Abstract
Background
We examined changes in the causes and circumstances of death in our neonatal intensive care unit (NICU) over 20 years.
Methods
For 551 infants who died between 1993 and 2013, the principal cause of death was recorded. Circumstances of death were assigned to one of the following four categories: death following cardiopulmonary resuscitation (CPR), death while being mechanically ventilated without CPR, death after withholding life-support interventions, and death after withdrawal of life support. Data were compared across four 5-year epochs.
Results
The mortality rate decreased from 5.9% in the first epoch to 3.0% in the last epoch (P<0.0001). The leading cause of death in all epochs was congenital anomalies. The percentage of deaths due to all other categories decreased or remained stable. Withdrawal of life support was the most common circumstance of death in all four epochs. Only 16% of deaths followed CPR. The percentage of neonates with documented do-not-resuscitate orders was highest in the final cohort (52%).
Conclusions
The mortality rate per admission decreased between 1993 and 2013. Each cause of death was stable or decreased as a percentage of all deaths except for deaths due to congenital anomalies. Withdrawal of life-support interventions is the most common circumstance of death in neonates.
Similar content being viewed by others
Main
Increased knowledge about normal neonatal physiology coupled with advances in both medicine and technology has led to significant progress in reducing infant mortality in the US over the past half century. It was hypothesized at the beginning of the twenty-first century that the US infant mortality rate would plateau following widespread use of surfactant (1, 2); however, infant mortality has continued to decline during recent decades. In 1993, there were 8.3 infant deaths per 1,000 live births (3), whereas in 2013 there were 6.0 infant deaths per 1,000 live births (4). This represents a 28% decrease in the infant mortality rate over a 20-year period.
Although the infant mortality rate in the US continues to decrease, the causes of death have shifted. A major contributor to the decline in infant mortality in the United States is the decline in neonatal deaths associated with low birth weight (5). Despite this change, it is clear that deaths occurring in the neonatal intensive care unit (NICU) continue to have a major impact on infant mortality. For this reason, we believed that it would be of interest to document the evolution of the leading causes of death in our Level IV NICU and the circumstances surrounding death. Understanding the major causes of death in the NICU and identifying modifiable factors contributing to the major causes have the potential to further reduce infant mortality. In addition, deaths in the NICU are often confounded by questions of whether initiation or continuation of intensive care is appropriate. Neonatologists and patients’ families are often confronted with challenging end-of-life decisions and are more frequently deciding to withhold or withdraw life support for infants judged to have incurable disorders or high probability of future disability (6). An additional goal of this study was to gain a greater understanding of end-of-life decision-making and the role of palliative care in the NICU in the hope that this may help in future decision-making and counseling of families.
Methods
This is a retrospective descriptive study involving infants who died in the NICU of the University of Iowa Children’s Hospital, a Level IV NICU with an on-site delivery service, between 1 July 1993 and 30 June 2013. Our NICU is the sole comprehensive neonatal unit in the state, and it admits patients from a local and regional population. There were 551 deaths during this period. Stillborn infants and infants who died in the delivery room were excluded. The medical records of all infants who died in the NICU were reviewed. The study was approved by the institutional review board of the University of Iowa.
Variables abstracted from the individual medical records were as follows: gestational age, birth weight, sex, outborn vs. inborn, singleton vs. multiple birth, age at death, principal cause of death, circumstances of death, documentation of parental involvement in end-of-life decision making, presence or absence of a do-not-resuscitate (DNR) order, and palliative care team involvement.
The principal cause of death was determined by the NICU medical director and was assigned to one of 13 distinct categories. Congenital anomaly included any congenital malformation incompatible with life or requiring major medical or surgical intervention to maintain life. Death from extreme prematurity was defined as death in an infant of gestational age less than 24 weeks with no other identifiable cause of death. Other categories included the following: respiratory distress syndrome, bronchopulmonary dysplasia, infection, acquired bowel disease, central nervous system injury, pulmonary hypertension, pulmonary hemorrhage, renal failure, hemorrhagic or hypovolemic shock, multisystem failure, and others for those diagnoses that did not fit into the above categories.
Circumstances of death were categorized into one of the following four options: (i) death following cardiopulmonary resuscitation (CPR), (ii) death while mechanically ventilated without CPR, (iii) death after with holding life-support interventions, and (iv) death after withdrawal of life-support interventions. When applicable, the documented reason for limitation of care was categorized using specific language as documented in the infant’s discharge summary. Categories included the following: (i)poor developmental prognosis, (ii) perceived futility of treatment in the face of limited life expectancy, and (iii) suffering resulting from continuing treatment.
Parental involvement in end-of-life decision-making was determined by the presence of documented discussion with parents regarding a plan for the infant’s death. Timing of this discussion was defined as the first documented discussion where poor prognosis was discussed and a decision was made regarding end-of-life plans. If a discussion with the family regarding end-of-life care occurred or if parents were documented as present at the time of death, they were considered as having been involved in the end-of-life decision. Other variables related to end-of-life decision-making were abstracted from medical records including the presence of a DNR order and palliative care-team involvement.
Data were entered into a REDCap database (7) and compared across four distinct 5-year epochs: Epoch 1 (1 July 1993 through 30 June 1998), Epoch 2 (1 July 1998 through 30 June 2003), Epoch 3 (1 July 2003 through 30 June 2008), and Epoch 4 (1 July 2008 through 30 June 2013).
Analyses were conducted with SAS 9.3 (Cary, NC). Descriptive statistics for population characteristics, circumstances, and means of death were obtained. χ2 and logistic regression analyses were used to compare categorical variables across epochs. Wilcoxon rank-sum tests and generalized linear modeling were used to compare continuous variables across the four epochs. P<0.05 was considered to be statistically significant.
Results
Over the 20-year study period, there were 13,952 admissions to the NICU of the University of Iowa Children’s Hospital. The mortality rate relative to admissions declined steadily over the 20-year period: 5.9% in Epoch 1, 4.0% in Epoch 2, 3.4% in Epoch 3, and 3.0% in Epoch 4. This decrease in the mortality rate was statistically significant (P≤0.0001). Both the mean gestational age and the mean birth weight of infants who died in the NICU trended upward over time; however, these changes were not statistically significant. The patient characteristics did not vary significantly among epochs (Table 1). The mean age at death increased from 18 days in Epoch 1 to 35 days in Epoch 4 (P=0.021).
The leading cause of death in all four epochs was congenital anomalies. The number of infants dying each year from major anomalies was relatively stable. The percentage of deaths due to anomalies trended upward, but this increase was not statistically significant (P=0.38; Table 2). The second and third leading causes of death in all epochs were central nervous system injury and infection, respectively. Comparing across epochs, the rates of death due to infection and extreme prematurity both decreased over the 20-year study period. There was a decrease in deaths due to infection from 0.687 to 0.249 per 100 admissions; however, this change was not statistically significant. The decline in deaths due to extreme prematurity was statistically significant (P=0.0008). The percentage of deaths due to all other categories remained relatively stable with no statistically significant change over time (Table 2).
Regarding the circumstances of death, the majority of deaths in the NICU occurred after withdrawal of life-support interventions (74%). Over the 20-year study period, only 16% of deaths were preceded by CPR. The percentage of infant deaths following CPR declined from 21% in Epoch 1 to 16% in Epoch 4; however, this change was not statistically significant (P=0.084; Table 3). Concerning infant deaths that occurred following limitation of care, the most commonly documented reasons were futility of treatment in the face of limited life expectancy (65%) and poor developmental prognosis (32%).
As documented in the medical records, parental involvement in the end-of-life decision-making process was found to occur in 92% of cases across the 20-year study period. Rates of parental involvement in direction of end-of-life care did not significantly change over time (P=0.66). The average time between documented discussion of end-of-life decisions and infant death increased over time, from 0.37 to 1.76 days; this change was statistically significant (P<0.0001). The percentage of neonates who died with a documented DNR order, regardless of circumstances of death, was greatest during the final epoch, 52%; however, this increase was not statistically significant (P=0.13; Table 3).
Palliative care-team involvement in the NICU was first documented in July 2009. Documented involvement of the palliative care team increased each year within the final epoch. During the 4 years of the study in which the palliative care team was available for consultation in the NICU, the team was consulted in 54% of cases that resulted in death.
Discussion
The death rate per NICU admission decreased over the 20-year period of study, from 5.9% in the first epoch (1993–1998) to 3.0% in the last epoch (2008–2013). This represents a 49% decrease in the mortality rate over a 20-year period. Congenital anomalies were the leading cause of death in all epochs. This is in agreement with other studies using various methodologies, which found congenital anomalies to be among the leading causes of neonatal mortality (4, 8, 9, 10, 11). In our study, the high proportion of deaths due to congenital anomalies was not due to an increase in the absolute number of infants dying each year from major anomalies, but because deaths from other causes declined. Most notably, deaths due to infection and extreme prematurity decreased, and opportunities remain for further reduction of mortality due to these causes. It should be noted that, in the final epoch, no deaths were characterized as solely due to extreme prematurity. This was due to both improved diagnostic capabilities and a conscious decision by the medical director to define a more specific cause of death in such cases. Despite this change in coding, it is interesting to note that both the mean gestational age and the mean birth weight of infants who died in the NICU tended to increase over time, which supports the conclusion that deaths secondary to extreme prematurity have decreased at our institution. In addition, other causes of death known to be direct consequences of prematurity did not increase.
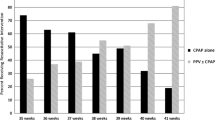
Although we are aware of no similar study of this breadth and duration from a US institution, our results are consistent with a multi-institution study that examined the causes and timing of death among extremely premature infants over a 10-year period (12). Patel et al. found that overall mortality declined among infants of gestational age 28 weeks and less born between 2000 and 2011; moreover, as gestational age increased, the percentage of deaths contributed to congenital anomalies also increased (12).
Our study shows that the majority of deaths in our unit are preceded by end-of-life decisions. Most deaths occurred without CPR, and 74% occurred following withdrawal of life support. This finding is similar to other recent studies in North America and Europe, indicating that removal of life-sustaining support is the primary mode of neonatal death, occurring in 62–93% of cases (6, 11, 13, 14, 15). These findings were unchanged throughout our 20-year study period. The most common reason for withdrawal of intensive care was perceived futility of treatment; the second most common reason was perceived poor developmental prognosis. Withdrawal of life-sustaining support as the primary neonatal mode of death reflects a change from earlier studies, such as the groundbreaking study by Duff and Campbell of neonatal deaths from 1970 to 1972, which documented that the majority of deaths (86%) at their institution occurred following full resuscitation (16).
The study by Duff and Campbell was also one of the first to explore ethical questions about various aspects of intensive care for critically ill infants as well as the involvement of the parents in these decisions (16). It was not until 1996, more than 20 years later, that a statement from the American Academy of Pediatrics explored the ethical controversy surrounding the treatment of dying neonates. This publication formally recommended parental involvement in the end-of-life decision-making process for critically ill pediatric patients (17). In our study, parental involvement in end-of-life decisions was documented in 92% of cases. A question that arises is the long-term implication of this high rate of parental involvement. Does shared decision-making make a difference in helping parents grieve or is it better to relieve the parents of responsibility for the decision and allow the physician to make the final decision regarding end-of-life care? Caeymaex et al. found that in decisions to withdraw or withhold treatment, parental perception of a shared decision is associated with a lower grief-score years after the child’s death (18).
Our study found that the average time between documented discussion of end-of-life decisions and time of infant death was relatively stable over the first 15 years of the study, and then increased significantly in the final 5-year epoch. This could be due to multiple factors. One possible explanation is that conversations regarding end-of-life decisions for infants with major congenital anomalies tend to take place earlier than those for neonates with severe illness or imminent death. These conversations often take place out of concern for future quality of life and likely require more time and contemplation than conversations that focus on the futility of continued treatment. Although our study did not specifically associate diagnosis with reason for limitation of care, a recent study found that nonterminal redirection of care (where quality-of-life considerations were considered) was most common in patients with severe central nervous system complications (9). It seems likely that this would also apply in many cases of infants with major congenital anomalies who may be physiologically more stable but have future quality-of-life concerns. In contrast, terminal redirection of care was most common in the setting of failure of other organ systems (i.e., cardiovascular or respiratory failure), where life-sustaining therapies are felt to be justified until further efforts are judged to be futile (9). Another explanation for the increased time between the family care conference and time of infant death is that palliative care-team involvement in our NICU was first introduced at the beginning of the final epoch and likely facilitated earlier end-of-life discussions with families. A recent study explored the impact of a palliative care program on end-of-life care in a NICU and found that implementation of a neonatal palliative care program did not significantly change the incidence of withdrawal of life support or overall mortality in their NICU (19). However, the authors reported that the time between the first end-of-life discussion and withdrawal of treatment was longer in those patients enrolled in the palliative care program, and DNR orders were found to be more frequent (19). A trend toward the increased use of DNR orders in the last epoch was seen in our study.
A potential limitation of our study is the retrospective design, which required reliance on review of medical records for details of care. Information about communication between the physicians and families may not have been fully documented and, in some cases, it was challenging to assess details of family participation in decision-making. However, these limitations of medical record review applied equally for the entire 20-year period and so did not affect our interpretation of changes over time. An additional limitation is that not all neonates who died in our hospital were included. We excluded the few infants who died outside of the NICU, e.g., in the delivery room, on pediatric inpatient units, or in the pediatric intensive care unit. We did not have complete records for all of these infants. Another limitation is that determining a single principal cause of death when multiple causes may have a role can be both difficult and subjective. We attempted to minimize this as a source of error by having all principal causes of death assigned using consistent criteria by one of two individuals who served as medical directors during the period of study (EFB and JMK). Another potential limitation is that the generalizability of this study may be limited in that we report the results from a single center, albeit the only comprehensive neonatal unit in our state. Despite these limitations, our study was able to achieve its goal of examining changes in the causes and circumstances of death in a large cohort of patients over a 20-year period and generate further discussions on this important topic.
Our 20-year review of deaths in our NICU showed a significant reduction in the mortality rate, from 5.9 to 3.0 deaths per 100 admissions. Congenital anomaly was the leading cause of death in all four 5-year epochs, and it became relatively more prominent as deaths from other causes declined. Our analysis also showed that most infants (75%) died after withdrawal of intensive care and that parental involvement in end-of-life decisions was documented in 92% of cases. Although deaths from infection and extreme prematurity have diminished over the years, opportunities remain for further prevention of deaths in the NICU.
References
MacDorman MF, Mathews TJ . The challenge of infant mortality: have we reached a plateau? Public Heath Rep 2009;124:670–81.
Hintz SR, Poole WK, Wright LL et al. Changes in mortality and morbidities among infants born at less than 25 weeks during the post-surfactant era. Arch Dis Child Fetal Neonatal Ed 2005;90:F128–33.
Singh GK, Mathews TJ, Clarke SC, Yannicos T, Smith BL . Annual summary of births, marriages, divorces, and deaths: United States, 1994. Monthly Vital Stat Rep 1995;43:1–44.
Mathews TJ, MacDorman MF, Thoma ME . Infant mortality statistics from the 2013 period linked birth/infant death data set. Natl Vital Stat Rep 2015;64:1–30.
Centers for Disease Control and Prevention (CDC). Public health approaches to reducing U.S. infant mortality. MMWR Morb Mortal Wkly Rep 2013;62:625–628.
Weiner J, Sharma J, Lantos J, Kilbride H . How infants die in the neonatal intensive care unit: trends from 1999 through 2008. Arch Pediatr Adolesc Med 2011;165:630–4.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG . Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81.
Callaghan WM, MacDorman MF, Rasmussen SA, Qin C, Lackritz EM . The contribution of preterm birth to infant mortality rates in the United States. Pediatrics 2006;118:1566–73.
Berger TM, Hofer A . Causes and circumstances of neonatal deaths in 108 consecutive cases over a 10-year period at the children’s hospital of Lucerne, Switzerland. Neonatology 2009;95:157–63.
Jacob J, Kamitsuka M, Clark RH, Kelleher AS, Spitzer AR . Etiologies of NICU deaths. Pediatrics 2015;135:e59–65.
Hellmann J, Knighton R, Lee SK, Shah PS, Canadian Neonatal Network End of Life Study Group. Neonatal deaths: prospective exploration of the causes and process of end-of-life decisions. Arch Dis Child Fetal Neonatal Ed 2016;101:F102–7.
Patel RM, Kandefer S, Walsh MC et al. Causes and timing of death in extremely premature infants from 2000 through 2011. N Eng J Med 2015;372:331–40.
Hagen CM, Hansen TWR . Deaths in a neonatal intensive care unit: a 10-year perspective. Pediatr Crit Care Med. 2004;5:463–8.
Simpson CDA, Ye XY, Hellmann J, Tomlinson C . Trends in cause-specific mortality at a Canadian outborn NICU. Pediatrics 2010;126:e1538–44.
Verhagen AAE, Janvier A, Leuthner SR et al. Categorizing neonatal deaths: a cross-cultural study in the United States, Canada, and the Netherlands. J Pediatr 2010;156:33–7.
Duff RS . Campbell AGM. Moral and ethical dilemmas in the special-care nursery. N Engl J Med 1973;289:890–4.
American Academy of Pediatrics, Committee on Bioethics. Ethics and the care of critically ill infants and children. Pediatrics 1996;98:149–52.
Caeymaex L, Jousselme C, Vasilescu C et al. Perceived role in end-of-life decision making in the NICU affects long-term parental grief response. Arch Dis Child Fetal Neonatal Ed 2013;98:F26–31.
Younge N, Smith PB, Goldberg RN et al. Impact of a palliative care program on end-of-life care in a neonatal intensive care unit. J Perinatol 2015;35:218–22.
Acknowledgements
This work was supported by grant UL1 RR024979 from the NIH, which supported development and use of the REDCap database.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Michel, M., Colaizy, T., Klein, J. et al. Causes and circumstances of death in a neonatal unit over 20 years. Pediatr Res 83, 829–833 (2018). https://doi.org/10.1038/pr.2018.1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2018.1
This article is cited by
-
End of life care in a level IV outborn neonatal intensive care unit
Journal of Perinatology (2024)
-
Essentials of Neonatal-Perinatal Medicine fellowship: part 2 - clinical education and experience
Journal of Perinatology (2022)
-
Compassionate extubation protocol to improve team communication and support in the neonatal intensive care unit
Journal of Perinatology (2021)
-
Physicians’ attitudes in relation to end-of-life decisions in Neonatal Intensive Care Units: a national multicenter survey
BMC Medical Ethics (2020)
-
Causes of death in preterm neonates (<33 weeks) born in tertiary care hospitals in India: analysis of three large prospective multicentric cohorts
Journal of Perinatology (2019)