Abstract
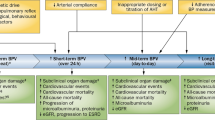
Blood pressure (BP) is a physiological parameter with short- and long-term variability caused by complex interactions between intrinsic cardiovascular (CV) mechanisms and extrinsic environmental and behavioral factors. Available evidence suggests that not only mean BP values are important, but also BP variability (BPV) might contribute to CV events. Labile hypertension (HTN) is referred to sudden rises in BP and it seems to be linked with unfavorable outcomes. The aim of this article was to review and summarize recent evidence on BPV phenomenon, unraveling the labile HTN concept along with the prognostic value of these conditions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Parati G, Ochoa JE, Lombardi C, Bilo G. Assessment and management of blood-pressure variability. Nat Rev Cardiol. 2013;10:143–55.
Floras JS. Blood pressure variability: a novel and important risk factor. Can J Cardiol. 2013;29:557–63.
Mann SJ. The clinical spectrum of labile hypertension: a management dilemma. J Clin Hypertens (Greenwich). 2009;11:491–7.
Eich RH, Cuddy RP, Smulyan H, Lyons RH. Hemodynamics in labile hypertension. A follow-up study. Circulation. 1966;34:299–307.
Tsioufis C. Blood pressure variability and cardiovascular prognosis. Many expectations but limited data. Hell J Cardiol. 2017;58:465–7.
Whelton PK, Carey RM, Aronow WS, Casey DE, Jr., Collins KJ, Dennison Himmelfarb C, et al.: 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017;71:1269–1324.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. Group ESCSD: 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Metoki H, Ohkubo T, Kikuya M, Asayama K, Obara T, Hashimoto J, et al. Prognostic significance for stroke of a morning pressor surge and a nocturnal blood pressure decline: the Ohasama study. Hypertension. 2006;47:149–54.
Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens. 2002;20:2183–9.
Kario K, Pickering TG, Umeda Y, Hoshide S, Hoshide Y, Morinari M, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003;107:1401–6.
Sheppard JP, Hodgkinson J, Riley R, Martin U, Bayliss S, McManus RJ. Prognostic significance of the morning blood pressure surge in clinical practice: a systematic review. Am J Hypertens. 2015;28:30–41.
Kario K, Pickering TG, Matsuo T, Hoshide S, Schwartz JE, Shimada K. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension. 2001;38:852–7.
de la Sierra A, Gorostidi M, Banegas JR, Segura J, de la Cruz JJ, Ruilope LM. Nocturnal hypertension or nondipping: which is better associated with the cardiovascular risk profile? Am J Hypertens. 2014;27:680–7.
Zweiker R, Eber B, Schumacher M, Toplak H, Klein W. “Non-dipping” related to cardiovascular events in essential hypertensive patients. Acta Med Austria. 1994;21:86–9.
Hoshide S, Kario K, Hoshide Y, Umeda Y, Hashimoto T, Kunii O, et al. Associations between nondipping of nocturnal blood pressure decrease and cardiovascular target organ damage in strictly selected community-dwelling normotensives. Am J Hypertens. 2003;16:434–8.
Cuspidi C, Sala C, Tadic M, Rescaldani M, Grassi G, Mancia G. Non-dipping pattern and subclinical cardiac damage in untreated hypertension: a systematic review and meta-analysis of echocardiographic studies. Am J Hypertens. 2015;28:1392–402.
Amodeo C, Guimaraes GG, Picotti JC, dos Santos CC, Bezzerra Fonseca KD, Matins RF, et al. Morning blood pressure surge is associated with death in hypertensive patients. Blood Press Monit. 2014;19:199–202.
Bombelli M, Fodri D, Toso E, Macchiarulo M, Cairo M, Facchetti R, et al. Relationship among morning blood pressure surge, 24-hour blood pressure variability, and cardiovascular outcomes in a white population. Hypertension. 2014;64:943–50.
Pierdomenico SD, Pierdomenico AM, Cuccurullo F. Morning blood pressure surge, dipping, and risk of ischemic stroke in elderly patients treated for hypertension. Am J Hypertens. 2014;27:564–70.
Wei FF, Li Y, Zhang L, Xu TY, Ding FH, Wang JG, et al. Beat-to-beat, reading-to-reading, and day-to-day blood pressure variability in relation to organ damage in untreated Chinese. Hypertension. 2014;63:790–6.
Oishi E, Ohara T, Sakata S, Fukuhara M, Hata J, Yoshida D, et al. Day-to-day blood pressure variability and risk of dementia in a general japanese elderly population: the Hisayama Study. Circulation. 2017;136:516–25.
Wang J, Shi X, Ma C, Zheng H, Xiao J, Bian H, et al. Visit-to-visit blood pressure variability is a risk factor for all-cause mortality and cardiovascular disease: a systematic review and meta-analysis. J Hypertens. 2017;35:10–7.
Xia Y, Liu X, Wu D, Xiong H, Ren L, Xu L, et al. Influence of beat-to-beat blood pressure variability on vascular elasticity in hypertensive population. Sci Rep. 2017;7:8394.
Olbers J, Gille A, Ljungman P, Rosenqvist M, Ostergren J, Witt N. High beat-to-beat blood pressure variability in atrial fibrillation compared to sinus rhythm. Blood Press. 2018;27:249–55.
Millar-Craig MW, Bishop CN, Raftery EB. Circadian variation of blood-pressure. Lancet. 1978;1:795–7.
Metoki H, Ohkubo T, Kikuya M, Asayama K, Obara T, Hara A, et al. Prognostic significance of night-time, early morning, and daytime blood pressures on the risk of cerebrovascular and cardiovascular mortality: the Ohasama Study. J Hypertens. 2006;24:1841–8.
Verdecchia P, Schillaci G, Guerrieri M, Gatteschi C, Benemio G, Boldrini F, et al. Circadian blood pressure changes and left ventricular hypertrophy in essential hypertension. Circulation. 1990;81:528–36.
Verdecchia P, Schillaci G, Gatteschi C, Zampi I, Battistelli M, Bartoccini C, et al. Blunted nocturnal fall in blood pressure in hypertensive women with future cardiovascular morbid events. Circulation. 1993;88:986–92.
Ben-Dov IZ, Kark JD, Ben-Ishay D, Mekler J, Ben-Arie L, Bursztyn M. Predictors of all-cause mortality in clinical ambulatory monitoring: unique aspects of blood pressure during sleep. Hypertension. 2007;49:1235–41.
Israel S, Israel A, Ben-Dov IZ, Bursztyn M. The morning blood pressure surge and all-cause mortality in patients referred for ambulatory blood pressure monitoring. Am J Hypertens. 2011;24:796–801.
Verdecchia P, Angeli F, Mazzotta G, Garofoli M, Ramundo E, Gentile G, et al. Day-night dip and early-morning surge in blood pressure in hypertension: prognostic implications. Hypertension. 2012;60:34–42.
Hoshide S, Yano Y, Mizuno H, Kanegae H, Kario K. Day-by-day variability of home blood pressure and incident cardiovascular disease in clinical practice: the J-HOP Study (Japan Morning Surge-Home Blood Pressure). Hypertension. 2018;71:177–84.
Stevens SL, Wood S, Koshiaris C, Law K, Glasziou P, Stevens RJ, et al. Blood pressure variability and cardiovascular disease: systematic review and meta-analysis. BMJ. 2016;354:i4098.
Rothwell PM, Howard SC, Dolan E, O’Brien E, Dobson JE, Dahlof B, et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet. 2010;375:895–905.
Chang TI, Reboussin DM, Chertow GM, Cheung AK, Cushman WC, Kostis WJ, et al. Group* SR: visit-to-visit office blood pressure variability and cardiovascular outcomes in SPRINT (Systolic Blood Pressure Intervention Trial). Hypertension. 2017;70:751–8.
McMullan CJ, Lambers Heerspink HJ, Parving HH, Dwyer JP, Forman JP, de Zeeuw D. Visit-to-visit variability in blood pressure and kidney and cardiovascular outcomes in patients with type 2 diabetes and nephropathy: a post hoc analysis from the RENAAL study and the Irbesartan Diabetic Nephropathy Trial. Am J Kidney Dis. 2014;64:714–22.
Yeh CH, Yu HC, Huang TY, Huang PF, Wang YC, Chen TP, et al. The risk of diabetic renal function impairment in the first decade after diagnosed of diabetes mellitus is correlated with high variability of visit-to-visit systolic and diastolic blood pressure: a case control study. BMC Nephrol. 2017;18:99.
Chia YC, Lim HM, Ching SM: Long-term visit-to-visit blood pressure variability and renal function decline in patients with hypertension over 15 years. J Am Heart Assoc. 2016;5: pii: e003825.
Yokota K, Fukuda M, Matsui Y, Hoshide S, Shimada K, Kario K. Impact of visit-to-visit variability of blood pressure on deterioration of renal function in patients with non-diabetic chronic kidney disease. Hypertens Res. 2013;36:151–7.
Gosmanova EO, Mikkelsen MK, Molnar MZ, Lu JL, Yessayan LT, Kalantar-Zadeh K, et al. Association of systolic blood pressure variability with mortality, coronary heart disease, stroke, and renal disease. J Am Coll Cardiol. 2016;68:1375–86.
Whittle J, Lynch AI, Tanner RM, Simpson LM, Davis BR, Rahman M, et al. Visit-to-Visit Variability of BP and CKD Outcomes: results from the ALLHAT. Clin J Am Soc Nephrol. 2016;11:471–80.
Yano Y, Fujimoto S, Kramer H, Sato Y, Konta T, Iseki K, et al. Long-term blood pressure variability, new-onset diabetes mellitus, and new-onset chronic kidney disease in the japanese general population. Hypertension. 2015;66:30–6.
Yokota K, Fukuda M, Matsui Y, Kario K, Kimura K. Visit-to-visit variability of blood pressure and renal function decline in patients with diabetic chronic kidney disease. J Clin Hypertens (Greenwich). 2014;16:362–6.
Ricci F, De Caterina R, Fedorowski A. Orthostatic hypotension: epidemiology, prognosis, and treatment. J Am Coll Cardiol. 2015;66:848–60.
Fedorowski A, Engstrom G, Hedblad B, Melander O. Orthostatic hypotension predicts incidence of heart failure: the Malmo preventive project. Am J Hypertens. 2010;23:1209–15.
Fedorowski A, Hedblad B, Engstrom G, Gustav Smith J, Melander O. Orthostatic hypotension and long-term incidence of atrial fibrillation: the Malmo Preventive Project. J Intern Med. 2010;268:383–9.
Voichanski S, Grossman C, Leibowitz A, Peleg E, Koren-Morag N, Sharabi Y, et al. Orthostatic hypotension is associated with nocturnal change in systolic blood pressure. Am J Hypertens. 2012;25:159–64.
Bilo G, Giglio A, Styczkiewicz K, Caldara G, Maronati A, Kawecka-Jaszcz K, et al. A new method for assessing 24-h blood pressure variability after excluding the contribution of nocturnal blood pressure fall. J Hypertens. 2007;25:2058–66.
Mena L, Pintos S, Queipo NV, Aizpurua JA, Maestre G, Sulbaran T. A reliable index for the prognostic significance of blood pressure variability. J Hypertens. 2005;23:505–11.
Kannel WB, Sorlie P, Gordon T. Labile hypertension: a faulty concept? The Framingham study. Circulation. 1980;61:1183–7.
Julius S, Schork MA. Borderline hypertension--a critical review. J Chronic Dis. 1971;23:723–54.
Nedostup AV, Fedorova VI, Dmitriev KV. [Labile hypertension in elderly: clinical features, autonomic regulation of circulation, approaches to treatment]. Klin Med (Mosk). 2000;78:27–32.
Migneco A, Ojetti V, Covino M, Mettimano M, Montebelli MR, Leone A, et al. Increased blood pressure variability in menopause. Eur Rev Med Pharmacol Sci. 2008;12:89–95.
Ma RC, Yiu KH, Wong EH, Liu KH, Chan JY, Chow CC, et al. A man with labile blood pressure. PLoS Med. 2007;4:e111.
Robertson D, Hollister AS, Biaggioni I, Netterville JL, Mosqueda-Garcia R, Robertson RM. The diagnosis and treatment of baroreflex failure. N Engl J Med. 1993;329:1449–55.
Heusser K, Tank J, Luft FC, Jordan J. Baroreflex failure. Hypertension. 2005;45:834–9.
Kuchel O, Cuche JL, Hamet P, Tolis G, Messerli FH, Barbeau A, et al. Labile (borderline) hypertension--new aspects of a common disorder. Angiology. 1975;26:619–31.
Julius S, Nesbitt S. Sympathetic overactivity in hypertension. A moving target. Am J Hypertens. 1996;9:113S–20S.
Kotsis V, Stabouli S, Karafillis I, Papakatsika S, Rizos Z, Miyakis S, et al. Arterial stiffness and 24 h ambulatory blood pressure monitoring in young healthy volunteers: the early vascular ageing Aristotle University Thessaloniki Study (EVA-ARIS Study). Atherosclerosis. 2011;219:194–9.
Mancia G. Short- and long-term blood pressure variability: present and future. Hypertension. 2012;60:512–7.
Mancia G, Parati G, Pomidossi G, Casadei R, Di Rienzo M, Zanchetti A. Arterial baroreflexes and blood pressure and heart rate variabilities in humans. Hypertension. 1986;8:147–53.
Parati G, Faini A, Valentini M. Blood pressure variability: its measurement and significance in hypertension. Curr Hypertens Rep. 2006;8:199–204.
Sanidas E, Papadopoulos DP, Grassos H, Velliou M, Tsioufis K, Barbetseas J, et al. Air pollution and arterial hypertension. A new risk factor is in the air. J Am Soc Hypertens. 2017;11:709–15.
Parati G, Bilo G. Calcium antagonist added to angiotensin receptor blocker: a recipe for reducing blood pressure variability?: evidence from day-by-day home blood pressure monitoring. Hypertension. 2012;59:1091–3.
Modesti PA, Morabito M, Bertolozzi I, Massetti L, Panci G, Lumachi C, et al. Weather-related changes in 24-hour blood pressure profile: effects of age and implications for hypertension management. Hypertension. 2006;47:155–61.
Deedwania PC, Nelson JR. Pathophysiology of silent myocardial ischemia during daily life. Hemodynamic evaluation by simultaneous electrocardiographic and blood pressure monitoring. Circulation. 1990;82:1296–304.
Rehman A, Zalos G, Andrews NP, Mulcahy D, Quyyumi AA. Blood pressure changes during transient myocardial ischemia: insights into mechanisms. J Am Coll Cardiol. 1997;30:1249–55.
Wingfield D, Grodzicki T, Palmer AJ, Wells F, Bulpitt CJ. General Practice Hypertension Study G: transiently elevated diastolic blood pressure is associated with a gender-dependent effect on cardiovascular risk. J Hum Hypertens. 2005;19:347–54.
Peters R, Wells F, Bulpitt C, Beckett N. Impact of transiently elevated diastolic pressure on cause of death: 29-year follow-up from the General Practice Hypertension Study Group. J Hypertens. 2013;31:71–6.
Sideris DA, Kontoyannis DA, Michalis L, Adractas A, Moulopoulos SD. Acute changes in blood pressure as a cause of cardiac arrhythmias. Eur Heart J. 1987;8:45–52.
Zuber SM, Kantorovich V, Pacak K. Hypertension in pheochromocytoma: characteristics and treatment. Endocrinol Metab Clin North Am. 2011;40:295–311. vii
Manger WM. The protean manifestations of pheochromocytoma. Horm Metab Res. 2009;41:658–63.
Mann SJ. Severe paroxysmal hypertension (pseudopheochromocytoma): understanding the cause and treatment. Arch Intern Med. 1999;159:670–4.
Mann SJ. Severe paroxysmal hypertension (pseudopheochromocytoma). Curr Hypertens Rep. 2008;10:12–8.
Sharabi Y, Goldstein DS, Bentho O, Saleem A, Pechnik S, Geraci MF, et al. Sympathoadrenal function in patients with paroxysmal hypertension: pseudopheochromocytoma. J Hypertens. 2007;25:2286–95.
Garcha AS, Cohen DL. Catecholamine excess: pseudopheochromocytoma and beyond. Adv Chronic Kidney Dis. 2015;22:218–23.
Le HM, Carbutti G, Ilisei D, Bouccin E, Vandemergel X. Pseudopheochromocytoma associated with domestic assault. Case Rep Cardiol. 2016;2016:6580215.
Gustavsen PH, Hoegholm A, Bang LE, Kristensen KS. White coat hypertension is a cardiovascular risk factor: a 10-year follow-up study. J Hum Hypertens. 2003;17:811–7.
Ugajin T, Hozawa A, Ohkubo T, Asayama K, Kikuya M, Obara T, et al. White-coat hypertension as a risk factor for the development of home hypertension: the Ohasama study. Arch Intern Med. 2005;165:1541–6.
Cuspidi C, Sala C, Grassi G, Mancia G. White coat hypertension: to treat or not to treat? Curr Hypertens Rep. 2016;18:80.
Franklin SS, O’Brien E, Staessen JA. Masked hypertension: understanding its complexity. Eur Heart J. 2017;38:1112–8.
Siven SS, Niiranen TJ, Kantola IM, Jula AM. White-coat and masked hypertension as risk factors for progression to sustained hypertension: the Finn-Home study. J Hypertens. 2016;34:54–60.
Sega R, Trocino G, Lanzarotti A, Carugo S, Cesana G, Schiavina R, et al. Alterations of cardiac structure in patients with isolated office, ambulatory, or home hypertension: data from the general population (Pressione Arteriose Monitorate E Loro Associazioni [PAMELA] Study). Circulation. 2001;104:1385–92.
Robertson D. Orthostatic hypertension: the last hemodynamic frontier. Hypertension. 2011;57:158–9.
Chhabra L, Spodick DH. Orthostatic hypertension: recognizing an underappreciated clinical condition. Indian Heart J. 2013;65:454–6.
Streeten DH, Auchincloss JH Jr., Anderson GH Jr, Richardson RL, Thomas FD, Miller JW. Orthostatic hypertension. Pathogenetic studies. Hypertension. 1985;7:196–203.
Streeten DH, Anderson GH Jr., Richardson R, Thomas FD. Abnormal orthostatic changes in blood pressure and heart rate in subjects with intact sympathetic nervous function: evidence for excessive venous pooling. J Lab Clin Med. 1988;111:326–35.
Agnoletti D, Valbusa F, Labat C, Gautier S, Mourad JJ, Benetos A.PARTAGE study Investigators. Evidence for a prognostic role of orthostatic hypertension on survival in a very old institutionalized population. Hypertension. 2016;67:191–6.
Veronese N, De Rui M, Bolzetta F, Zambon S, Corti MC, Baggio G, et al. Orthostatic changes in blood pressure and mortality in theelderly: the Pro.V.A study. Am J Hypertens. 2015;28:1248–56.
Bursztyn M, Jacobs JM, Hammerman-Rozenberg A, Stessman J. Prevalence of orthostatic hypertension in the very elderly and its relationship to all-cause mortality. J Hypertens. 2016;34:2053–8.
Weiss A, Beloosesky Y, Grossman A, Shlesinger A, Koren-Morag N, Grossman E. The association between orthostatic hypertension and all-cause mortality in hospitalized elderly persons. J Geriatr Cardiol. 2016;13:239–43.
Eguchi K, Kario K, Hoshide S, Hoshide Y, Ishikawa J, Morinari M, et al. Greater change of orthostatic blood pressure is related to silent cerebral infarct and cardiac overload in hypertensive subjects. Hypertens Res. 2004;27:235–41.
Matsubayashi K, Okumiya K, Wada T, Osaki Y, Fujisawa M, Doi Y, et al. Postural dysregulation in systolic blood pressure is associated with worsened scoring on neurobehavioral function tests and leukoaraiosis in the older elderly living in a community. Stroke. 1997;28:2169–73.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sanidas, E., Grassos, C., Papadopoulos, D.P. et al. Labile hypertension: a new disease or a variability phenomenon?. J Hum Hypertens 33, 436–443 (2019). https://doi.org/10.1038/s41371-018-0157-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-018-0157-8
This article is cited by
-
Estimating cardiovascular health gains from eradicating indoor cold in Australia
Environmental Health (2022)