Abstract
Background:
Asphyxiated infants treated with therapeutic cooling can have persistent oral feeding difficulty because of involvement of neural pathways in the brainstem, cortex, and basal ganglia. The goal is to predict the composite adverse outcome of death or persistent oral feeding difficulty using precooling/cooling attributes, and the severity and distribution of hypoxic–ischemic lesions, especially brainstem lesions on post-cooling brain magnetic resonance imaging (MRI).
Methods:
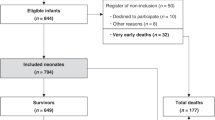
Retrospective review of 86 asphyxiated infants cooled from January 2006 to August 2014. Persistent feeding difficulty was defined as needing feeding support (gastrostomy tube (g-tube) or home gavage feeds) after discharge. Clinical and laboratory risk factors, and the brain MRI abnormalities including the presence of brainstem lesions were compared between infants with and without adverse outcome using univariate analysis. Significant variables were then analyzed in a stepwise logistic regression (LR) model.
Results:
Infants with adverse outcome (n = 31, 4 died pre-discharge) had longer hospital stay (26 days, interquartile range (IQR) 19–43 vs. 13 days, IQR 9–20; p < 0.01) and reached goal enteral feeds (oral/gavage) later (11 days vs. 8 days, p < 0.01) compared to 55 infants discharged on full oral feeds. The former infants were more likely to have cord pH ≤ 7.15, severely abnormal neurological examination, bleeding diathesis, continued need for ventilation, and positive MRI findings including brainstem lesions. In LR analysis, brainstem lesions on MRI (p = 0.00, odds ratio 19, 95% confidence interval 4–85) was independently associated with the adverse outcome.
Conclusions:
Brainstem involvement on post-cooling brain MRI was predictive of adverse outcome. Early identification of these infants may facilitate discussion of home feeding plans between clinicians and parents earlier, thereby potentially reducing the length of hospital stay.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Nelson KB, Ellenberg JH. The asymptomatic newborn and risk of cerebral palsy. Am J Dis Child. 1987;141:1333–5.
Sarkar S, Bhagat I, Bapuraj JR, Dechert RE, Donn SM. Does clinical status 1 week after therapeutic hypothermia predict brain MRI abnormalities? J Perinatol. 2013;33:538–42.
Shankaran S, Laptook A, Wright LL, Ehrenkranz RA, Donovan EF, Fanaroff AA, et al. Whole-body hypothermia for neonatal encephalopathy: animal observations as a basis for a randomized, controlled pilot study in term infants. Pediatrics. 2002;110:377–85.
Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, et al. Whole body hypothermia for neonates with hypoxic–ischemic encephalopathy. N Engl J Med. 2005;353:1574–84.
Jacobs SE, Morley CJ, Inder TE, Stewart MJ, Smith KR, McNamara PJ, et al. Whole-body hypothermia for term and near-term newborns with hypoxic–ischemic encephalopathy: a randomized controlled trial. Arch Pediatr Adolesc Med. 2011;165:692–700.
Martinez-Biarge M, Diez-Sebastian J, Wushhoff CJ, Lawrence S, Aloysius A, Rutherford MA, et al. Feeding and communication impairments in infants with central gray matter lesions following perinatal hypoxic–ischaemic injury. Eur J Paediatr Neurol. 2012;16:688–96.
Jacobs SE, Berg M, Hunt R, Tarnow-Mordi WO, Inder TE, Davis PG. Cooling for newborns with hypoxic–ischemic encephalopathy. Cochrane Database Syst Rev. 2013;1:CD003311.
Gluckman PD, Wyatt JS, Azzopardi D, Ballard R, Edwards AD, Ferriero DM, et al. Selective head cooling with mild hypothermia after neonatal encephalopathy: multicentre randomised trial. Lancet. 2005;365:663–70.
Sarkar S, Donn SM, Bapuraj JR, Bhagat I, Barks JD. Distribution and severity of hypoxic–ischemic lesions on brain MRI following therapeutic cooling: selective head versus whole body cooling. Arch Dis Child Fetal Neonatol Ed. 2012;97:F335–F339.
Barkovich AJ, Hajnal BL, Vigneron D, Sola A, Patridge JC, Allen F, et al. Prediction of neuromotor outcome in perinatal asphyxia: evaluation of MR scoring systems. Am J Neuroradiol. 1998;19:143–9.
Ambalavanan N, Carlo WA, Shankaran S, Bann CM, Emrich SL, Higgins RD, et al. National Institute of Child Health and Human Development Neonatal Research Network. Predicting outcomes of neonates diagnosed with hypoxemic–ischemic encephalopathy. Pediatrics. 2006;118:2084–93.
Sarkar S, Barks JD, Bapuraj JR, Bhagat I, Dechert RE, Schumacher RE, et al. Does phenobarbital improve the effectiveness of therapeutic hypothermia in infants with hypoxic–ischemic encephalopathy? J Perinatol. 2012;32:15–20.
Sarkar S, Donn SM, Bapuraj JR, Bhagat I, Dechert RE, Barks JD. The relationship between clinically identifiable intrapartum sentinel events and short-term outcome after therapeutic hypothermia. J Pediatr. 2011;159:726–30.
Barkovich AJ, Westmark K, Partridge C, Sola A, Ferriero DM. Perinatal asphyxia: MR findings in the first 10 days. Am J Neuroradiol. 1995;16:427–38.
Rutherford M, Ramenghi LA, Edwards AD, Brocklehurst P, Halliday H, Levene M, et al. Assessment of brain tissue injury after moderate hypothermia in neonates with hypoxic–ischaemic encephalopathy: a nested subset of a randomised control trial. Lancet Neurol. 2010;9:39–45.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Gupta, S., Bapuraj, J.R., Carlson, G. et al. Predicting the need for home gavage or g-tube feeds in asphyxiated neonates treated with therapeutic hypothermia. J Perinatol 38, 728–733 (2018). https://doi.org/10.1038/s41372-018-0080-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0080-4
This article is cited by
-
Predictive value of the Thompson score for short-term adverse outcomes in neonatal encephalopathy
Pediatric Research (2023)
-
Brainstem hypoxic–ischemic lesions on MRI in infants treated with therapeutic cooling: effects on the length of stay and mortality
Journal of Perinatology (2021)