). https://doi.org/10.1038/s41372-018-0287-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0287-4
This article is cited by
-
Cardiac morphology in neonates with fetal growth restriction
Journal of Perinatology (2023)
-
Role of prenatal fetal echocardiography in the assessment of intrauterine growth restriction
Egyptian Journal of Radiology and Nuclear Medicine (2022)
-
Expression and DNA Methylation Status of the Imprinted Genes PEG10 and L3MBTL1 in the Umbilical Cord Blood and Placenta of the Offspring of Assisted Reproductive Technology
Reproductive Sciences (2021)