Abstract
Objectives
To evaluate the impact of congenital solitary functioning kidney (CSFK) length, measured early in life, on the eGFR levels during the follow-up.
Study design
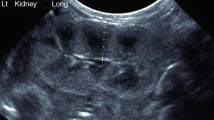
We retrospectively selected 162 CSFK patients undergoing, within 60 days of life, renal length (RL) measurement by ultrasound.
We divided the population in:
-
Group 1 = RL ≥ 2 standard deviation score (SDS).
-
Group 2 = RL < 2 SDS and showing RL ≥ 2 SDS during the follow-up.
-
Group 3 = RL < 2 SDS and showing RL < 2 SDS during the follow-up.
Primary outcome: development of eGFR below the range of normality.
Results
The median follow-up period of the overall population was 6.2 years (range 2–21.5 years). The cumulative proportion of patients free of primary outcome at 15 years of age was 96.4% in group 1, 64.6% in group 2, and 45.6% in group 3 (p = 0.03).
The RL > 2 SDS within 60 days of life was a significant protective factor (hazard ratio = 0.13; 95% C.I. 0.02–0.97) against development of primary outcome.
Conclusion
RL ≥ 2 SDS within 60 days of life could identify a population of CSFK with reduced risk of presenting reduced eGFR levels later in life.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Westland R, Schreuder MF, Bökenkamp A, Spreeuwenberg MD, Van Wijk JAE. Renal injury in children with a solitary functioning kidney-the KIMONO study. Nephrol Dial Transplant. 2011;26:1533–41.
Schreuder MF. Life with one kidney. Pediatr Nephrol. 2018;33:595–604.
van Vuuren SH, van der Doef R, Cohen-Overbeek TE, Goldschmeding R, Pistorius LR, de Jong TPVM. Compensatory enlargement of a solitary functioning kidney during fetal development. Ultrasound Obstet Gynecol. 2012;40:665–8.
Sammut S, Behr L, Hekmati M, Gubler MC, Laborde K, Lelièvre Pégorier M. Compensatory renal growth after unilateral or subtotal nephrectomy in the ovine fetus. Pediatr Res. 2013;74:624–32.
Douglas-Denton R, Moritz KM, Bertram JF, Wintour EM. Compensatory renal growth after unilateral nephrectomy in the ovine fetus. J Am Soc Nephrol. 2002;13:406–10.
Marzuillo P, Guarino S, Grandone A, Di Somma A, Della Vecchia N, Esposito T. et al. Outcomes of a cohort of prenatally diagnosed and early enrolled patients with congenital solitary functioning kidney. J Urol. 2017;198:1153–8.
Westland R, Schreuder MF, Ket JCF, van Wijk JAE. Unilateral renal agenesis: a systematic review on associated anomalies and renal injury. Nephrol Dial Transplant. 2013;28:1844–55.
Hains DS, Bates CM, Ingraham S, Schwaderer AL. Management and etiology of the unilateral multicystic dysplastic kidney: a review. Pediatr Nephrol. 2009;24:233–41.
La Scola C, Ammenti A, Puccio G, Lega MV, De Mutiis C, Guiducci C, et al. Congenital solitary kidney in children: size matters. J Urol. 2016;196:1250–6.
Westland R, Kurvers RAJ, van Wijk JAE, Schreuder MF. Risk factors for renal injury in children with a solitary functioning kidney. Pediatrics. 2013;131:e478–85.
Zhang Z, Quinlan J, Hoy W, Hughson MD, Lemire M, Hudson T, et al. A common RET variant is associated with reduced newborn kidney size and function. J Am Soc Nephrol. 2008;19:2027–34.
Widjaja E, Oxtoby JW, Hale TL, Jones PW, Harden PN, McCall IW. Ultrasound measured renal length versus low dose CT volume in predicting single kidney glomerular filtration rate. Br J Radiol. 2004;77:759–64.
Schwartz GJ, Brion LP, Spitzer A. The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children, and adolescents. Pediatr Clin North Am. 1987;34:571–90.
Srivastava T, Alon US, Althahabi R, Garg U. Impact of standardization of creatinine methodology on the assessment of glomerular filtration rate in children. Pediatr Res. 2009;65:113–6.
Rosenbaum DM, Korngold E, Teele RL. Sonographic assessment of renal length in normal children. Am J Roentgenol. 1983;142:467–9.
Schwartz GJ, Furth SL. Glomerular filtration rate measurement and estimation in chronic kidney disease. Pediatr Nephrol. 2007;22:1839–48.
Schwartz GJ, Work DF. Measurement and estimation of GFR in children and adolescents. Clin J Am Soc Nephrol. 2009;4:1832–43.
Helal I, Fick-Brosnahan GM, Reed-Gitomer B, Schrier RW. Glomerular hyperfiltration: definitions, mechanisms and clinical implications. Nat Rev Nephrol. 2012;8:293–300.
Jeon HG, Lee SR, Joo DJ, Oh YT, Kim MS, Kim YS, et al. Predictors of kidney volume change and delayed kidney function recovery after donor nephrectomy. J Urol. 2010;184:1057–63.
Lenihan CR, Busque S, Derby G, Blouch K, Myers BD, Tan JC. Longitudinal study of living kidney donor glomerular dynamics after nephrectomy. J Clin Invest. 2015;125:1311–8.
Schreuder MF. Safety in glomerular numbers. Pediatr Nephrol. 2012;27:1881–7.
Acknowledgements
The authors thank Anna Carella and Simona Malvone for reviewing the English language of this manuscript.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Marzuillo, P., Guarino, S., Grandone, A. et al. Congenital solitary kidney size at birth could predict reduced eGFR levels later in life. J Perinatol 39, 129–134 (2019). https://doi.org/10.1038/s41372-018-0260-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0260-2
This article is cited by
-
Predicting outcomes in children with congenital anomalies of the kidney and urinary tract
Pediatric Nephrology (2023)
-
Kidney length standardized to body length predicts outcome in infants with a solitary functioning kidney
Pediatric Nephrology (2023)
-
Evolution of congenital anomalies of urinary tract in children with and without solitary kidney
Pediatric Research (2022)
-
Management of the congenital solitary kidney: consensus recommendations of the Italian Society of Pediatric Nephrology
Pediatric Nephrology (2022)
-
Risk stratification for children with a solitary functioning kidney
Pediatric Nephrology (2021)