Abstract
Background
The aim of this study was to estimate the prevalence of haploinsufficiency of short stature homeobox containing gene (SHOX) deficiency (SHOXD) in a population of short-statured children, and to analyze their phenotype and the performance of clinical scores.
Methods
Screening for SHOXD was performed in 281 children with short stature by direct sequencing and multiplex ligation probe-dependent amplification. Subjects with SHOXD were compared with 117 matched short patients without SHOXD. We calculated the cutoff of growth velocity associated with the highest sensitivity and specificity as a screening test for SHOXD by receiver operating characteristic curves.
Results
The prevalence of SHOXD was 6.8%. Subjects with SHOXD showed a lower growth velocity (P<0.05) and a higher prevalence of dysmorphic signs. The best cutoff for growth velocity was −1.5 standard deviation score (SDS) both in the whole population and in subjects with a Rappold score <7 and <4 points. Growth velocity was ≤−1.5 SDS or Rappold score was >7/>4 points in 17/17 of 19 children with SHOXD and in 49/65 of 117 subjects without SHOX mutations.
Conclusions
Growth rate ≤−1.5 SDS, even with negative Rappold score, may be useful to detect precociously children with SHOXD. Selecting children deserving the genetic test by using growth velocity or the Rappold score significantly increases the sensitivity in detecting mutations and decreases the specificity.
Similar content being viewed by others
Main
Haploinsufficiency of short stature homeobox containing gene (SHOX) is one of the prevalent monogenic causes of short stature. SHOX is located in the pseudoautosomal region 1 on the Xp22.33 and Yp11.32 chromosomes and encodes a transcription factor that regulates chondrocyte proliferation and differentiation in the growth plate (1). The loss of both SHOX alleles causes an extreme phenotype of skeletal dysplasia called Langer mesomelic dysplasia, while SHOX haploinsufficiency is associated with a wide spectrum of short stature phenotypes including Turner syndrome, Léri–Weill dyschondrosteosis, and idiopathic short stature (ISS) (2).
The real prevalence of SHOX deficiency (SHOXD) in children with ISS is still unknown and various studies reported a great variability (3). Current guidelines for diagnosis and treatment of children with ISS state that SHOX analysis should be considered for any patient with clinical findings compatible with SHOXD (4). However, most of the subjects with ISS and SHOXD show mild and highly variable phenotypes, especially in prepubertal age, making it difficult to identify which child should be screened (2, 5, 6, 7). Moreover, more than 380 mutations in the coding regions of the gene and mutations in the downstream or upstream enhancer elements have been identified, but a clear genotype–phenotype correlation has not been reported (5, 6, 8).
Many clinical scores have been developed to identify children deserving screening for SHOXD (5, 6). They are based on the presence of dysmorphisms and signs of skeletal dysplasia such as alterations in anthropometric measures and in some specific ratios as arm span to height and sitting height to height (5, 6). However, the sensitivity of these scores in identifying subjects with SHOXD among patients with ISS has been discussed, especially in younger children in whom skeletal disproportions are not so pronounced (6, 7).
Children carrying SHOX defects show a mild impairment of prepubertal growth followed by a compromised pubertal growth due to premature growth plate fusion, and therefore they reach a final height of around 2 standard deviation score (SDS) below the mean. In 2006, US Food and Drug Administration and European Medicines Agency approved recombinant growth hormone (rhGH) therapy for growth promotion in subjects with SHOX mutations. Several studies have shown that rhGH treatment is safe and effective in improving the final height in children with SHOXD and that the height gain is greater if treatment starts at a younger age (9, 10, 11, 12, 13).
Therefore, to start rhGH treatment as soon as possible and to optimize the results, it is essential to identify early, at a prepubertal age, subjects with SHOXD.
The aim of this study was first to estimate the prevalence of SHOXD in a large population of Italian short children with respect to international studies results. Second, we analyzed the clinical phenotypes and anthropometric parameters helpful in identifying patients with SHOX haploinsufficiency and we assessed the sensitivity and the usefulness of various scores.
Methods
This was a single-center longitudinal study conducted at the Division of Pediatrics, University of Piemonte Orientale (Novara, Italy). We consecutively recruited 281 children with short stature, aged 2–18 years between January 2012 and December 2015. The study complied with the recommendations of the Declaration of Helsinki and was approved by the Ethics Committee of Maggiore della Carità Hospital, Novara, Italy (463/CE, CE 95/12). Informed written consent was obtained from all subjects and their parents before the beginning of the study.
Inclusion criteria were the presence of short stature, defined as a height <3rd percentile according to Italian growth charts (14), or as stature below the parental target, a normal GH response to provocative tests and a normal karyotype in females. Exclusion criteria were syndromes or chromosomal defects, clear signs of any skeletal dysplasia except SHOXD, severe neurological impairments, autoimmune diseases, endocrine diseases, past or present rhGH therapy, type 1 and 2 diabetes, renal dysfunction, growth-influencing medications, alcohol or smoking, and any other condition known to influence height.
All subjects who fulfilled the inclusion criteria were analyzed for SHOX mutations by direct sequencing and multiplex ligation probe-dependent amplification (MLPA) analysis (15). Prevalence data were calculated in the overall 281 patients.
From the whole population we selected patients with a follow-up of at least 12 months and we created a database with patients’ longitudinal clinical, anthropometrical, and biochemical data. We were able to obtain all these data for 136 subjects. All patients with SHOXD (19 subjects) were compared with a population of 117 age-, gender-, and pubertal status-matched children without SHOX mutations (Figure 1).
Clinical Assessments
Height was measured to the nearest millimeter by the Harpenden stadiometer (Holtain Limited, Crymych, Pembrokeshire, UK) and weight by using an electronic scale. BMI was calculated. Height, weight, and BMI were stratified according to Italian growth charts (14). BMI SDS was assessed by the LMS (Lambda-Mu-Sigma) method (14). Growth velocity was calculated from the difference of mean heights obtained from two consecutive visits, divided by the time between the visits, and adjusted to a 12-month interval. The minimum time interval between visits to calculate growth velocity was 12 months. Target height based on the parents’ measured height was determined according to Tanner. Birth length and weight were compared with Italian neonatal standards (16). Sitting height, arm span, and forearm length were determined by trained investigators. The presence of dysmorphic signs such as micrognathia, short neck, short forearm, bowing of the forearm, cubitus valgus, dislocation of the ulna, scoliosis, muscular hypertrophy, and Madelung deformity was also investigated. The score proposed by Rappold et al. (5) was calculated. This score includes: an arm span-to-height ratio <96.5%, a sitting height-to-height ratio >55.5%, the occurrence of a BMI >50th percentile, cubitus valgus, short forearm, bowing of the forearm, muscular hypertrophy, and dislocation of the ulna.
Hormonal Assays
All the subjects performed a GH stimulation test that was defined as normal if the GH peak response, after GHRH+arginine, was ≥20 ng/ml. GH during provocative tests was measured using Commercial RIA Kits (SMC-RIA-CT; Pantec, Torino, Italy). Serum IGF-I was measured by Liason automated chemiluminescence analyzer supplied by DiaSorin (Saluggia, Vercelli, Italy) with a measurement range of 3–1,500 ng/ml. Age and gender reference ranges were used to calculate an IGF-I SDS for each patient.
Genetic Analyses of the SHOX Gene
Genomic DNA was extracted from lymphocytes using a QIAamp DNA Kit (Qiagen, Hilden, Germany). The entire coding region of the SHOX gene (exon 2–exon 6a/6b) and intron–exon boundaries were amplified by PCR. PCR conditions and primer sequences are available upon request. The PCR products were visualized on a 2% agarose gel and purified using Affymetrix ExoSAP-IT enzymatic PCR clean-up system (Santa Clara, CA, USA). The purified products were then sequenced with Big Dye Terminator Kit (Applied Biosystems, Foster City, CA) and automatic sequencer ABI PRISM 3100 Genetic Analyzer (Applied Biosystems).
Search for deletions/duplications of the single exons, of the entire gene, and of the upstream and downstream enhancers was performed by an MLPA assay using an MLPA Commercial Kit (SALSA MLPA Kit P018-G1 SHOX; MRC-Holland, Amsterdam, Netherlands) following the manufacturer’s instructions.
Statistics
Data are expressed as mean±SD or percentages. For categorical variables, the variation between groups was compared by χ2 tests. For continuous variables, the variation between groups was compared by means of nonparametric Wilcoxon’s and Mann–Whitney U-tests, as appropriate. To determine in our population the cutoff value of growth velocity, we performed ROC curve analysis. Using ROC curves, we identified the cutoff value associated with the highest sensitivity and specificity by plotting for each cutoff value sensitivity vs. (1-specificity). The area under the ROC curve and the 95% confidence interval (95% CI) were assessed. The sensitivity, specificity, positive predictive value, and negative predictive value were calculated for various scoring systems. We then compared the sensitivity and specificity of screening methods by two-tailed Fisher’s exact test or χ2 test, as appropriate. Statistical significance was assumed for P<0.05. Statistical analysis was performed with SPSS for Windows version 17.0 (SPSS, Chicago, IL) and ROC curve analysis with the MedCalc software version 11.0.1 (MedCalc Software, Mariakerke, Belgium).
Results
The total population comprised 281 patients with short stature (50.7% females, 70.8% prepubertal), the mean age was of 8.6±4.0 years and the mean height was of −2.0±0.5 SDS. In this population, we identified 19 (6.8%) unrelated patients with SHOXD who carried functionally relevant SHOX variations: one subject (5.3%) had a large deletion including the whole gene and the enhancers regions, nine children (47.3%) showed a deletion including the SHOX downstream enhancer, four children (21.1%) showed a partial intragenic or enhancer duplication, and five children (26.3%) had a point mutation in the coding region of the gene.
All patients with SHOXD (mean age 8.7±3.4 years, 57.9% females, 89.5% prepubertal, mean height SDS −2.1±0.7) were compared with a population of 117 age-, gender- and pubertal status-matched children without SHOXD proven by direct sequencing and MLPA (mean age 7.9±3.8 years, 54.7% females, 76.1% prepubertal, mean height SDS −2.0±0.6).
The anthropometrical, biochemical data, and dysmorphic signs of the 19 children with SHOXD and 117 controls without SHOX mutations are presented in Table 1.
No differences were found with respect to height, weight, BMI, or target height. The anthropometrical data at birth and the number of subjects born small for gestational age were similar in children with and without SHOXD. The GH peak at provocation test was not different between the two groups and both children with and without SHOXD showed normal values of insulin-like growth factor I (IGF-I) SDS.
Children with SHOX mutations showed significantly lower growth velocity than subjects without SHOX mutations (growth velocity SDS −1.86±0.93 vs. −0.77±2.0, P<0.05).
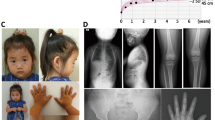
The arm span, the sitting height- and arm span-to-height and sitting height-to-height ratios were similar in the two groups. Subjects with SHOX mutations showed significantly higher prevalence of micrognathia (63.2% vs. 26.5%, P<0.01), short forearm (21.1% vs. 3.4%, P<0.01), muscular hypertrophy (36.8% vs. 14.5%, P<0.05), and Madelung deformity (15.7% vs. 1.7%, P<0.01). No difference between the two groups was found in ear’s anomalies, short neck, scoliosis, bowing of the forearm, and cubitus valgus prevalences.
The Rappold score was significantly higher in children with SHOX mutations (4.53±3.34 vs. 2.47±2.71, P<0.05). Children with SHOXD demonstrated a significantly higher prevalence of Rappold score >7 points (26.3% vs. 5.1%, P<0.01) and >4 points (36.8% vs. 16.2%, P<0.05) than subjects without SHOXD.
No differences were found for the same data between prepubertal and pubertal children.
The performance of screening criteria for SHOXD in our population is shown in Table 2. The Rappold score >4 points showed the highest sensitivity, while the Rappold score >7 points demonstrated the best positive predictive value. The negative predictive values did not differ among the various scores and the ratio between arm span and height and the Rappold score >7 points showed the highest specificity.
Using a Rappold score >7 points and >4 points, as a screening criterion to perform the genetic analyses of the SHOX gene, out of 19 children with SHOX mutations, 14 and 12 subjects would have been missed, respectively.
As growth velocity was the only anthropometric parameter significantly different between the two groups, we performed receiver operating characteristic (ROC) curve analysis to determine, in our population, the cutoff value of growth velocity associated with the highest sensitivity and specificity as a screening test for SHOX mutations. The ROC curve analysis performed on growth velocity in 19 children with SHOXD and 117 subjects without SHOX mutations showed that the cutoff value was −1.5 SDS. Figure 2 shows the ROC curve for growth velocity in the whole population. The area under the curve was 0.699 and the 95% CI was 0.613–0.775.
In subjects with a Rappold score <7 points, the cutoff value of growth velocity remained −1.5 SDS (area under the curve 0.661; 95% CI: 0.569–0.746) (Figure 3); similarly, in the Rappold score <4 points-group, the cutoff value of growth velocity was −1.5 SDS (area under the curve 0.636; 95% CI: 0.528–0.735) (Figure 4).
This cutoff did not change if the analysis was performed in prepubertal subgroup (17 subjects with SHOXD and 89 without mutations).
According to this cutoff, growth velocity was ≤−1.5 SDS or Rappold score was >7 points in 17 of 19 children with SHOXD and in 49 of 117 subjects without SHOX mutations. Growth velocity was ≤−1.5 SDS or Rappold score was >4 points in 17 of 19 children with SHOXD and in 65 of 117 controls. Table 2 shows sensitivity, specificity, positive, and negative predictive values for growth velocity or Rappold score >7 or 4 points. When comparing sensitivity of the various scoring systems, we found that growth velocity/Rappold score >7 and growth velocity/Rappold score >4 showed both a sensitivity of 89.5% and were significantly more sensitive than the other scoring systems. When comparing specificities, growth velocity/Rappold score >7 showed a higher specificity than growth velocity/Rappold score >4, but it was significantly lower compared with the other scoring systems. Moreover, growth velocity was significantly lower in subjects with SHOXD compared with children without SHOX mutations, but with a positive Rappold score for both the cutoff values of 7 and 4 points.
Discussion
The clinical diagnosis of haploinsufficiency of SHOX gene in short-statured children is still a challenge because of the mild and highly variable phenotype, especially in prepubertal age, and because of the low sensitivity of the available clinical scores.
The innovative aspect of this study was the identification of growth velocity as a helpful anthropometric parameter to improve the sensitivity of previously published clinical scores in detecting children with SHOX mutations among subjects with short stature.
In our population, the prevalence of SHOXD was 6.8%, in the upper range of previously published prevalences (1, 3, 5, 13, 17).
We identified mutations as well as deletions and duplications in both the whole gene and in the upstream and downstream enhancer domains. In line with previous reports (2, 5, 17), the majority of patients (53%) with SHOXD showed deletions of different size, which encompass the SHOX gene itself or its regulatory enhancers. Although a genotype–phenotype correlation cannot be established, both subjects with point mutations and patients with deletions or duplications showed clinical signs of SHOXD.
We found no difference in the degree of short stature between those with or without SHOX mutations; in fact, both groups had a mean height of –2.0 SDS and this is consistent with previous reports (5, 6, 7). Furthermore, we have not found any difference between patients with and without SHOXD in weight, BMI, or target height. The most striking anthropometric difference between SHOX-deficient and non-SHOX-deficient subjects was the 1.0 SDS lower growth velocity in the SHOX-deficient group. The literature shows contradictory data on growth from infancy to final height in patients with SHOX mutations. In line with our findings, some studies show that the height deficit is already present at a prepubertal age, suggesting that early childhood is a phase of growth failure (2, 6) and the absence of catch-up growth at any time (18). Conversely, other longitudinal follow-up studies show a relative well-preserved prepubertal growth followed by a compromised pubertal spurt due to a premature growth plate fusion (19, 20, 21).
The growth velocity reported in our study in children with SHOX mutations was similar to that of some previously published studies and to that of girls with Turner syndrome (9, 10, 13).
According to previous findings, the phenotype of our children with SHOXD was highly variable (2, 5, 6). Compared with children without SHOX mutations, the subjects with SHOXD showed more frequently clinical signs such micrognathia, short forearm, muscular hypertrophy, and Madelung deformity. However, these signs are highly aspecific (such as micrognathia) or appear in a small number of subjects with SHOXD (such as Madelung deformity), limiting their value to identify children with mutations. Furthermore, we have not found any difference between patients with and without SHOXD in the arm span, the sitting height, and the ratios of arm span to height and sitting height to height. This finding may be explained by the fact that the majority of our children with short stature and SHOX mutations was young and prepubertal (89.5%) and, as reported previously, skeletal disproportions become more pronounced with age (2, 7, 22).
As described previously, the negative predictive values were high in all scores and ratios proposed to identify SHOXD (2, 6, 7, 8). As expected, the ratio between arm span and height, reflecting limb shortening, and the Rappold score >7 points showed the highest specificity (5, 6). Finally, as shown previously, the Rappold score >4 points showed the highest sensitivity, while the Rappold score >7 points demonstrated the best positive predictive value (5, 7). However, in this study, using the Rappold score as a screening criterion to perform the genetic analyses of the SHOX gene, the majority of subjects with SHOX mutations would have been missed. This might be explained by the absence of pronounced skeletal disproportions in our prepubertal children and by the inclusion of the criteria BMI >50th percentile. In fact, as stated by Wolters et al. (7), the increase of BMI in childhood worldwide may mask the difference between children with and without SHOXD. Therefore, the sensitivity of the Rappold score to detect children with SHOX defects in our population of subjects with ISS is very low.
For clinicians, it is of great importance that all potential cases of SHOXD are detected to start rhGH treatment as soon as possible and to optimize results in linear growth. As discussed previously, growth velocity was the only anthropometric parameter that significantly differed between children with and without SHOX mutations. We therefore performed ROC curve analysis to determine, in our population, the growth rate’s cutoff value associated with the highest sensitivity and specificity to propose it as a screening test for SHOX mutations. This value in the whole studied population was −1.5 SDS, and interestingly, this cutoff did not change in prepubertal subgroup and in children not detected by the Rappold score. To our knowledge, none of the previously proposed screening scores included the growth rate as a criterion to identify children with SHOX mutations. Indeed, in the work of Rappold et al. (5), growth velocity was not included into the analysis, and in their algorithm, Binder et al. (2) only considered the presence of typical clinical signs in the patient or of a known mutation in a first-degree relative. Despite growth velocity is a difficult parameter to evaluate in clinical routine, its calculation during a follow-up period of at least 12 months could limit its variability. Moreover, longitudinal data demonstrated that growth failure and height deficit in SHOXD are already present at preschool age (2, 6, 18). In this work, we demonstrated that selecting children deserving the genetic test, by using growth velocity or the Rappold score, significantly increases the sensitivity in detecting SHOX mutations and decreases the specificity. Moreover, in our study, growth velocity was significantly lower in subjects with SHOXD compared with children without SHOX mutations but with a positive Rappold score. This may be explained by the fact that children with SHOXD showed a more pronounced growth delay compared to subjects with short stature but without SHOX mutations. Increasing the sensitivity of screening scores is crucial for an early start of rhGH therapy to reach the greatest height gain before the fusion of the epiphyseal growth plates. However, the parallel reduction of specificity may lead to unnecessary genetic screening and a benefit/cost analysis should be performed on larger case series.
The major limitation of our current study is the small sample of patients that might pose our results susceptible to confounding bias. Moreover, all clinical, anthropometrical, and biochemical data for a follow-up period of at least 12 months were available only for 117 control subjects. Another limit is the lack of radiological data and of the clinical helpful parameter of extremities to trunk ratio. Finally, we have not performed a cost analysis of extending the genetic test of SHOX mutations to all the subjects with a growth velocity lower than −1.5 SDS.
In conclusion, this study confirms that the phenotype of children with SHOXD is highly variable and that screening for SHOX alterations in children with a positive Rappold score is rational, even in an Italian population of subjects with short stature. Finally, this study suggests that the presence of a growth rate lower than −1.5 SDS, even in the absence of a positive Rappold score, may be a useful anthropometric parameter to detect precociously children with SHOXD.
References
Rao E, Weiss B, Fukami M et al. Pseudoautosomal deletions encompassing a novel homeobox gene cause growth failure in idiopathic short stature and Turner syndrome. Nat Genet 1997;16:54–63.
Binder G . Short stature due to SHOX deficiency: genotype, phenotype and therapy. Horm Res Paediatr 2011;75:81–89.
Nicosi A, Caruso-Nicoletti M . Epidemiology of SHOX deficiency. J Endocrinol Invest 2010;33:7–10.
Cohen P, Rogol AD, Deal CL et al. Consensus statement on the diagnosis and treatment of children with idiopathic short stature: a summary of the Growth Hormone Research Society, the Lawson Wilkins Pediatric Endocrine Society, and the European Society for Paediatric Endocrinology Workshop. J Clin Endocrinol Metab 2008;93:4210–4217.
Rappold G, Blum WF, Shavrikova EP et al. Genotypes and phenotypes in children with short stature: clinical indicators of SHOX haploinsufficiency. J Med Genet 2007;44:306–313.
Binder G, Ranke MB, Martin DD . Auxology is a valuable instrument for the clinical diagnosis of SHOX haploinsufficiency in schoolage children with unexplained short stature. J Clin Endocrinol Metab 2003;88:4891–4896.
Wolters B, Lass N, Wunsch R et al. Short stature before puberty: which children should be screened for shox deficiency? Horm Res Paediatr 2013;80:273–280.
Rosilio M, Huber-Lequesne C, Sapin H et al. Genotypes and phenotypes of children with SHOX deficiency in France. J Clin Endocrinol Metab 2012;97:E1257–E1265.
Blum WF, Ross JL, Zimmermann AG et al. GH treatment to final height produces similar height gains in patients with shox deficiency and Turner syndrome: results of a multicenter trial. J Clin Endocrinol Metab 2013;98:E1383–E1392.
Iughetti L, Vannelli S, Street ME et al. Impaired GH secretion in patients with SHOX deficiency and efficacy of recombinant human GH therapy. Horm Res Paediatr 2012;78:279–287.
Blum WF, Cao D, Hesse V et al. Height gains in response to growth hormone treatment to final height are similar in patients with SHOX deficiency and Turner syndrome. Horm Res 2009;71:167–172.
Blum WF, Crowe BJ, Quigley CA et al. Growth hormone is effective in treatment of short stature associated with short stature homeobox-containing gene deficiency: two-year results of a randomized, controlled, multicenter trial. J Clin Endocrinol Metab 2007;92:219–228.
Binder G, Schwarze CP, Ranke MB . Identification of short stature caused by SHOX defects and therapeutic effect of recombinant human growth hormone. J Clin Endocrinol Metab 2000;85:245–249.
Cacciari E, Milani S, Balsamo A et al. Italian cross-sectional growth charts for height, weight and BMI (2 to 20 yr). J Endocrinol Invest 2006;29:581–593.
Schouten JP, McElgunn CJ, Waaijer R et al. Relative quantification of 40 nucleic acid sequences by multiplex ligation-dependent probe amplification. Nucleic Acids Res 2002;30:e57.
Bertino E, Spada E, Occhi L et al. Neonatal Anthropometric Charts: The Italian neonatal study compared with other European studies. J Pediatr Gastroenterol Nutr 2010;51:353–361.
Huber C, Rosilio M, Munnich A et al. French SHOX GeNeSIS Module. High incidence of SHOX anomalies in individuals with short stature. J Med Genet 2006;43:735–739.
Ross JL, Scott C Jr, Marttila P et al. Phenotypes associated with SHOX deficiency. J Clin Endocrinol Metab 2001;86:5674–5680.
Kosho T, Muroya K, Nagai T et al. Skeletal features and growth patterns in 14 patients with haploinsufficiency of SHOX: implications for the development of Turner syndrome. J Clin Endocrinol Metab 1999;84:4613–4621.
Fukami M, Nishi Y, Hasegawa Y et al. Statural growth in 31 Japanese patients with SHOX haploinsufficiency: support for a disadvantageous effect of gonadal estrogens. Endocr J 2004;51:197–200.
Jorge AAL, Souza SC, Nishi MY et al. SHOX mutations in idiopathic short stature and Leri–Weill dyschondrosteosis: frequency and phenotypic variability. Clin Endocrinol 2007;66:130–135.
Rappold GA, Fukami M, Niesler B et al. Deletions of the Homeobox Gene SHOX (Short Stature Homeobox) are an important cause of growth failure in children with short stature. J Clin Endocrinol Metab 2002;87:1402–1406.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Genoni, G., Monzani, A., Castagno, M. et al. Improving clinical diagnosis in SHOX deficiency: the importance of growth velocity. Pediatr Res 83, 438–444 (2018). https://doi.org/10.1038/pr.2017.247
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2017.247
This article is cited by
-
Variants in the 5′UTR reduce SHOX expression and contribute to SHOX haploinsufficiency
European Journal of Human Genetics (2021)