Abstract
Objective
To investigate the performance of weight/heightn in discriminating obesity-related cardio-metabolic risks, and compare their performance with BMI in Chinese and American children.
Methods
57,201 Chinese children aged 7–18 and 10,441 American children aged 12–18 with complete record of sex, age, height, weight, and waist circumference were included. Analyses and comparisons of BMI, weight/height2.5, and weight/height3 were predominantly discussed, while BMI z score, converted by BMI based on 2007 WHO growth standard, was set as the reference. Log-binomial regression models and areas under receiver-operating characteristic curves were used to examine their abilities on identifying cardio-metabolic risks, including elevated blood pressure, impaired fasting glucose, and dyslipidemia. Misclassification rates of each index were calculated.
Results
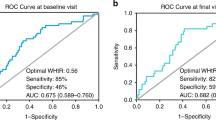
Weight/height3 is relatively stable during childhood in both populations. Odds ratio of weight/height3 in discriminating cardio-metabolic risks ranged from 1.09 (95% CI: 1.04, 1.14) to 1.23 (95% CI: 1.22, 1.25) and 1.06 (95% CI: 1.04, 1.08,) to 1.17 (95% CI: 1.15, 1.20) in Chinese and American participants, respectively. When 85th and 95th percentiles were set as thresholds for each sex, weight/height3 showed similar accuracy to BMI percentiles, and were more precise than BMI z scores. Misclassification rates of weight/height3 ranged from 19.1% (95% CI: 18.8%, 19.5%) to 34.7% (95% CI: 34.0%, 35.4%) compared to BMI z score, which ranged from 26.3% (95% CI: 26.0%, 26.7%) to 36.8% (95% CI: 36.0%, 37.5%) in Chinese participants. Results were similar in American participants. Combined use of weight/height3 and waist-to-height ratio did not change the classification accuracy.
Conclusions and relevance
Tri-ponderal mass index (TMI) performed superior to BMI z scores and similar to BMI percentiles in Chinese and American participants. TMI is stable in adolescents, and could be a more efficient indicator for screening obesity-related cardio-metabolic risks in routine health screening compared with BMI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Force USPST, Barton M. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics. 2010;125:361–7.
Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–14.
Peterson CM, Su H, Thomas DM, Heo M, Golnabi AH, Pietrobelli A, et al. Tri-ponderal mass index vs body mass index in estimating body fat during adolescence. JAMA Pediatr. 2017;171:629–36.
Heo M, Kabat GC, Gallagher D, Heymsfield SB, Rohan TE. Optimal scaling of weight and waist circumference to height for maximal association with DXA-measured total body fat mass by sex, age and race/ethnicity. Int J Obes. 2013;37:1154–60.
TJ. C. Weight/heightp compared to weight/height2 for assessing adiposity in childhood: influence of age and bone age on p during puberty. Ann Hum Biol. 1986;13:19.
Rosenthal M, Bain SH, Bush A, Warner JO. Weight/height2.88 as a screening test for obesity or thinnes in schoolage children. Eur J Pediatr. 1994;153:876–83.
Faron O. Adolphe Quetelet, Physique sociale ou essai sur le développement des facultés de l’homme [1869]. 1997. Ann Demogr Hist. 1998;1:266.
Quetelet A. Essai sur le développement des facultés de l’homme. In: Vilquin E, Anderson JP. Brussels: Académie Royale de Belgique. 1869.
Cole TJ. Weight-stature indices to measure underweight, overweight, and obesity. Anthr Assess Nutrition Status. 1991:83–111.
De Lorenzo A, Romano L, Di Renzo L, Gualtieri P, Salimei C, Carrano E, et al. Triponderal mass index rather than body mass index: an indicator of high adiposity in Italian children and adolescents. Nutrition. 2019;60:41–7.
Hattori K, Hirohara T. Age change of power in weight/heightp indices used as indicators of adiposity in japanese. Am J Hum Biol. 2002;14:275–9.
John Lukens VDD, Kanneganti TD. Inflammasome activation in obesity-related inflammatory diseases and autoimmunity. Discov Med.2011;12:10
Silveira LS, Monteiro PA, Antunes Bde M, Seraphim PM, Fernandes RA, Christofaro DG, et al. Intra-abdominal fat is related to metabolic syndrome and non-alcoholic fat liver disease in obese youth. BMC Pediatr. 2013;13:6.
Larsson SC, Wolk A. Overweight and obesity and incidence of leukemia: a meta-analysis of cohort studies. Int J Cancer. 2008;122:1418–21.
Singer K, Eng DS, Lumeng CN, Gebremariam A, M. Lee J. The relationship between body fat mass percentiles and inflammation in children. Obesity. 2014;22:1332–6.
Linder K, Springer F, Machann J, Schick F, Fritsche A, Haring HU, et al. Relationships of body composition and liver fat content with insulin resistance inobesity-matched adolescents and adults. Obesity. 2014;22:1325–31.
Nawarycz T, So HK, Choi KC, Sung RY, Li AM, Nelson EA, et al. Waist-to-height ratio as a measure of abdominal obesity in southern Chinese and European children and adolescents. Int J Obes. 2016;40:1109–18.
Khoury M, Manlhiot C, McCrindle BW. Role of the waist/height ratio in the cardiometabolic risk assessment of children classified by body mass index. J Am Coll Cardiol. 2013;62:742–51.
Chen Y, Ma L, Ma Y, Wang H, Luo J, Zhang X, et al. A national school-based health lifestyles interventions among Chinese children and adolescents against obesity: rationale, design and methodology of a randomized controlled trial in China. BMC Public Health. 2015;15:210.
Fang C, Wang Z, Xu G. Spatial-temporal characteristics of PM2.5 in China: a city-level perspective analysis. J Geogr Sci 2016;26:1519–32.
NHBPEP. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:24.
Myers GL, Cooper GR, Winn W, Smith SJ. The Centers for Disease Control-National Heart, Lung and Blood Institute Lipid Standardization Program. An approach to accurate and precise lipid measurements. Clin Lab Med.1989;9:31.
Doran B, Guo Y, Xu J, Weintraub H, Mora S, Maron DJ, et al. Prognostic value of fasting versus nonfasting low-density lipoprotein cholesterol levels on long-term mortality: insight from the National Health and Nutrition Examination Survey III (NHANES-III). Circulation. 2014;130:546–53.
Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr Res Rev. 2010;23:247–69.
McCrindle BW, Kwiterovich PO, McBride PE, Daniels SR, Kavey RE. Guidelines for lipid screening in children and adolescents: bringing evidence to the debate. Pediatrics. 2012;130:353–6.
Onis Md, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–7.
Zimmet P, Alberti KGMM, Kaufman F, Tajima N, Silink M, Arslanian S, et al. The metabolic syndrome in children and adolescents—an IDF consensus report. Pediatric Diabetes. 2007;8:299–306.
Jacobson TA, Maki KC, Orringer CE, Jones PH, Kris-Etherton P, Sikand G, et al. National lipid association recommendations for patient-centered management of dyslipidemia: part 2. J Clin Lipidol. 2015;9(6 Suppl):S1–122 e121.
Hacke C, Weisser B. Effects of parental smoking on exercise systolic blood pressure in adolescents. J Am Heart Assoc. 2015;4:e001936.
Thompson ML, Myers JE, Kriebel D. Prevalence odds ratio or prevalence ratio in the analysis of cross sectional data: what is to be done? Occupat Environ Med. 1998;55:272–7.
Sander G. Model-based estimation of relative risks and other epidemiologic measures in studies of common outcomes and in case-control studies. Am J Epidemiol. 2004;160:301–5.
Skov T, Deddens J, Petersen MR, Endahl L. Prevalence proportion ratios: estimation and hypothesis testing. Int J Epidemiol. 1998;27:91.
Ye P, Yan Y, Ding W, Dong H, Liu Q, Huang G, et al. Prevalence of metabolic syndrome in Chinese children and adolescents: a meta-analysis. Zhong Hua Liu Xing Bing Xue Za Zhi. 2015;36:884–88.
JI CY, Chen TJ. China WGoOi. Empirical changes in the prevalence of overweight and obesity among Chinese students from 1985 to 2010 and corresponding preventive strategies. Biomed Environ Sci. 2013;26:1–12.
Song P, Yu J, Chang X, Wang M, An L. Prevalence and correlates of metabolic syndrome in chinese children: the China Health and Nutrition Survey. Nutrients.2017;9:79.
Skinner AC, Perrin EM, Moss LA, Skelton JA. Cardiometabolic risks and severity of obesity in children and young adults. N Engl J Med.2015;373:1307–17.
Rao G. Prevention or reversal of cardiometabolic diseases. J Clin Prev Cardiol. 2018;7:22–8.
United Nations Sustainable Development Knowledge Platform. Transforming our world: the 2030 Agenda for Sustainable Development. New York, NY: United Nations Department of Economic and Social Affairs; 2015. https://sustainabledevelopment.un.org/post2015/transformingourworld. Accessed 17 Aug 2018.
Sardinha LB, Santos DA, Silva AM, Grontved A, Andersen LB, Ekelund U. A comparison between BMI, waist circumference, and waist-to-height ratio for identifying cardio-metabolic risk in children and adolescents. PLoS ONE. 2016;11:e0149351.
Ashley-Martin J, Ensenauer R, Maguire B, Kuhle S. Predicting cardiometabolic markers in children using tri-ponderal mass index: a cross-sectional study. Arch Dis Child. 2019. archdischild-2018-316028.
Ramírez-Vélez R, Correa-Bautista EJ, Carrillo AH, González-Jiménez E, Schmidt-RioValle J, Correa-Rodríguez M, et al. Tri-ponderal mass index vs. fat mass/height3 as a screening tool for metabolic syndrome prediction in colombian children and young people. Nutrients. 2018;10:412.
Acknowledgements
The authors greatly appreciated the Educational Administration Leaderships and primary and middle school health nurses who worked hard on data collection. The present research was supported by funding of National Natural Science Foundation of China (No. 81673192) and the funding of Excellent Talents Fund Program of Peking University Health Science Center (BMU2017YJ002). JM, YS, and ZZ were co-investigators and designer of the original study, XW carried out the initial data analysis, BD. and LA supervised the procedure. All authors were involved in writing the manuscript and had final approval of the submitted and published versions. XW took full responsibility for the whole work.
Funding
This work was supported by the funding of National Natural Science Foundation of China (No. 81673192) awarded to JM and the funding of Excellent Talents Fund Program of Peking University Health Science Center (BMU2017YJ002) awarded to BD. These funding sources had no role in the design of this study and did not have any role during its execution, analyses, interpretation of the data, or decision to submit results.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Wang, X., Dong, B., Ma, J. et al. Role of tri-ponderal mass index in cardio-metabolic risk assessment in children and adolescents: compared with body mass index. Int J Obes 44, 886–894 (2020). https://doi.org/10.1038/s41366-019-0416-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0416-y