Abstract
Objective
Emerging evidence suggests that individual appetitive traits may usefully explain patterns of weight loss in behavioral weight loss treatments for children. The objective of this study was to identify trajectories of child appetitive traits and the impact on child weight changes over time.
Methods
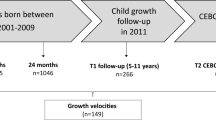
Secondary data analyses of a randomized noninferiority trial conducted between 2011 and 2015 evaluated children’s appetitive traits and weight loss. Children with overweight and obesity (mean age = 10.4; mean BMI z = 2.0; 67% girls; 32% Hispanic) and their parent (mean age = 42.9; mean BMI = 31.9; 87% women; 31% Hispanic) participated in weight loss programs and completed assessments at baseline, 3, 6,12, and 24 months. Repeated assessments of child appetitive traits, including satiety responsiveness, food responsiveness and emotional eating, were used to identify parsimonious grouping of change trajectories. Linear mixed-effects models were used to identify the impact of group trajectory on child BMIz change over time.
Results
One hundred fifty children and their parent enrolled in the study. The three-group trajectory model was the most parsimonious and included a high satiety responsive group (HighSR; 47.4%), a high food responsive group (HighFR; 34.6%), and a high emotional eating group (HighEE; 18.0%). Children in all trajectories lost weight at approximately the same rate during treatment, however, only the HighSR group maintained their weight loss during follow-ups, while the HighFR and HighEE groups regained weight (adjusted p-value < 0.05).
Conclusions
Distinct trajectories of child appetitive traits were associated with differential weight loss maintenance. Identified high-risk subgroups may suggest opportunities for targeted intervention and maintenance programs.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, et al. Trends in obesity prevalence among children and adolescents in the united states, 1988–1994 through 2013–2014. JAMA. 2016;315:2292–9.
Singh AS, Mulder C, Twisk JWR, Van Mechelen W, Chinapaw MJM. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9:474–88.
Force USPST. Screening for obesity in children and adolescents: US preventive services task force recommendation statement. JAMA. 2017;317:2417–26.
Block JP, Oken E. Practical considerations for the us preventive services task force recommendations on obesity in children and adolescents. JAMA Int Med. 2017;177:1077–9.
Carnell S, Wardle J. Appetite and adiposity in children: evidence for a behavioral susceptibility theory of obesity. Am J Clin Nutr. 2008;88:22–29.
Ferriday D, Brunstrom JM. ‘I just can’t help myself’: effects of food-cue exposure in overweight and lean individuals. Int J Obesity. 2010;35:142.
Carnell S, Wardle J. Appetitive traits and child obesity: measurement, origins and implications for intervention: Symposium on ‘Behavioural nutrition and energy balance in the young’. Proc Nutr Soc. 2008;67:343–55.
Boutelle KN, Bouton ME. Implications of learning theory for developing programs to decrease overeating. Appetite. 2015;93:62–74.
Jansen A, Vanreyten A, van Balveren T, Roefs A, Nederkoorn C, Havermans R. Negative affect and cue-induced overeating in non-eating disordered obesity. Appetite. 2008;51:556–62.
Field AE, Camargo CA Jr, Ogino S. The merits of subtyping obesity: one size does not fit all. JAMA. 2013;310:2147–8.
Webber L, Hill C, Saxton J, Van Jaarsveld CHM, Wardle J. Eating behaviour and weight in children. Int J Obesity. 2008;33:21.
Jansen A, Theunissen N, Slechten K, Nederkoorn C, Boon B, Mulkens S, et al. Overweight children overeat after exposure to food cues. Eating Behav. 2003;4:197–209.
Boutelle KN, Peterson CB, Crosby RD, Rydell SA, Zucker N, Harnack L. Overeating phenotypes in overweight and obese children. Appetite. 2014;76:95–100.
French SA, Epstein LH, Jeffery RW, Blundell JE, Wardle J. Eating behavior dimensions. Associations with energy intake and body weight. A review. Appetite. 2012;59:541–9.
Fisher JO, Cai G, Jaramillo SJ, Cole SA, Comuzzie AG, Butte NF. Heritability of hyperphagic eating behavior and appetite-related hormones among hispanic children. Obesity. 2007;15:1484–95.
Birch LL, Fisher JO, Davison KK. Learning to overeat: maternal use of restrictive feeding practices promotes girls’ eating in the absence of hunger. Am J Clin Nutr. 2003;78:215–20.
Shomaker LB, Tanofsky-Kraff M, Zocca JM, Courville A, Kozlosky M, Columbo KM, et al. Eating in the absence of hunger in adolescents: intake after a large-array meal compared with that after a standardized meal. Am J Clin Nutr. 2010;92:697–703.
Boutelle KN, Rhee KE, Liang J, et al. Effect of attendance of the child on body weight, energy intake, and physical activity in childhood obesity treatment: a randomized clinical trial. JAMA Pediatrics. 2017;171:622–8.
Boutelle KN, Braden A, Douglas JM, Rhee KE, Strong D, Rock CL, et al. Design of the FRESH study: a randomized controlled trial of a parent-only and parents of school child family-based treatment for childhood obesity. Contemp Clin Trials. 2015;45:364–70.
Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, et al. CDC growth charts: United States. Advance data from vital and health statistics; no. 314. Hyattsville, Maryland: National Center for Health Statistics. 2000.
Carnell S, Wardle J. Measuring behavioural susceptibility to obesity: validation of the child eating behaviour questionnaire. Appetite. 2007;48:104–13.
Wardle J, Guthrie CA, Sanderson S, Rapoport L. Development of the children’s eating behaviour questionnaire. J Child Psychol Psychiatry. 2001;42:963–70.
Tanofsky-Kraff M, Theim KR, Yanovski SZ, Bassett AM, Burns NP, Ranzenhofer LM, et al. Validation of the emotional eating scale adapted for use in children and adolescents (EES-C). Int J Eating Disord. 2007;40:232–40.
Vannucci A, Tanofsky-Kraff M, Shomaker LB, Ranzenhofer LM, Matheson BE, Cassidy OL, et al. Construct validity of the emotional eating scale adapted for children and adolescents. Int J Obesity. 2011;36:938.
Tanofsky-Kraff M, Ranzenhofer LM, Yanovski SZ, Schvey NA, Faith M, Gustafson J, et al. Psychometric properties of a new questionnaire to assess eating in the absence of hunger in children and adolescents. Appetite. 2008;51:148–55.
Nagin DS. Group-based trajectory modeling: an overview. Annals Nutr Metab. 2014;65:205–10.
Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annual Rev Clin Psychol. 2010;6:109–38.
Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociol Methods Res. 2007;35:542–71.
Klijn SL, Weijenberg MP, Lemmens P, van den Brandt PA, Lima Passos V. Introducing the fit-criteria assessment plot–A visualisation tool to assist class enumeration in group-based trajectory modelling. Stat Methods Med Res. 2017;26:2424–36.
Little RJ. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc. 1988;83:1198–202.
Jones BL, Nagin DS, Roeder KA. SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res. 2001;29:374–93.
Benjamini Y, Krieger AM, Yekutieli D. Adaptive linear step-up procedures that control the false discovery rate. Biometrika. 2006;93:491–507.
R Development CORE Team. R: A language and environment for statistical computing. R foundation for statistical computing. Vienna, Austria: R Development CORE Team; 2008.
Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67:1–48.
Lenth RV. Least-squares means: the R package lsmeans. J Stat Softw. 2016;69:1–33.
Schachter S. Some extraordinary facts about obese humans and rats. Am Psychol. 1971;26:129.
Schachter S, Rodin J. Obese humans and rats. John Wiley & Sons Inc. New York, NY, 1974.
Appelhans BM, Woolf K, Pagoto SL, Schneider KL, Whited MC, Liebman R. Inhibiting food reward: delay discounting, food reward sensitivity, and palatable food intake in overweight and obese women. Obesity. 2011;19:2175–82.
Berridge KC, Ho C-Y, Richard JM, DiFeliceantonio AG. The tempted brain eats: pleasure and desire circuits in obesity and eating disorders. Brain Res. 2010;1350:43–64.
Volkow ND, Wang G-J, Baler RD. Reward, dopamine and the control of food intake: implications for obesity. Trends Cogn Sci. 2011;15:37–46.
Boutelle K, Wierenga CE, Bischoff-Grethe A, Melrose AJ, Grenesko-Stevens E, Paulus MP, et al. Increased brain response to appetitive tastes in the insula and amygdala in obese compared with healthy weight children when sated. Int J Obesity. 2015;39:620.
Bruce A, Holsen L, Chambers R, Martin L, Brooks W, Zarcone J, et al. Obese children show hyperactivation to food pictures in brain networks linked to motivation, reward and cognitive control. Int J Obesity. 2010;34:1494.
Klasnja P, Hekler EB, Shiffman S, Boruvka A, Almirall D, Tewari A, et al. Microrandomized trials: an experimental design for developing just-in-time adaptive interventions. Health Psychol. 2015;34:1220.
Nahum-Shani I, Smith SN, Spring BJ, Collins LM, Witkiewitz K, Tewari A, et al. Just-in-time adaptive interventions (JITAIs) in mobile health: key components and design principles for ongoing health behavior support. Annals Behav Med. 2017;52:446–62.
Acknowledgements
We want to thank and acknowledge all of the families and children who participated in this study. The families that participated were reimbursed for time and effort, and the interventionists who worked at the University of California, San Diego Center for Healthy Eating and Activity Research were compensated for their work. In 2017, our group had the following published in JAMA Pediatrics [18].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Boutelle, K.N., Kang Sim, D.E., Manzano, M. et al. Role of appetitive phenotype trajectory groups on child body weight during a family-based treatment for children with overweight or obesity. Int J Obes 43, 2302–2308 (2019). https://doi.org/10.1038/s41366-019-0463-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0463-4
This article is cited by
-
Characteristics of eating behavior profiles among preschoolers with low-income backgrounds: a person-centered analysis
International Journal of Behavioral Nutrition and Physical Activity (2022)