Abstract
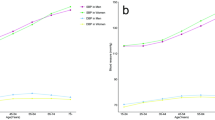
The aim of the present study was to examine the prevalence, awareness, treatment, control, and potentially influencing factors of high blood pressure (HBP) in Chinese rural adults based on a cross-sectional study. Using data from the Rural Diabetes, Obesity and Lifestyle (RuralDiab) study, a total of 30,834 participants aged 18–74 years were enrolled for the epidemiological study. The multivariate logistic regression model including all selected potentially influencing factors was carried out for the adjusted odds ratios (ORs) and 95% confidence intervals (CIs). Overall, a total of 9872 individuals were diagnosed as HBP (32.02%) with substantial imparity between men and women (32.87% vs. 30.58%), and the corresponding age-standardized prevalence of HBP were 19.50% (20.94% in men and 18.85% in women). Among the HBP patients, 6654 were aware of the diagnosis (67.40%), 5391 were taking medication (54.61%), and 2572 had their blood pressure controlled (26.05%).The corresponding age-adjusted awareness, treatment, and control of HBP were 59.35%, 45.91%, and 23.87%, respectively, and the corresponding rates were higher in women than those in men. The age-specific prevalence and management rates of HBP displayed increased trends with aging in both sexes(P trend < 0.05). Aging, low level of education, unhealthy lifestyle, positive family history of hypertension, overweight, obesity, diabetes, and dyslipidemia were associated with the prevalence, awareness, treatment, and control of HBP. In conclusion, uncontrolled HBP was common with high prevalence in Chinese rural residents. Strengthening the primary prevention through lifestyle modifications is necessary for reducing the disease burden and improving the management rates of HBP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Cooper RS, Kaufman JS, Bovet P. Global burden of disease attributable to hypertension. J Am Med Assoc. 2017;317:2017–8.
Wolf-Maier K, Cooper RS, Banegas JR, Giampaoli S, Hense HW, Joffres M, et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. J Am Med Assoc. 2003;289:2363–9.
Wu L, He Y, Jiang B, Liu M, Wang J, Yang S, et al. The association between the prevalence, treatment and control of hypertension and the risk of mild cognitive impairment in an elderly urban population in China. Hypertens Res. 2016;39:367–735.
Wu Y, Huxley R, Li L, Anna V, Xie G, Yao C, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation. 2008;118:2679–86.
Wang JW, Zhang LX, Wang F, Liu LS, Wang HY, the China National Survey of Chronic Kidney Disease Working Group. Prevalence, awareness, treatment, and control of hypertension in China: results from a National Survey. Am J Hypertens. 2014;27:1355–61.
Yang G, Wang Y, Zeng Y, Gao GF, Liang X, Zhou M, et al. Rapid health transition in China, 1990–2010: findings from the global burden of disease study 2010. Lancet. 2013;381:1987–2015.
Chen WW, Gao RL, Liu LS, Zhu ML, Wang W, Wang YJ, et al. The report of cardiovascular diseases in China–2013 profiles. Chin Circ J. 2014;29:487–91.
Gu D, Reynolds K, Wu X, Chen J, Duan X, Muntner P, et al. Prevalence, awareness, treatment, and control of hypertension in china. Hypertension. 2002;40:920–7.
Yang J, Lu F, Zhang C, Liu Z, Zhao Y, Gao F, et al. Prevalence of prehypertension and hypertension in a Chinese rural area from 1991 to 2007. Hypertens Res. 2010;33:331–7.
Writing group of 2010 Chinese guidelines for the management of hypertension. 2010 Chinese guidelines for the management of hypertension. Chin J Hypertens. 2011;19:701–43.
Chinese Nutrition Society. The dietary guidelines for Chinese residents. Lhasa: The Tibet people’s Publishing House; 2011. 97, 197–8.
World Health Organization. International guide for monitoring alcohol consumption and related harm. Geneva: WHO; 2000. p. 51.
International Physical Activity Questionnaire: Short Last 7 Days Self-Administered Format 2005. http://www.ipaq.ki.se/downloads.htm. Accessed 26 October 2015
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2009;32:S62–7.
Joint Committee for Developing Chinese Guidelines on Prevention and Treatment of Dyslipidemia in Adults. Chinese guidelines on prevention and treatment of dyslipidemia in adults. Zhonghua Xin Xue Guan Bing Za Zhi. 2007;35:390–419.
National Bureau of Statistics of the People’s Republic of China. China statistical yearbook, 2010. Beijing, China: China statistic press; 2010. http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/indexch.htm Accessed 25 April 2016
Li Z, Guo X, Zheng L, Sun Z, Yang H, Sun G, et al. Prehypertension in rural northeastern China: results from the northeast China rural cardiovascular health study. J Clin Hypertens. 2014;16:664–70.
Li D, Lv J, Liu F, Liu P, Yang X, Feng Y, et al. Hypertension burden and control in mainland China: analysis of nationwide data 2003–2012. Int J Cardiol. 2015;184:637–44.
Du S, Batis C, Wang H, Zhang B, Zhang J, Popkin BM. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. Am J Clin Nutr. 2014;99:334–43.
Wang Y, Zhang J, Ding Y, Zhang M, Liu J, Ma J, et al. Prevalence of hypertension among adults in remote rural areas of Xinjiang, China. Int J Environ Res Public Health. 2016;13. pii: E524. https://doi.org/10.3390/ijerph13060524.
Li W, Gu H, Teo KK, Bo J, Wang Y, Yang J, et al. Hypertension prevalence, awareness, treatment, and control in 115 rural and urban communities involving 47 000 people from China. J Hypertens. 2016;34:39–46.
American Heart Association Statistics Committee. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133:e38–360.
Li G, Wang H, Wang K, Wang W, Dong F, Qian Y, et al. Prevalence, awareness, treatment, control and risk factors related to hypertension among urban adults in Inner Mongolia 2014: differences between Mongolian and Han populations. BMC Public Health. 2016;16:294.
Meng XJ, Dong GH, Wang D, Liu MM, Lin Q, Tian S, et al. Prevalence, awareness, treatment, control, and risk factors associated with hypertension in urban adults from 33 communities of China: the CHPSNE study. J Hypertens. 2011;29:1303–10.
Wei Q, Sun J, Huang J, Zhou HY, Ding YM, Tao YC, et al. Prevalence of hypertension and associated risk factors in Dehui City of Jilin Province in China. J Hum Hypertens. 2015;29:64–68.
Wang H, Zhang X, Zhang J, He Q, Hu R, Wang L, et al. Factors associated with prevalence, awareness, treatment and control of hypertension among adults in Southern China: a community-based, cross-sectional survey. PLoS ONE. 2013;8:e62469 https://doi.org/10.1371/journal.pone.0062469
Qureshi AI, Suri MF, Kirmani JF, Divani AA, Mohammad Y. Is prehypertension a risk factor for cardiovascular diseases? Stroke. 2005;36:1859–63.
Suri MF, Qureshi AI. Prehypertension as a risk factor for cardiovascular diseases. J Cardiovasc Nurs. 2006;21:478–82.
Gu D, He J, Coxson PG, Rasmussen PW, Huang C, Thanataveerat A, et al. The cost-effectiveness of low-cost essential antihypertensive medicines for hypertension control in China: a modelling study. PLoS Med. 2015;12:e1001860.
Dong G, Sun Z, Zheng L, Li J, Zhang X, Zhang X, et al. Prevalence, awareness, treatment, and control of hypertension in rural adults from Liaoning Province, Northeast China. Hypertens Res. 2007;30:951–8.
Meng XJ, Dong GH, Wang D, Liu MM, Lin Q, Tian S, et al. Prevalence, awareness, treatment, control, and risk factors associated with hypertension in urban adults from 33 communities of China: the CHPSNEstudy. J Hypertens. 2011;29:1303–10.
Black ML, Wise CA, Wang W, Bittles AH. Combining genetics and population history in the study of ethnic diversity in the People’s Republic of China. Hum Biol. 2006;78:277–93.
Wang Y, Klarić L, Yu X, Thaqi K, Dong J, Novokmet M, et al. The association between glycosylation of immunoglobulin g and hypertension: a multiple ethnic cross-sectional study. Medicine. 2016;95:e3379.
Acknowledgements
This research was supported by the National Key Research and Development Program “Precision Medicine Initiative” of China (Grant No. 2016YFC0900803), National Natural Science Foundation of China (Grant No. 81573243, 81602925, U1304821), Henan Provincial Science Fund for Distinguished Young Scholars (Grant No. 164100510021), Science and Technology Innovation Talents Support Plan of Henan Province Colleges and Universities (Grant No. 14HASTIT035), High-level Personnel Special Support Project of Zhengzhou University (Grant No. ZDGD13001). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. In addition, we like to thank the participants, the coordinators, and administrators for their supports during the study. To Dr. Fatiha Karam, the authors would like to express their gratitude for their critical reading of the manuscript.
Author contributions
CW conceived and designed the experiments. XL, YL, YG, LL, KY, RL, ZM, and RB performed and conducted the experiments. XL, YL, KY, and RL analyzed the data and take responsibility for the integrity and accuracy of the information. XL, ZM, and RB contributed to the reagents/materials/analysis tools. XL and YL drafted and revised the manuscript. All authors have approved the final manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
These authors contributed equally: Xiaotian Liu and Yuqian Li.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Liu, X., Li, Y., Guo, Y. et al. The burden, management rates and influencing factors of high blood pressure in a Chinese rural population: the Rural Diabetes, Obesity and Lifestyle (RuralDiab) study. J Hum Hypertens 32, 236–246 (2018). https://doi.org/10.1038/s41371-018-0039-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-018-0039-0
This article is cited by
-
Alterations of gut microbiota are associated with blood pressure: a cross-sectional clinical trial in Northwestern China
Journal of Translational Medicine (2023)
-
Diabetic peripheral neuropathy screening and the related risk factors to its prevalence in people with type 2 diabetes
International Journal of Diabetes in Developing Countries (2023)
-
Prevalence of miR146a Gene Polymorphisms in Diabetic and Non-diabetic Patients with Chronic Kidney Disease
Iranian Journal of Science and Technology, Transactions A: Science (2022)
-
Associations between PM2.5 exposure duration and physical activity intensity on the health of hypertension in urban residents of Beijing
Environmental Science and Pollution Research (2021)
-
Prevalence and risk factors of chronic kidney disease and diabetic kidney disease in a central Chinese urban population: a cross-sectional survey
BMC Nephrology (2020)