Abstract
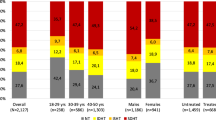
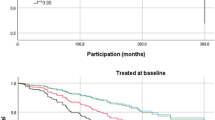
Effective and sustained blood pressure (BP) control in hypertensive patients with moderate-to-severe obesity is often difficult to achieve. We evaluated clinic, 24h, day-time and night-time systolic/diastolic BP levels and control in a large cohort of adult outpatients with different classes of obesity. A single center, prospective, cohort study was conducted at Hypertension Unit, Division of Cardiology, Sant’Andrea Hospital, Rome Italy. All BP measurements were performed and BP thresholds were set according to guidelines. Study population was stratified according to BMI. We included 4,766 individuals (women 48.6%, age 60.3 ± 11.6 years, clinic BP 143.8 ± 18.2/90.9 ± 12.3 mmHg, 24h BP 130.2 ± 13.3/79.1 ± 9.5 mmHg), among whom 36.0% had normal weight, 43.5% were overweight, 15.7% had class I, and 4.8% class II/III obesity. Obese outpatients had higher prevalence of risk factors, and were treated more frequently and with more antihypertensive drugs than those with normal body weight. Obese outpatients showed higher systolic BP levels at all BP measurements, mostly 24h and night-time periods, than those observed in normal weight outpatients. BMI resulted significantly related with clinic (r = 0.053; P < 0.001), 24h (r = 0.098; P < 0.001) and night-time systolic BP (r = 0.126; P < 0.001), and left ventricular mass indexed by height^2.7 (r = 0.311; P < 0.001). BMI was also negatively and independently associated with predefined BP goals at all types of BP measurements. Obesity was associated with higher systolic BP levels during the entire 24h period and increased left ventricular mass. These effects were independently observed, even after correction for major cardiovascular risk factors and comorbidities, as well as the number and type of antihypertensive drug classes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Bhurosy T, Jeewon R. Overweight and obesity epidemic in developing countries: a problem with diet, physical activity, or socioeconomic status? ScientificWorldJournal. 2014;2014:964236.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81.
Stevens GA, Singh GM, Lu Y, Danaei G, Lin JK, Finucane MM, et al. National, regional, and global trends in adult overweight and obesity prevalences. Popul Health Metr. 2012;10:22.
Kelly T, Yang W, Chen CS, Reynolds K, He J. Global burden of obesity in 2005 and projections to 2030. Int J Obes. 2008;32:1431–7.
Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, et al. National, regional, and global trends in body–mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377:557–67.
Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol. 2009;53:1925–32.
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88.
Hall JE. The kidney, hypertension, and obesity. Hypertension. 2003;41(3 Pt 2):625–33.
Garrison RJ, Kannel WB, Stokes J 3rd, Castelli WP. Incidence and precursors of hypertension in young adults: the Framingham Offspring Study. Prev Med. 1987;16:235–51.
Jones DW, Miller ME, Wofford MR, Anderson DC Jr., Cameron ME, et al. The effect of weight loss intervention on antihypertensive medication requirements in the hypertension Optimal Treatment (HOT) study. Am J Hypertens. 1999;12(12 Pt 1-2):1175–80.
O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, et al. European society of hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–68.
Tocci G, Presta V, Figliuzzi I, Attalla El Halabieh N, Battistoni A, Coluccia R, et al. Prevalence and clinical outcomes of white-coat and masked hypertension: analysis of a large ambulatory blood pressure database. J Clin Hypertens. 2018;20:297–305.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–219.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–357.
Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult treatment panel III). JAMA. 2001;285:2486–97.
Ryden L, Standl E, Bartnik M, Van den Berghe G, Betteridge J, de Boer MJ, et al. Guidelines on diabetes, pre-diabetes, and cardiovascular diseases: executive summary. The task force on diabetes and cardiovascular diseases of the European Society of Cardiology (ESC) and of the European Association for the Study of Diabetes (EASD). Eur Heart J. 2007;28:88–136.
Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, et al. Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the task force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology. Eur Heart J. 2008;29:2909–45.
Bassand JP, Hamm CW, Ardissino D, Boersma E, Budaj A, Fernandez-Aviles F, et al. Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J. 2007;28:1598–660.
Thygesen K, Alpert JS, White HD. Universal definition of myocardial infarction. Eur Heart J. 2007;28:2525–38.
Goldstein LB, Adams R, Alberts MJ, Appel LJ, Brass LM, Bushnell CD, et al. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council: cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group: the American Academy of Neurology affirms the value of this guideline. Stroke. 2006;37:1583–633.
Easton JD, Saver JL, Albers GW, Alberts MJ, Chaturvedi S, Feldmann E, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009;40:2276–93.
Scuteri A, Morrell CH, Orru M, AlGhatrif M, Saba PS, Terracciano A, et al. Gender specific profiles of white coat and masked hypertension impacts on arterial structure and function in the SardiNIA study. Int J Cardiol. 2016;217:92–8.
Cuspidi C, Sala C, Tadic M, Rescaldani M, Grassi G, Mancia G. Untreated masked hypertension and subclinical cardiac damage: a systematic review and meta-analysis. Am J Hypertens. 2015;28:806–13.
Baird SW, Jin Z, Okajima K, Russo C, Schwartz JE, Elkind MSV, et al. Relationship between body mass and ambulatory blood pressure: comparison with office blood pressure measurement and effect of treatment. J Hum Hypertens. 2018;32:122–8.
Kotsis V, Stabouli S, Bouldin M, Low A, Toumanidis S, Zakopoulos N. Impact of obesity on 24h ambulatory blood pressure and hypertension. Hypertension. 2005;45:602–7.
Kang IS, Pyun WB, Shin J, Kim JH, Kim SG, Shin GJ. Association between central obesity and circadian parameters of blood pressure from the korean ambulatory blood pressure monitoring registry: Kor-ABP registry. J Korean Med Sci. 2013;28:1461–7.
Macumber IR, Weiss NS, Halbach SM, Hanevold CD, Flynn JT. The association of pediatric obesity with nocturnal non-dipping on 24h ambulatory blood pressure monitoring. Am J Hypertens. 2016;29:647–52.
Palatini P, Reboldi G, Beilin LJ, Casiglia E, Eguchi K, Imai Y, et al. Prognostic value of ambulatory blood pressure in the obese: The Ambulatory Blood Pressure-International Study. J Clin Hypertens (Greenwich). 2016;18:111–8.
Mourad JJ, Lopez-Sublet M, Aoun-Bahous S, Villeneuve F, Jaboureck O, Dourmap-Collas C, et al. Impact of miscuffing during home blood pressure measurement on the prevalence of masked hypertension. Am J Hypertens. 2013;26:1205–9.
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Figliuzzi, I., Presta, V., Miceli, F. et al. 24-Hour ambulatory blood pressure levels and control in a large cohort of adult outpatients with different classes of obesity. J Hum Hypertens 33, 298–307 (2019). https://doi.org/10.1038/s41371-018-0132-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-018-0132-4
This article is cited by
-
Effective out-of-office BP monitoring to detect masked hypertension: perspectives for wearable BP monitoring
Hypertension Research (2023)
-
Prevalence and clinical characteristics of isolated systolic hypertension in young: analysis of 24 h ambulatory blood pressure monitoring database
Journal of Human Hypertension (2022)
-
The prevalence of masked hypertension and masked uncontrolled hypertension in relation to overweight and obesity in a nationwide registry in China
Hypertension Research (2022)