Abstract
Background
Hearing loss is a disabling condition whose prevalence rises with age. Obesity—a risk factor common to many non-communicable diseases—now appears to be implicated. We aimed to determine: (1) cross-sectional associations of body composition measures with hearing in mid-childhood and mid-life and (2) its longitudinal associations with 10-year body mass index (BMI) trajectories.
Methods
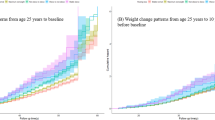
Design & Participants: There were 1481 11–12-year-old children and 1266 mothers in the population-based cross-sectional CheckPoint study nested within the Longitudinal Study of Australian Children (LSAC). Anthropometry (CheckPoint): BMI, fat/fat-free mass indices, waist-to-height ratio; LSAC wave 2–6-biennial measured BMI. Audiometry (CheckPoint): Mean hearing threshold across 1, 2 and 4 kHz; hearing loss (threshold > 15 dB HL, better ear). Analysis: Latent class models identifying BMI trajectories; linear/logistic regression quantifying associations of body composition/trajectories with hearing threshold/loss.
Results
Measures of adiposity, but not fat-free mass, were cross-sectionally associated with hearing. Fat mass index predicted the hearing threshold and loss in children (β 0.6, 95% confidence interval (CI) 0.3–0.8, P < 0.001;, odds ratio (OR) 1.2, 95% CI 1.0–1.4, P = 0.05) and mothers (β 0.8, 95% CI 0.5–1.2, P < 0.001; OR 1.2, 95% CI 1.1–1.4, P = 0.003). Concurrent obesity (OR 1.5, 95% CI 1.1–2.1, P = 0.02) and waist-to-height ratio (WHtR) ≥ 0.6 (OR 1.6, 95% CI 1.2–2.3, P = 0.01) predicted maternal hearing, with similar but attenuated patterns in children. In longitudinal analyses, mothers’, but not children’s, BMI trajectories predicted hearing (OR for severely obese 3.0, 95% CI 1.4–6.6, P = 0.01).
Conclusions
Concurrent adiposity and decade-long BMI trajectories showed small, but clear, associations with poor hearing in mid-life women, with emergent patterns by mid-childhood. This suggests that obesity may play a role in the rising global burden of hearing loss. Replication and mechanistic and body compositional studies could elucidate possible causal relationships.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Chia EM, Wang JJ, Rochtchina E, Cumming RR, Newall P, Mitchell P. Hearing impairment and health-related quality of life: the Blue Mountains Hearing Study. Ear Hear. 2007;28:187–95.
Huddle MG, Goman AM, Kernizan FC, et al. The economic impact of adult hearing loss: a systematic review. JAMA Otolaryngol Head Neck Surg 2017;143(10):1040–8.
Wang J, le Clercq CMP, Sung V, et al. Cross-sectional epidemiology of hearing loss in Australian children aged 11-12 years old and 25-year secular trends. Arch Dis Child 2018;103(6):579–85.
Wang J, Sung V, le Clercq CM, et al. High prevalence of slight and mild hearing loss across mid-life: a cross-sectional national Australian study. Submitted to Public Health 2018.
Lin FR, Thorpe R, Gordon-Salant S, Ferrucci L. Hearing loss prevalence and risk factors among older adults in the United States. J Gerontol A. 2011;66:582–90.
Gates GA, Mills JH. Presbycusis. Lancet. 2005;366:1111–20.
Kvestad E, Czajkowski N, Krog NH, Engdahl B, Tambs K. Heritability of hearing loss. Epidemiology. 2012;23:328–31.
Nelson DI, Nelson RY, Concha-Barrientos M, Fingerhut M. The global burden of occupational noise-induced hearing loss. Am J Ind Med. 2005;48:446–58.
Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988-94 through 2013-4. JAMA. 2016;315:2292–9.
Shargorodsky J, Curhan SG, Curhan GC, Eavey R. Change in prevalence of hearing loss in US adolescents. JAMA. 2010;304:772–8.
Gates GA, Cobb JL, D’Agostino RB, Wolf PA. The relation of hearing in the elderly to the presence of cardiovascular disease and cardiovascular risk factors. Arch Otolaryngol Head Neck Surg. 1993;119:156–61.
Horikawa C, Kodama S, Tanaka S, et al. Diabetes and risk of hearing impairment in adults: a meta-analysis. J Clin Endocrinol Metab. 2013;98:51–58.
Rosenhall U, Sundh V. Age-related hearing loss and blood pressure. Noise Health. 2006;8:88.
Uchida Y, Sugiura S, Ando F, Nakashima T, Shimokata H. Molecular genetic epidemiology of age-related hearing impairment. Auris Nasus Larynx. 2011;38:657–65.
Yamasoba T, Lin FR, Someya S, Kashio A, Sakamoto T, Kondo K. Current concepts in age-related hearing loss: epidemiology and mechanistic pathways. Hear Res. 2013;303:30–38.
Jung da J, Jang JH, Lee KY. Is body mass index associated with the development of age-related hearing impairment in Koreans? The Korean National Health and Nutrition Examination Survey 2009-12. Clin Exp Otorhinolaryngol. 2016;9:123–30.
Barrenas ML, Jonsson B, Tuvemo T, Hellstrom PA, Lundgren M. High risk of sensorineural hearing loss in men born small for gestational age with and without obesity or height catch-up growth: a prospective longitudinal register study on birth size in 245,000 Swedish conscripts. J Clin Endocrinol Metab. 2005;90:4452–6.
Fransen E, Topsakal V, Hendrickx JJ, et al. Occupational noise, smoking, and a high body mass index are risk factors for age-related hearing impairment and moderate alcohol consumption is protective: a European population-based multicenter study. J Assoc Res Otolaryngol. 2008;9:264–76. 261-3
Lalwani AK, Katz K, Liu YH, Kim S, Weitzman M. Obesity is associated with sensorineural hearing loss in adolescents. Laryngoscope. 2013;123:3178–84.
O’Donovan G, Owen A, Kearney EM, et al. Cardiovascular disease risk factors in habitual exercisers, lean sedentary men and abdominally obese sedentary men. Int J Obes (Lond). 2005;29:1063–9.
Romero-Corral A, Somers VK, Sierra-Johnson J, et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond). 2008;32:959–66.
Davis A, McMahon CM, Pichora-Fuller KM, et al. Aging and hearing health: the life-course approach. Gerontologist. 2016;56:S256–267.
Sanson A, Johnstone R. ‘Growing Up in Australia’ takes its first steps. Fam Matters. 2004;67:46–53.
Edwards B. Growing Up in Australia: the Longitudinal Study of Australian Children: entering adolescence and becoming a young adult. Fam Matters. 2014;95:5.
Norton A, Monahan K. LSAC technical paper No. 15: Wave 6 weighting and non-response. Australian Institute of Family Studies 2015.
Wake M, Clifford S, York E, et al. Introducing Growing Up in Australia’s Child Health CheckPoint: a physical health and biomarkers module for the Longitudinal Study of Australian Children. Fam Matters. 2014;95:15–23.
Clifford S, Davies S, Wake M. Growing Up in Australia’s Child Health CheckPoint cohort summary and methodology. BMJ Open. 2017. In press.
Vidmar S, Carlin J, Hesketh K, Cole T. Standardizing anthropometric measures in children and adolescents with new functions for egen. Stata J. 2004;4:50–55.
Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data 2000:1-27.
Flegal KM, Ogden CL. Changes in terminology for childhood overweight and obesity. National Health Statistics Reports; 2010.
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 2000;894:i-xii, 1-253.
Khoury M, Manlhiot C, McCrindle BW. Role of the waist/height ratio in the cardiometabolic risk assessment of children classified by body mass index. J Am Coll Cardiol. 2013;62:742–51.
Khoury M, Manlhiot C, Dobbin S, et al. Role of waist measures in characterizing the lipid and blood pressure assessment of adolescents classified by body mass index. Arch Pediatr Adolesc Med. 2012;166:719–24.
Teunisse RJ, Olde Rikkert MG. Prevalence of musical hallucinations in patients referred for audiometric testing. Am J Geriatr Psychiatry. 2012;20:1075–7.
Clark JG. Uses and abuses of hearing loss classification. ASHA. 1981;23:493–500.
Cone BK, Wake M, Tobin S, Poulakis Z, Rickards FW. Slight-mild sensorineural hearing loss in children: audiometric, clinical, and risk factor profiles. Ear Hear. 2010;31:202–12.
Ecob R, Russ S, Davis A. BMI over the lifecourse and hearing ability at age 45 years: a population based study. Longitud Life Course Stud. 2011;2:242–59.
le Clercq CMP, van Ingen G, Ruytjens L, et al. Prevalence of hearing loss among children 9 to 11 years old: the Generation R Study. JAMA Otolaryngol Head Neck Surg. 2017;27:10.
Jones BL, Nagin DS. A Stata plugin for estimating group-based trajectory models. Pittsburgh: Carnegie Mellon University; 2012.
Andruff H, Carraro N, Thompson A, Gaudreau P, Louvet B. Latent class growth modelling: a tutorial. Tutor Quant Methods Psychol. 2009;5:11–24.
Helgeson VS, Snyder P, Seltman H. Psychological and physical adjustment to breast cancer over 4 years: identifying distinct trajectories of change. Health Psychol. 2004;23:3.
Nagin DS. Analyzing developmental trajectories: a semiparametric, group-based approach. Psychol Methods. 1999;4:139.
Ucler R, Turan M, Garca F, Acar I, Atmaca M, Cankaya H. The association of obesity with hearing thresholds in women aged 18-40 years. Endocrine. 2016;52:46–53.
Kim TS, Park SW, Kim DY, Kim EB, Chung JW, So HS. Visceral adipose tissue is significantly associated with hearing thresholds in adult women. Clin Endocrinol (Oxf). 2014;80:368–75.
Kang SH, Jung DJ, Choi EW, et al. Visceral fat area determined using bioimpedance analysis is associated with hearing loss. Int J Med Sci. 2015;12:946–51.
Weber DR, Leonard MB, Shults J, Zemel BS. A comparison of fat and lean body mass index to BMI for the identification of metabolic syndrome in children and adolescents. J Clin Endocrinol Metab. 2014;99:3208–16.
Dai S, Eissa MA, Steffen LM, Fulton JE, Harrist RB, Labarthe DR. Associations of BMI and its fat-free and fat components with blood lipids in children: Project HeartBeat! Clin Lipidol. 2011;6:235–44.
Curhan SG, Eavey R, Wang M, Stampfer MJ, Curhan GC. Body mass index, waist circumference, physical activity, and risk of hearing loss in women. Am J Med. 2013;126:1142 e1141–1148.
Kim SH, Won YS, Kim MG, Baek YJ, Oh IH, Yeo SG. Relationship between obesity and hearing loss. Acta Otolaryngol. 2016;136:1046–50.
Lavie CJ, De Schutter A, Patel DA, Milani RV. Body composition and fitness in the obesity paradox—body mass index alone does not tell the whole story. Prev Med. 2013;57:1–2.
Price GM, Uauy R, Breeze E, Bulpitt CJ, Fletcher AEWeight. shape, and mortality risk in older persons: elevated waist-hip ratio, not high body mass index, is associated with a greater risk of death. Am J Clin Nutr. 2006;84:449–60.
Lavie CJ, Alpert MA, Arena R, Mehra MR, Milani RV, Ventura HO. Impact of obesity and the obesity paradox on prevalence and prognosis in heart failure. JACC Heart Fail. 2013;1:93–102.
Williams J, Wake M, Campbell M. Comparing estimates of body fat in children using published bioelectrical impedance analysis equations. Pediatr Obes. 2007;2:174–9.
Hwang JH, Hsu CJ, Yu WH, Liu TC, Yang WS. Diet-induced obesity exacerbates auditory degeneration via hypoxia, inflammation, and apoptosis signaling pathways in CD/1 mice. PLoS One. 2013;8:e60730.
Chudek J, Wiecek A. Adipose tissue, inflammation and endothelial dysfunction. Pharmacol Rep. 2006;58:Suppl:81–88.
Nash SD, Cruickshanks KJ, Zhan W, et al. Long-term assessment of systemic inflammation and the cumulative incidence of age-related hearing impairment in the epidemiology of hearing loss study. J Gerontol A. 2014;69:207–14.
Verschuur C, Agyemang-Prempeh A, Newman TA. Inflammation is associated with a worsening of presbycusis: evidence from the MRC national study of hearing. Int J Audiol. 2014;53:469–75.
Verschuur CA, Dowell A, Syddall HE, et al. Markers of inflammatory status are associated with hearing threshold in older people: findings from the Hertfordshire Ageing Study. Age Ageing. 2012;41:92–97.
Liew G, Wong TY, Mitchell P, Newall P, Smith W, Wang JJ. Retinal microvascular abnormalities and age-related hearing loss: the Blue Mountains hearing study. Ear Hear. 2007;28:394–401.
Liu H, Luo H, Yang T, Wu H, Chen D. Association of leukocyte telomere length and the risk of age-related hearing impairment in Chinese Hans. Sci Rep. 2017;7:10106.
Acknowledgements
This article uses unit-record data from Growing Up in Australia, the Longitudinal Study of Australian Children. The study is conducted in partnership between the Department of Social Services, the Australian Institute of Family Studies and the Australian Bureau of Statistics. The findings and views reported in this paper are solely those of the authors. M.W. and J.W. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of data analysis. Research Electronic Data Capture (REDCap) tools were used in this study. More information about this software can be found at: www.project-redcap.org. We thank the LSAC and CheckPoint study participants, staff and students for their contributions.
Funding
This work was supported by the Australian National Health and Medical Research Council (NHMRC) Project Grants 1041352 and 1109355, The Royal Children’s Hospital Foundation (2014-241), the Murdoch Children’s Research Institute, the University of Melbourne, the National Heart Foundation of Australia (100660), Financial Markets Foundation for Children (2014-055, 2016-310) and the Victorian Deaf Education Institute. The funding bodies did not play any role in the study. The following authors were supported by the NHMRC: V.S. (Early Career Fellowship 1125687), K.L. (Early Career Fellowship APP1091124), P.C. (Centre of Research Excellence in Child Language 1023493), R.L. (Postgraduate Scholarship 1114567) and M.W. (Senior Research Fellowship 1046518) in this work. V.S. was additionally supported by the Cottrell Research Fellowship from the Royal Australasian College of Physicians, K.L. by the National Heart Foundation Postdoctoral Fellowship (101239) and M.W. by Cure Kids, New Zealand.
Author contribution
M.W. conceived and led the CheckPoint study with the CheckPoint team and was LSAC’s Health Design Leader. M.W. was the primary student supervisor along with V.S. and oversaw all aspects of the study and the manuscript preparation. R.L. contributed to hearing data collection and, under the guidance of P.C., designed the hearing protocols. T.O. led the body composition measures. J.W. and K.L. conducted data extraction, cleaning and handling. J.W. performed data analysis and wrote the main paper. M.W., T.O., P.C., S.Z. and A.G. advised on statistical issues and interpretation. All authors critically reviewed the manuscripts and had the final approval of the submitted and published version of this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Wang, J., Sung, V., Lycett, K. et al. How body composition influences hearing status by mid-childhood and mid-life: The Longitudinal Study of Australian Children. Int J Obes 42, 1771–1781 (2018). https://doi.org/10.1038/s41366-018-0170-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0170-6
This article is cited by
-
A bidirectional Mendelian randomisation study to evaluate the relationship between body constitution and hearing loss
Scientific Reports (2023)
-
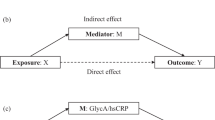
Does inflammation mediate the association between obesity and hearing status in mid-childhood and mid-life?
International Journal of Obesity (2022)
-
Body mass index, waist circumference, and risk of hearing loss: a meta-analysis and systematic review of observational study
Environmental Health and Preventive Medicine (2020)
-
Do body mass index and waist-to-height ratio over the preceding decade predict retinal microvasculature in 11–12 year olds and midlife adults?
International Journal of Obesity (2020)