Abstract
Background/objectives
Gestational exposure to perfluoroalkyl substances (PFAS), a ubiquitous class of persistent endocrine disrupting chemicals, is associated with increased risk of obesity and cardiometabolic disease. However, it is unclear if gestational PFAS exposure is associated with adiposity trajectories related to adult obesity and cardiometabolic health.
Subjects/methods
We measured perfluorooctanoic acid (PFOA), perfluorooctanesulfonic acid (PFOS), perfluorononaoic acid, and perfluorohexanesulfonic acid (PFHxS) concentrations in maternal serum collected between 16 weeks gestation and delivery in a cohort of 345 mother–child pairs in Cincinnati, OH (enrolled 2003-06). From age 4 weeks to 12 years, we measured weight and length or height up to eight times and calculated child body mass index (BMI) (1865 repeated measures). Using covariate-adjusted linear mixed models and splines to account for repeated BMI measures and nonlinear BMI patterns, respectively, we estimated the age/magnitude of infancy BMI zenith (~1 year) and childhood BMI nadir (~5 years), BMI accrual from 8 to 12 years, and BMI at age 12 years by PFAS terciles.
Results
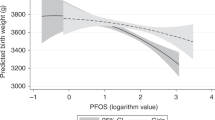
BMI trajectories varied by PFOA concentrations (age × PFOA interaction p value = 0.03). Children born to women with higher PFOA concentrations had lower infancy and early childhood BMI, earlier BMI nadir, accelerating BMI gains in mid-childhood and adolescence, and higher BMI at age 12 years. Some of these associations were non-monotonic. PFOS and PFHxS were not associated with alterations in BMI trajectories, but were monotonically associated with lower BMI across infancy, childhood, and adolescence. Compared to children in the first PFOS tercile, those in the second (β: −0.83; 95% confidence interval (CI): −2.11, 0.51 kg/m2), and third (β: −1.41; 95% CI: −2.65, −0.14 kg/m2) had lower BMI at age 12 years.
Conclusions
These results suggest that gestational PFOA exposure may be associated with BMI trajectories related to adult obesity and cardiometabolic disease, while PFOS and PFHxS exposure is associated with lower BMI in the first 12 years of life.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2. JAMA. 2014;311:806–14.
Sahoo K, Sahoo B, Choudhury AK, Sofi NY, Kumar R, Bhadoria AS. Childhood obesity: causes and consequences. J Family Med Prim Care. 2015;4:187–92.
Park MH, Falconer C, Viner RM, Kinra S. The impact of childhood obesity on morbidity and mortality in adulthood: a systematic review. Obes Rev. 2012;13:985–1000.
Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet. 2002;360:473–82.
Llewellyn A, Simmonds M, Owen CG, Woolacott N. Childhood obesity as a predictor of morbidity in adulthood: a systematic review and meta-analysis. Obes Rev. 2015;17:56–67.
Di Gravio C, Krishnaveni GV, Somashekara R, Veena SR, Kumaran K, Krishna M, et al. Comparing BMI with skinfolds to estimate age at adiposity rebound and its associations with cardio-metabolic risk markers in adolescence. Int J Obes. 2019;43:683–90.
Brisbois TD, Farmer AP, McCargar LJ. Early markers of adult obesity: a review. Obes Rev. 2012;13:347–67.
Aris IM, Rifas-Shiman SL, Li LJ, Kleinman KP, Coull BA, Gold DR, et al. Patterns of body mass index milestones in early life and cardiometabolic risk in early adolescence. Int J Epidemiol. 2019;48:157–67.
Zhang T, Whelton PK, Xi B, Krousel-Wood M, Bazzano L, He J, et al. Rate of change in body mass index at different ages during childhood and adult obesity risk. Pediatr Obes. 2019;14:e12513.
Geserick M, Vogel M, Gausche R, Lipek T, Spielau U, Keller E, et al. Acceleration of BMI in early childhood and risk of sustained obesity. N Engl J Med. 2018;379:1303–12.
Bjerregaard LG, Adelborg K, Baker JL. Change in body mass index from childhood onwards and risk of adult cardiovascular disease. Trends Cardiovasc Med. 2020;30:39–45.
Gjaerde LK, Gamborg M, Angquist L, Truelsen TC, Sorensen TIA, Baker JL. Association of childhood body mass index and change in body mass index with first adult ischemic stroke. JAMA Neurol. 2017;74:1312–8.
Bjerregaard LG, Jensen BW, Angquist L, Osler M, Sorensen TIA, Baker JL. Change in overweight from childhood to early adulthood and risk of type 2 diabetes. N Engl J Med. 2018;378:1302–12.
Sovio U, Kaakinen M, Tzoulaki I, Das S, Ruokonen A, Pouta A, et al. How do changes in body mass index in infancy and childhood associate with cardiometabolic profile in adulthood? Findings from the Northern Finland Birth Cohort 1966 Study. Int J Obes. 2014;38:53–9.
Aris IM, Bernard JY, Chen LW, Tint MT, Pang WW, Lim WY, et al. Infant body mass index peak and early childhood cardio-metabolic risk markers in a multi-ethnic Asian birth cohort. Int J Epidemiol. 2017;46:513–25.
Peneau S, Gonzalez-Carrascosa R, Gusto G, Goxe D, Lantieri O, Fezeu L, et al. Age at adiposity rebound: determinants and association with nutritional status and the metabolic syndrome at adulthood. Int J Obes. 2016;40:1150–6.
Aris IM, Rifas-Shiman SL, Li LJ, Kleinman K, Coull BA, Gold DR, et al. Pre-, perinatal, and parental predictors of body mass index trajectory milestones. J Pediatr. 2018;201:69–77.e8.
Heindel JJ, Blumberg B. Environmental obesogens: mechanisms and controversies. Annu Rev Pharmacol Toxicol. 2019;59:59–106.
Office of Economic Co-operation and Development (OECD). Toward a new comprehensive global datbase of per- and polyfluoroalkyl substances (PFAS). Paris: Organisation for Economic Co-operation and Development; 2018. https://www.oecd.org/officialdocuments/publicdisplaydocumentpdf/?cote=ENV-JM-MONO(2018)7&doclanguage=en.
Calafat AM, Wong LY, Kuklenyik Z, Reidy JA, Needham LL. Polyfluoroalkyl chemicals in the U.S. population: data from the National Health and Nutrition Examination Survey (NHANES) 2003-2004 and comparisons with NHANES 1999-2000. Environ Health Perspect. 2007;115:1596–602.
Woodruff TJ, Zota AR, Schwartz JM. Environmental chemicals in pregnant women in the United States: NHANES 2003-2004. Environ Health Perspect. 2011;119:878–85.
Olsen GW, Burris JM, Ehresman DJ, Froehlich JW, Seacat AM, Butenhoff JL, et al. Half-life of serum elimination of perfluorooctanesulfonate,perfluorohexanesulfonate, and perfluorooctanoate in retired fluorochemical production workers. Environ Health Perspect. 2007;115:1298–305.
Kashino I, Sasaki S, Okada E, Matsuura H, Goudarzi H, Miyashita C, et al. Prenatal exposure to 11 perfluoroalkyl substances and fetal growth: a large-scale, prospective birth cohort study. Environ Int. 2020;136:105355.
Forns J, Verner MA, Iszatt N, Nowack N, Bach CC, Vrijheid M, et al. Early life exposure to perfluoroalkyl substances (PFAS) and ADHD: a meta-analysis of nine European population-based studies. Environ Health Perspect. 2020;128:57002.
Haines DA, Khoury C, Saravanabhavan G, Werry K, Walker M, Malowany M. Human biomonitoring reference values derived for persistent organic pollutants in blood plasma from the Canadian Health Measures Survey 2007–2011. Int J Hyg Environ Health. 2017;220:744–56.
Heindel JJ, Blumberg B, Cave M, Machtinger R, Mantovani A, Mendez MA, et al. Metabolism disrupting chemicals and metabolic disorders. Reprod Toxicol. 2017;68:3–33.
Ye L, Guo J, Ge RS. Environmental pollutants and hydroxysteroid dehydrogenases. Vitam Horm. 2014;94:349–90.
Fletcher T, Galloway TS, Melzer D, Holcroft P, Cipelli R, Pilling LC, et al. Associations between PFOA, PFOS and changes in the expression of genes involved in cholesterol metabolism in humans. Environ Int. 2013;57-58:2–10.
Vanden Heuvel JP, Thompson JT, Frame SR, Gillies PJ. Differential activation of nuclear receptors by perfluorinated fatty acid analogs and natural fatty acids: a comparison of human, mouse, and rat peroxisome proliferator-activated receptor-alpha, -beta, and -gamma, liver X receptor-beta, and retinoid X receptor-alpha. Toxicol Sci. 2006;92:476–89.
Qi W, Clark JM, Timme-Laragy AR, Park Y. Perfluorobutanesulfonic acid (PFBS) potentiates adipogenesis of 3T3-L1 adipocytes. Food Chem Toxicol. 2018;120:340–5.
Watkins AM, Wood CR, Lin MT, Abbott BD. The effects of perfluorinated chemicals on adipocyte differentiation in vitro. Mol Cell Endocrinol. 2015;400:90–101.
Johnson PI, Sutton P, Atchley DS, Koustas E, Lam J, Sen S, et al. The Navigation Guide—evidence-based medicine meets environmental health: systematic review of human evidence for PFOA effects on fetal growth. Environ Health Perspect. 2014;122:1028–39.
Shoaff J, Papandonatos GD, Calafat AM, Chen A, Lanphear BP, Ehrlich S, et al. Prenatal exposure to perfluoroalkyl substances: infant birth weight and early life growth. Environ Epidemiol. 2018;2:1–7.
Maisonet M, Terrell ML, McGeehin MA, Christensen KY, Holmes A, Calafat AM, et al. Maternal concentrations of polyfluoroalkyl compounds during pregnancy and fetal and postnatal growth in British girls. Environ Health Perspect. 2012;120:1432–7.
Braun JM, Chen A, Romano ME, Calafat AM, Webster GM, Yolton K, et al. Prenatal perfluoroalkyl substance exposure and child adiposity at 8 years of age: the HOME Study. Obesity. 2016;24:231–7.
Halldorsson TI, Rytter D, Haug LS, Bech BH, Danielsen I, Becher G, et al. Prenatal exposure to perfluorooctanoate and risk of overweight at 20 years of age: a prospective cohort study. Environ Health Perspect. 2012;120:668–73.
Hoyer BB, Ramlau-Hansen CH, Vrijheid M, Valvi D, Pedersen HS, Zviezdai V, et al. Anthropometry in 5- to 9-year-old Greenlandic and Ukrainian children in relation to prenatal exposure to perfluorinated alkyl substances. Environ Health Perspect. 2015;123:841–6.
Mora AM, Oken E, Rifas-Shiman SL, Webster TF, Gillman MW, Calafat AM, et al. Prenatal exposure to perfluoroalkyl substances and adiposity in early and mid-childhood. Environmental Health Perspectives. 2017;125:467–73.
Chen MH, Ng S, Hsieh CJ, Lin CC, Hsieh WS, Chen PC. The impact of prenatal perfluoroalkyl substances exposure on neonatal and child growth. Sci Total Environ. 2017;607-608:669–75.
Starling AP, Adgate JL, Hamman RF, Kechris K, Calafat AM, Dabelea D. Prenatal exposure to per- and polyfluoroalkyl substances and infant growth and adiposity: the Healthy Start Study. Environ Intl. 2019;131:104983.
Braun JM, Buckley JP, Cecil KM, Chen A, Kalkwarf HJ, Lanphear BP, et al. Adolescent follow-up in the Health Outcomes and Measures of the Environment (HOME) Study: cohort profile. BMJ Open. 2020;10:e034838.
Braun JM, Kalloo G, Chen A, Dietrich KN, Liddy-Hicks S, Morgan S, et al. Cohort profile: the Health Outcomes and Measures of the Environment (HOME) Study. Int J Epidemiol. 2017;46:24.
Kato K, Basden BJ, Needham LL, Calafat AM. Improved selectivity for the analysis of maternal serum and cord serum for polyfluoroalkyl chemicals. J Chromatogr A. 2011;1218:2133–7.
van der Laan MJ, Polley EC, Hubbard AE. Super learner. Stat Appl Genet Mol Biol. 2007;6:Article25.
Braun JM, Daniels JL, Poole C, Olshan AF, Hornung R, Bernert JT, et al. A prospective cohort study of biomarkers of prenatal tobacco smoke exposure: the correlation between serum and meconium and their association with infant birth weight. Environ Health. 2010;9:53.
Romano ME, Xu Y, Calafat AM, Yolton K, Chen A, Webster GM, et al. Maternal serum perfluoroalkyl substances during pregnancy and duration of breastfeeding. Environ Res. 2016;149:239–46.
Grajeda LM, Ivanescu A, Saito M, Crainiceanu C, Jaganath D, Gilman RH, et al. Modelling subject-specific childhood growth using linear mixed-effect models with cubic regression splines. Emerg Themes Epidemiol. 2016;13:1.
Werner EF, Braun JM, Yolton K, Khoury JC, Lanphear BP. The association between maternal urinary phthalate concentrations and blood pressure in pregnancy: the HOME Study. Environ Health. 2015;14:75.
Rosner B. Fundamentals of biostatistics. 4th ed. Pacific Grove, CA: Duxbury; 2000.
Tanner EM, Bornehag CG, Gennings C. Dynamic growth metrics for examining prenatal exposure impacts on child growth trajectories: application to perfluorooctanoic acid (PFOA) and postnatal weight gain. Environ Res. 2019;182:109044.
Gyllenhammar I, Diderholm B, Gustafsson J, Berger U, Ridefelt P, Benskin JP, et al. Perfluoroalkyl acid levels in first-time mothers in relation to offspring weight gain and growth. Environ Int. 2017;111:191–9.
Taxvig C, Dreisig K, Boberg J, Nellemann C, Schelde AB, Pedersen D, et al. Differential effects of environmental chemicals and food contaminants on adipogenesis, biomarker release and PPARgamma activation. Mol Cell Endocrinol. 2012;361:106–15.
Bastos Sales L, Kamstra JH, Cenijn PH, van Rijt LS, Hamers T, Legler J. Effects of endocrine disrupting chemicals on in vitro global DNA methylation and adipocyte differentiation. Toxicol in Vitro. 2013;27:1634–43.
Hines EP, White SS, Stanko JP, Gibbs-Flournoy EA, Lau C, Fenton SE. Phenotypic dichotomy following developmental exposure to perfluorooctanoic acid (PFOA) in female CD-1 mice: low doses induce elevated serum leptin and insulin, and overweight in mid-life. Mol Cell Endocrinol. 2009;304:97–105.
Lv Z, Li G, Li Y, Ying C, Chen J, Chen T, et al. Glucose and lipid homeostasis in adult rat is impaired by early-life exposure to perfluorooctane sulfonate. Environ Toxicol. 2013;28:532–42.
Kingsley SL, Kelsey KT, Butler R, Chen A, Eliot MN, Romano ME, et al. Maternal serum PFOA concentration and DNA methylation in cord blood: A pilot study. Environ Res. 2017;158:174–8.
Ornoy A. Prenatal origin of obesity and their complications: gestational diabetes, maternal overweight and the paradoxical effects of fetal growth restriction and macrosomia. Reprod Toxicol. 2011;32:205–12.
Barker DJP. Developmental origins of chronic disease. Public Health. 2012;126:185–9.
Andersen CS, Fei C, Gamborg M, Nohr EA, Sorensen TI, Olsen J. Prenatal exposures to perfluorinated chemicals and anthropometry at 7 years of age. Am J Epidemiol. 2013;178:921–7.
Barry V, Darrow LA, Klein M, Winquist A, Steenland K. Early life perfluorooctanoic acid (PFOA) exposure and overweight and obesity risk in adulthood in a community with elevated exposure. Environ Res. 2014;132C:62–9.
Martinsson M, Nielsen C, Bjork J, Rylander L, Malmqvist E, Lindh C, et al. Intrauterine exposure to perfluorinated compounds and overweight at age 4: a case-control study. PloS ONE. 2020;15:e0230137.
Manzano-Salgado CB, Casas M, Lopez-Espinosa MJ, Ballester F, Iniguez C, Martinez D, et al. Prenatal exposure to perfluoroalkyl substances and cardiometabolic risk in children from the spanish INMA birth cohort study. Environ Health Perspect. 2017;125:097018.
Koustas E, Lam J, Sutton P, Johnson PI, Atchley DS, Sen S, et al. The navigation guide-evidence-based medicine meets environmental health: systematic review of nonhuman evidence for PFOA effects on fetal growth. Environ Health Perspect. 2014;122:1015–27.
Abbott BD. Review of the expression of peroxisome proliferator-activated receptors alpha (PPAR alpha), beta (PPAR beta), and gamma (PPAR gamma) in rodent and human development. Reprod Toxicol. 2009;27:246–57.
Abbott BD, Wolf CJ, Das KP, Zehr RD, Schmid JE, Lindstrom AB, et al. Developmental toxicity of perfluorooctane sulfonate (PFOS) is not dependent on expression of peroxisome proliferator activated receptor-alpha (PPAR alpha) in the mouse. Reprod Toxicol. 2009;27:258–65.
Kingsley SL, Eliot MN, Kelsey KT, Calafat AM, Ehrlich S, Lanphear BP, et al. Variability and predictors of serum perfluoroalkyl substance concentrations during pregnancy and early childhood. Environ Res. 2018;165:247–57.
Verner MA, Loccisano AE, Morken NH, Yoon M, Wu H, McDougall R, et al. Associations of perfluoroalkyl substances (PFASs) with lower birth weight: an evaluation of potential confounding by glomerular filtration rate using a physiologically based pharmacokinetic model (PBPK). Environ Health Perspect. 2015;123:1317–24.
Lazarevic N, Barnett AG, Sly PD, Knibbs LD. Statistical methodology in studies of prenatal exposure to mixtures of endocrine-disrupting chemicals: a review of existing approaches and new alternatives. Environ Health Perspect. 2019;127:26001.
Acknowledgements
This work was supported by National Institute of Environmental Health Sciences grants P01 ES011261, R01 ES014575, R01 ES020349, R01 ES027244, R01 ES025214, and R01 ES030078. We would like to acknowledge the Centers for Disease Control and Prevention (CDC) laboratory staff who performed the PFAS measurements. We are grateful to our participants for the time they have given to our study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Brown University was compensated for JMB’s services as an expert witness for plaintiffs in litigation related to PFAS-contaminated drinking water; these funds were not paid to JMB directly. JMB received a honorarium for serving on an advisory board to Quest Diagnostics. CBE was compensated as an expert witness for plaintiffs in litigation related to PFAS-contaminated drinking water. BPL served as an expert witness in cases related to childhood lead poisoning, but he has not personally received any compensation for these services. The other authors report no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Braun, J.M., Eliot, M., Papandonatos, G.D. et al. Gestational perfluoroalkyl substance exposure and body mass index trajectories over the first 12 years of life. Int J Obes 45, 25–35 (2021). https://doi.org/10.1038/s41366-020-00717-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-020-00717-x
This article is cited by
-
Prenatal exposure to per- and polyfluoroalkyl substances and early childhood adiposity and cardiometabolic health in the Healthy Start study
International Journal of Obesity (2024)
-
Per- and polyfluoroalkyl substances, gestational weight gain, postpartum weight retention and body composition in the UPSIDE cohort
Environmental Health (2023)
-
Prenatal and childhood exposure to per-/polyfluoroalkyl substances (PFASs) and its associations with childhood overweight and/or obesity: a systematic review with meta-analyses
Environmental Health (2023)
-
Determinants of maternal and neonatal PFAS concentrations: a review
Environmental Health (2023)
-
Serum perfluoroalkyl substances and growth and development in US adolescents: a nationally representative cross-sectional study
European Journal of Pediatrics (2023)