Abstract
Background:
Apnea of prematurity (AOP) is nearly universal among very preterm infants, but neither the apnea burden nor its clinical associations have been systematically studied in a large consecutive cohort.
Methods:
We analyzed continuous bedside monitor chest impedance and electrocardiographic waveforms and oxygen saturation data collected on all neonatal intensive care unit (NICU) patients <35 wk gestation from 2009 to 2014 (n = 1,211; >50 infant-years of data). Apneas, with bradycardia and desaturation (ABDs), defined as central apnea ≥10 s associated with both bradycardia <100 bpm and oxygen desaturation <80%, were identified using a validated automated algorithm.
Results:
Number and duration of apnea events decreased with increasing gestational age (GA) and postmenstrual age (PMA). ABDs were more frequent in infants <31 wk GA at birth but were not more frequent in those with severe retinopathy of prematurity (ROP), bronchopulmonary dysplasia (BPD), or severe intraventricular hemorrhage (IVH) after accounting for GA. In the day before diagnosis of late-onset septicemia and necrotizing enterocolitis, ABD events were increased in some infants. Many infants continued to experience short ABD events in the week prior to discharge home.
Conclusion:
Frequency of apnea events is a function of GA and PMA in infants born preterm, and increased apnea is associated with acute but not with chronic pathologic conditions.
Similar content being viewed by others
Main
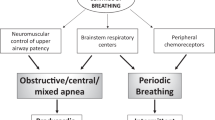
Apnea of prematurity (AOP) reflects immaturity of brainstem and peripheral chemoreceptors and occurs in essentially all infants born at <28 wk gestation and many of those born between 28–34 wk (1,2,3,4). AOP is commonly defined as cessation of breathing for >20 s, or >10 s with associated bradycardia or oxygen desaturation (5). In our research, we use the abbreviation ABDn for episodes of central apnea of at least n seconds duration, when accompanied by both bradycardia and desaturation (6). Hypoxia associated with apnea could have detrimental effects on developing tissues and organs resulting in long-term or permanent impairment (6,7,8,9,10), and therapies such as respiratory support and caffeine are only partially successful in reducing the burden of AOP (11,12). Management of refractory apnea, optimum levels and durations of various therapies, and determining readiness for discharge from the neonatal intensive care unit (NICU) continue to be major challenges, and accurate quantitation of apnea is required for both clinical care and outcomes research (13).
Quantitation of apnea in NICU patients has historically involved one of two approaches: medical record documentation of events by bedside caregivers, or short pneumographic recordings of respiratory impedance or inductance signals, heart rate, and oxygen saturation. These approaches are limited, the former by inaccuracy of reporting (14,15,16) and the latter by requirements for extra attachments to infants and time and expertise required for signal interpretation. As a result, previous studies of AOP are limited by small numbers of infants studied over short periods of time. Our group recently developed a novel automated computer algorithm for quantifying central apnea of prematurity from waveform and vital sign data continuously collected from standard NICU bedside monitors (17). This system was clinically validated and allows identification of central AOP events in large numbers of infants for the entire NICU stay.
Clinical variables affecting the severity of AOP and the timing of resolution as infants approach term-corrected age are not well defined. Prior studies have shown an inverse correlation between gestational age at birth and postmenstrual age at which apnea resolves (18,19,20). Chronic or acute pathologic processes may also impact the occurrence, severity, and duration of AOP. For example, severe intraventricular hemorrhage (IVH) may be associated with central nervous system dysfunction that could manifest as central apnea (6,21,22), and bronchopulmonary dysplasia, with associated abnormal blood oxygen and carbon dioxide levels, may be associated with dysregulation of peripheral or central chemoreceptor sensitivity and increased apnea. Acute systemic inflammatory processes such as sepsis are known to lead to an abrupt increase in apnea over baseline in some infants (23,24). It is also possible that hypoxemia association with AOP may contribute to pathology such as retinopathy of prematurity (8,10) or might contribute to neurodevelopmental impairment (7,10,25).
The goals of the current study were twofold: to provide a comprehensive assessment of the burden of central apnea throughout the NICU stay of a large number of preterm infants, and to establish the association of AOP with chronic and acute pathologic processes.
Results
Demographics, Clinical Outcomes, and Respiratory Support
Of 1,372 infants <35 wk gestation admitted to the UVA NICU during the study period, chest impedance waveform and vital sign data were available for analysis for 1,268. Figure 1 shows the type of respiratory support for each infant relative to gestational age (GA) and postmenstrual age (PMA). Fifty-seven of these infants were excluded from the apnea, with bradycardia and desaturation (ABD), analysis because they had no chest impedance data off mechanical ventilation and prior to 40 wk PMA, either due to death or transfer from our unit. Demographics and clinical outcomes of the 1,211 infants with ABDs analyzed are shown in Table 1 . Median gestational age for the entire cohort was 32 wk (25th-75th% 28–33 wk). Birthweight distribution was 235 (19%) extremely low birth weight (<1,000 g) and 521 (43%) very low birth weight (<1,500 g).
Respiratory support. Type of respiratory support over the course of the neonatal intensive care unit stay is shown for all 1,268 infants <35 wk gestational age (GA) with bedside monitor data available for analysis. Number of infants in each GA week group is shown on the right y axis, and the change in color represents mode of respiratory support with advancing postmenstrual age: ventilator (black), nasal continuous positive airway pressure (green), nasal cannula (NC, yellow), and room air (blue).
Number of ABDs Is Inversely Correlated With GA and PMA
ABD events were assessed when chest impedance, heart rate, and SpO2 data were available and infants were not on mechanical ventilation including nasal intermittent positive pressure ventilation. Median number of days analyzed per infant was 15 (25th-75th percentile 7–34 d, > 50 infant-years of data).
Figure 2a shows an example of an algorithm-detected ABD10 event, with the major features described in the caption. Figure 2b is a histogram showing the number of infants in each GA week with at least one ABD10 event during the NICU stay. Percentage of infants with at least one algorithm-detected ABD based on GA group is as follows: 97% of infants <27 wk, 92% of infants 27–30 wk, 73% of infants 31–32 wk, and 52% of infants 33–34 wk. Note that some infants with no detected ABDs may have been on prolonged mechanical ventilation or may have been transferred to our center at later PMAs for procedures.
Apnea, bradycardia, desaturation example, and incidence. Apnea at least 10 s with associated bradycardia <100 beats/min and oxygen desaturation <80% were analyzed using a published algorithm (17). (a) Graphic representation of 60 s of vital sign and waveform data showing a representative ABD event. From top to bottom: Heart rate (HR with 100 beats per minute threshold of bradycardia indicated by the thin green line), oxygen saturation (SpO2 with 80% threshold of desaturation indicated by the thin blue line), chest impedance (CI), filtered chest impedance (FCI), and computer algorithm-detected probability of apnea (PA). An “ABD10” event is shown, with apnea duration >10 seconds and associated bradycardia and oxygen desaturation. Another shorter breathing pause occurred without associated bradycardia, which did not meet our definition of an “ABD” event. (b) ABDs were analyzed on all infants all times that bedside monitor data were available and the infant was not on mechanical ventilation. Number of infants of each gestational age with at least one algorithm-detected ABD10 event (black fill) and with no events detected (white) is shown.
Figure 3 includes two heat maps of the average daily number of ABD events for all 1211 infants based on GA and PMA, with ABD10 and ABD20 shown (3A, 3B). Note that ABD20 events (apnea at least 20 s with associated bradycardia <100 and desaturation <80% of any duration) are a subset of the ABD10 events. In these heat maps, warmer colors denote more apnea events each day, and are most evident in the lower left hand corners—lower GA and PMA. ABD10s persist to later PMAs compared to ABD20s—for example, the average number of ABD10s at 34 wk PMA is 3 or more, while there is on average <1 ABD20 at 34 wk PMA. The inset of Figure 3a shows that the number of ABD10s at 32–36 wk PMA is about threefold greater for infants <31 wk GA compared to those 31–34 wk. Among the infants <31 wk GA, however, there is no significant impact of GA on the number of ABD10 at these later PMAs.
Mean number of ABD events per day based on gestational and postmenstrual age. For 1,211 infants <35 wk gestational age (GA), ABDs were analyzed during all times that data were available and infants were not on mechanical ventilation. (a) Heat map of mean daily #ABD10s (apnea at least 10 s with associated bradycardia and desaturation) for each week of GA and postmenstrual age (PMA). Color scale goes from blue (zero) to red (eight) events per day. The line graph below shows mean daily #ABD10s for infants <27 wk GA (blue), 27–30 wk (green), and 31–34 wk (red). (b) Mean daily #ABD20s (apnea at least 20 s with bradycardia and desaturation) for each week of GA and PMA.
Lack of Association of Number of ABDs With Severe ROP, BPD, and Severe IVH
Since retinopathy of prematurity (ROP) has been linked to aberrant oxygenation (8,26,27), and since apnea is a major cause of hypoxia (28,29) and rebound hyperoxia (30), we tested the hypothesis that the number of ABD events would be greater in infants who developed severe ROP requiring laser or bevacizumab therapy (Supplementary Figure S1 online). After accounting for GA, we did not find a statistically significant difference in the mean number of ABD10s throughout the NICU stay in 47 infants with treated ROP compared to those without (Supplementary Figure S1a online). We also analyzed ABDs in infants with and without severe IVH (grade III-IV) and in those with BPD, since both of these conditions might be thought to lead to increased frequency of apnea. Considering all ABD10 events throughout the NICU stay, after accounting for GA, there was no significant difference in number of apnea events in the 243 infants with BPD or the 51 infants with severe IVH (Supplementary Figure S1b,c online) compared to infants without these morbidities. We further investigated whether, at later PMA when infants are maturing and nearing NICU discharge, infants with BPD or severe IVH have more central apnea spells with bradycardia and desaturation than those without. At 35 wk PMA, we found that GA is significantly associated with BPD and severe IVH (ROC AUCs 0.927 and 0.817, respectively, P < 0.0001), but that after accounting for GA infants with BPD did not have more ABD10s at 35 wk PMA compared to babies without BPD, (ROC AUC 0.927, change in AUC 0, P = 0.63). For babies with severe IVH, there was a trend toward more ABDs at 35 wk PMA that was not statistically significant (ROC AUC 0.832, change in AUC 0.015, P = 0.085).
Apnea Increases Before Diagnosis of Late-Onset Septicemia and necrotizing enterocolitis (NEC)
Acute systemic inflammatory processes can be associated with apnea in preterm infants (23), and we therefore analyzed ABDs in these illnesses (Supplementary Figure S2 online). We identified 28 cases of late-onset septicemia and 21 cases of NEC in infants when they were not on mechanical ventilation and had chest impedance and vital sign data available for analysis >50% of the time in the 48-h period prior to diagnosis. In seven cases of NEC (33%) and 12 cases of late-onset septicemia (43%) infants had at least twofold increased ABD events in the 24-h period prior compared to 24–48 h prior to diagnosis. We also analyzed number of seconds of apnea associated with bradycardia and desaturation in the 24 h period before diagnosis compared to 24–48 h prior, and found similar results as shown in Supplementary Figure S2 online.
ABD Events in the Week Prior to Discharge Home From the NICU
We sought to determine whether infants continued to experience mild, self-resolved or not clinically recognized ABD events in the week prior to NICU discharge. Of the 1,211 infants included in this analysis, 1,048 were discharged home (the others either died or were transferred to another unit). Decisions about readiness for discharge were made by the clinical care team without knowledge of algorithm-detected ABDs. Caffeine was usually discontinued between 32–34 wk PMA, when the infant was off continuous positive airway pressure and no longer having significant clinically detected apnea events requiring stimulation. In our unit during the period of this study, there was a general policy of an 8-d “apnea countdown” with no events requiring intervention before discharge home (18). Minor apnea events that are self-resolved or that occur during feeding generally do not delay discharge, and events that occur following immunizations or general anesthesia near the time of NICU discharge do not restart the apnea countdown. Cardiorespiratory monitors are routinely prescribed for infants going home on supplemental oxygen and are occasionally prescribed for other infants with clinical conditions or events at the discretion of the medical team.
PMA for the 1,048 infants discharged home was 36.6 ± 2.7 wk. In the 7 d prior to discharge, no ABD10s were detected by the automated algorithm in 508 infants (48%), whereas 146 infants (14%) had 10 or more events ( Table 2 ). GA was significantly lower in infants with ABDs in the week before discharge, but PMA at discharge was similar for infants with and without discharge week ABDs. A home apnea monitor or pulse oximeter or both were prescribed at discharge for 168 infants (16%), including all infants discharged on supplemental oxygen and 58 infants discharged on room air. Fourteen infants not on supplemental oxygen and with no ABDs detected by our algorithm in the week prior to discharge were sent home with a monitor, while 103 babies with more than 10 ABDs detected in the week prior to discharge were sent home without a monitor.
Apparent Life-Threatening Event and sudden infant death syndrome
As shown in Table 2 , (15) infants were readmitted within 8 wk of NICU discharge for apnea or apparent life-threatening event, including 2% of infants with one or more discharge week ABDs and 0.8% of infants with no discharge week ABDs (P = 0.17).
Reviewing matched birth/death records from the state of Virginia, we found one sudden infant death syndrome death in the study population. The infant was a 32 wk GA twin discharged at 35 wk PMA who died 2 wk after NICU discharge with a forensic autopsy identifying cause of death as sudden infant death syndrome. As we previously reported, during her 3 wk in the NICU, she had excessive periodic breathing—fivefold more than other 32 wk infants—but no clinically recorded apnea and only one computer-detected ABD10 event, which did not occur in the week prior to discharge (31).
Discussion
We provide a quantitative analysis of central apnea throughout the NICU stay of 1,211 preterm infants that confirms some old concepts about AOP and challenges others. We found, as expected, that apnea accompanied by both bradycardia and oxygen desaturation is common in the NICU despite respiratory and pharmacologic treatments administered to nearly all very preterm infants. We confirmed that an acute increase in ABD events may occur in the day prior to diagnosis of an acute illness such as sepsis or NEC. On the other hand, chronic pathologic processes (ROP, BPD, IVH) were not significantly associated with the frequency of central apnea after controlling for gestational age. Finally, we found that longer apneas (ABD20s) resolve earlier than shorter ones, and ABD10 events are not uncommon in the week prior to NICU discharge of healthy preterm infants.
Limitations of the Automated Apnea Detection System
Our apnea detection algorithm requires low or absent variance in the chest impedance signal to detect cessation of breathing efforts, and thus detects only central apnea. Preterm infants also have obstructive apnea, which may or may not be accompanied by some degree of motion of the chest wall and abdomen. The algorithm filters out gross motion artifact before identifying breathing signals in the impedance waveform, but it was not designed to identify obstructive apnea. Prior studies using measures of nasal airflow (thermistors or carbon dioxide detectors) and respiratory inductance plethysmography indicate that the majority of apnea events in preterm infants have both central and obstructive components. Our methodology will miss pure obstructive events but will capture pure central and most mixed central/obstructive events.
We employed a stringent definition of apnea, requiring both bradycardia and oxygen desaturation, in order to measure the most clinically significant events. Many other studies, and the NICHD Consensus Statement (5), define AOP as cessation of breathing with bradycardia or desaturation and give slightly different thresholds for “BD”. Also, the algorithm detects ABD events irrespective of whether they are noticed or are considered clinically important. We previously reported that medical record documentation does not accurately reflect occurrence of ABD events (14), and speculate that many of the algorithm-detected events are self-resolved or are occurring during or following procedures, handling, or feeding and therefore not necessarily documented by bedside caregivers.
Finally, we are reporting only on the number of ABD events, thus we do not make any statements about depth or duration of bradycardia or oxygen desaturation.
Apnea Prior to Diagnosis of Acute Illness
An acute increase in apnea is generally thought to reflect acute stress or illness in preterm infants, and our study provides quantitative evidence of this. Apnea during septicemia or NEC is likely attributable at least in part to release of prostaglandins during a systemic inflammatory response (32,33,34). Many infants did not experience an increase in apnea during sepsis or NEC and we do not have enough cases to determine whether apnea is more likely to occur with specific organisms or reflects a higher severity of illness. Future work will focus on whether real-time analysis and display of abnormal respiratory or other vital sign patterns could provide early warning of potentially catastrophic illnesses, leading to earlier treatment and improved outcomes.
Lack of Association of Apnea Frequency and Chronic Morbidities
After accounting for gestational age, we did not find a greater number of ABD events among infants with severe ROP. Large randomized clinical trials have demonstrated that targeting lower SpO2 results in lower rates of ROP (27) but a smaller retrospective study suggested that intermittent hypoxia events are linked to more severe ROP (8). It is likely that retinal vascular pathology is related to both hyperoxia and hypoxia and to the phase of development at which aberrant SpO2 occurs. We did not analyze the timing, depth, or duration of hypoxia during apneic events, nor did we assess hypoxia occurring without central apnea (35). Most of our infants with severe ROP were ≤25 wk GA and were on prolonged mechanical ventilation, which precludes apnea but does not preclude dysoxia that might contribute to ROP.
The finding that infants with BPD did not have more central apnea was surprising, since chemoreceptor dysregulation might be expected in these infants (3). It is possible that infants with significant lung disease are on mechanical ventilation or other respiratory support and caffeine for prolonged periods of time when they are most susceptible, and thus apnea is masked. Infants with BPD may also be more prone to obstructive apnea (28,36,37) which we did not measure. Other studies reviewing apnea or bradycardia events documented in the medical record have reported more events in very preterm infants with BPD (19,20).
We did not find a significant difference in number of ABDs in infants with severe IVH though there was a trend toward slightly more ABDs at later PMA. The number of infants with high-grade IVH in our cohort was small, and we did not separately analyze the even smaller fraction of infants with posthemorrhagic hydrocephalus who might have more apnea. Additionally, our methods did not allow us to assess whether infants with IVH had more obstructive apnea as has been reported by others (21). Larger studies would be required to determine whether, as has been reported in a small study, predischarge apnea predicts adverse neurodevelopment at several years of age in preterm infants with severe IVH (9).
Resolution of Apnea
We found, consistent with other reports (18,19,20,23), that infants born at gestations <31 wk had apnea to later PMA than those born less preterm. This reaffirms that a specific PMA (e.g., 36 wk) cannot be used as a “safe” benchmark for low apnea risk without also considering GA. In the spectrum from 23–31 wk GA, however, our data show that the number of ABD events by the time infants reached 35 wk PMA was no longer a function of GA at birth. This is in contrast to findings of other studies (19,20) that relied on medical record documentation of events and therefore probably captured more events that required intervention and were considered clinically important. These studies also included bradycardia or apnea episodes and thus likely included obstructive apnea and vagal bradycardia which we did not measure.
Many infants in our cohort who were otherwise ready for discharge home continued to have short algorithm-detected ABDs. These events may have been self-resolved or occurred during feeding or stressors such as immunization (38), Most infants were sent home without a monitor and very few were readmitted to our hospital within 2 mo for apnea or apparent life-threatening event, which is in keeping with other reports (39). Our unit protocol of discharging infants after a week free of needing stimulation to resolve an apneic spell has not changed based on our studies to date, and further work in larger patient populations is needed to establish criteria for safe NICU discharge, since the cost of additional hospital days simply for an “apnea countdown” is substantial (40).
Conclusion
Apnea events with associated bradycardia and oxygen desaturation occur frequently in hospitalized preterm neonates in spite of respiratory support and caffeine. Further research is needed to determine the long-term impact of these events and identify therapies to minimize apnea burden in the NICU.
Methods
Study Population and Data Collection
We stored and analyzed the bedside monitor waveforms and vital signs of all infants <35 wk gestation in the University of Virginia NICU from January 2009 through March 2014. The study was approved by the UVA Institutional Review Board as requiring no consent, since all data were analyzed retrospectively and could not influence patient care.
Demographic and clinical data, including dates on and off mechanical ventilation and other respiratory support, were obtained from the electronic medical record. Clinical decisions were made by the care team without knowledge of computer algorithm-detected apneas. Caffeine was given based on our unit policy of initiating caffeine for all infants <32 wk GA at birth, and discontinuing caffeine after 32 wk postmenstrual age once the infant was off continuous positive airway pressure and having little or no clinically recognized apnea requiring stimulation. Decisions about dosing and duration of caffeine and readiness for discharge home were based on standard assessment of bedside monitor data, medical record documentation, and nursing reports of apnea events. Generally in our unit during the years of this study, an 8-d period free of apnea requiring stimulation was required prior to discharge (18).
Clinical events and conditions were recorded in a relational clinical database. Severe IVH grade III-IV was identified by serial head ultrasounds. BPD was defined as requirement for supplemental oxygen in our NICU at 36 wk postmenstrual age. Infants who were transferred to an outside hospital on oxygen prior to 36 wk PMA and for whom the subsequent oxygen status was not known were not included in the BPD analysis. Late-onset septicemia was defined as signs of sepsis >3 d from birth, positive blood culture, and antibiotic treatment for at least 5 d. Diagnosis of NEC required abdominal signs with abdominal radiograph showing pneumatosis, portal venous air, or pneumoperitoneum, or requirement for surgery. Cases of NEC with associated septicemia were classified as NEC alone. Severe ROP was defined as requiring laser photoablation or intravitreous bevacizumab therapy.
Data Analysis
Development and validation of the apnea detection system used in this study were previously reported (17). Bedside monitor data were collected using a central network server (BedMaster Ex, Excel Medical, Jupiter, FL), including chest impedance waveforms (60 Hz), electrocardiogram waveforms (three leads at 240 Hz each), and every 2 s oxygen saturation from pulse oximetry signals (using 8 s SpO2 averaging). A computer algorithm was developed to detect episodes of low variance in the chest impedance waveform signal after eliminating heart beat and motion artifact. Temporally associated declines in heart rate to less than 100 bpm and in oxygen saturation to less than 80% were identified. The algorithm identified ABDn events as central apnea of at least n seconds with both bradycardia and desaturation of any duration. For example, ABD10 denotes an episode of cessation of chest movement of 10 or more seconds with associated bradycardia <100 bpm of any duration and desaturation <80% of any duration. The algorithm underwent extensive development, testing, and validation (17).
Statistical Analysis
Continuous variables were analyzed by t-test or ANOVA and categorical variables by Fischer exact test. Receiver operator characteristics curves were constructed, and change in ROC area was analyzed to determine the impact of GA, severe IVH, and BPD on number of ABD events at 35 wk PMA. Number of ABDs in the day prior to septicemia or NEC diagnosis was compared to the prior 1-d baseline for each infant by sign rank test. Statistical significance was considered as two-tailed P < 0.05, and analyses were conducted in MATLAB (MathWorks, Natick, MA)
Statement of Financial Support
This study was supported by the National Institutes of Health (Bethesda, MD, USA) HD072071, HD064488.
Disclosures:
None.
References
Katz-Salamon M. Delayed chemoreceptor responses in infants with apnoea. Arch Dis Child 2004;89:261–6.
Darnall RA. The role of CO(2) and central chemoreception in the control of breathing in the fetus and the neonate. Respir Physiol Neurobiol 2010;173:201–12.
Gauda EB, McLemore GL, Tolosa J, Marston-Nelson J, Kwak D. Maturation of peripheral arterial chemoreceptors in relation to neonatal apnoea. Semin Neonatol 2004;9:181–94.
Poets CF. Apnea of Prematurity. In: Principles and Practice of Pediatric Sleep Medicine: Second Edition. London: Elsevier Saunders, 2012:195–200.
Finer NN, Higgins R, Kattwinkel J, Martin RJ. Summary proceedings from the apnea-of-prematurity group. Pediatrics 2006;117(3 Pt 2):S47–51.
Pillekamp F, Hermann C, Keller T, von Gontard A, Kribs A, Roth B. Factors influencing apnea and bradycardia of prematurity - implications for neurodevelopment. Neonatology 2007;91:155–61.
Janvier A, Khairy M, Kokkotis A, Cormier C, Messmer D, Barrington KJ. Apnea is associated with neurodevelopmental impairment in very low birth weight infants. J Perinatol 2004;24:763–8.
Di Fiore JM, Bloom JN, Orge F, et al. A higher incidence of intermittent hypoxemic episodes is associated with severe retinopathy of prematurity. J Pediatr 2010;157:69–73.
Cheung PY, Barrington KJ, Finer NN, Robertson CM. Early childhood neurodevelopment in very low birth weight infants with predischarge apnea. Pediatr Pulmonol 1999;27:14–20.
Poets CF, Roberts RS, Schmidt B, et al.; Canadian Oxygen Trial Investigators. Association Between Intermittent Hypoxemia or Bradycardia and Late Death or Disability in Extremely Preterm Infants. JAMA 2015;314:595–603.
Gizzi C, Montecchia F, Panetta V, et al. Is synchronised NIPPV more effective than NIPPV and NCPAP in treating apnoea of prematurity (AOP)? A randomised cross-over trial. Arch Dis Child Fetal Neonatal Ed 2015;100:F17–23.
Schmidt B, Roberts RS, Davis P, et al.; Caffeine for Apnea of Prematurity Trial Group. Caffeine therapy for apnea of prematurity. N Engl J Med 2006;354:2112–21.
Butler TJ, Firestone KS, Grow JL, Kantak AD. Standardizing documentation and the clinical approach to apnea of prematurity reduces length of stay, improves staff satisfaction, and decreases hospital cost. Jt Comm J Qual Patient Saf 2014;40:263–9.
Vergales BD, Paget-Brown AO, Lee H, et al. Accurate automated apnea analysis in preterm infants. Am J Perinatol 2014;31:157–62.
Amin SB, Burnell E. Monitoring apnea of prematurity: validity of nursing documentation and bedside cardiorespiratory monitor. Am J Perinatol 2013;30:643–8.
Brockmann PE, Wiechers C, Pantalitschka T, Diebold J, Vagedes J, Poets CF. Under-recognition of alarms in a neonatal intensive care unit. Arch Dis Child Fetal Neonatal Ed 2013;98:F524–7.
Lee H, Rusin CG, Lake DE, et al. A new algorithm for detecting central apnea in neonates. Physiol Meas 2012;33:1–17.
Darnall RA, Kattwinkel J, Nattie C, Robinson M. Margin of safety for discharge after apnea in preterm infants. Pediatrics 1997;100:795–801.
Eichenwald EC, Aina A, Stark AR. Apnea frequently persists beyond term gestation in infants delivered at 24 to 28 weeks. Pediatrics 1997;100(3 Pt 1):354–9.
Lorch SA, Srinivasan L, Escobar GJ. Epidemiology of apnea and bradycardia resolution in premature infants. Pediatrics 2011;128:e366–73.
Butcher-Puech MC, Henderson-Smart DJ, Holley D, Lacey JL, Edwards DA. Relation between apnoea duration and type and neurological status of preterm infants. Arch Dis Child 1985;60:953–8.
Colavita RD, Ment LR. The electrocardiogram in preterm infants with intraventricular hemorrhage and apnea. J Clin Monit 1986;2:1–5.
Hofstetter AO, Legnevall L, Herlenius E, Katz-Salamon M. Cardiorespiratory development in extremely preterm infants: vulnerability to infection and persistence of events beyond term-equivalent age. Acta Paediatr 2008;97:285–92.
Balan KV, Kc P, Hoxha Z, Mayer CA, Wilson CG, Martin RJ. Vagal afferents modulate cytokine-mediated respiratory control at the neonatal medulla oblongata. Respir Physiol Neurobiol 2011;178:458–64.
Hunt CE, Corwin MJ, Baird T, et al.; Collaborative Home Infant Monitoring Evaluation study group. Cardiorespiratory events detected by home memory monitoring and one-year neurodevelopmental outcome. J Pediatr 2004;145:465–71.
Martin RJ, Wang K, Köroğlu O, Di Fiore J, Kc P. Intermittent hypoxic episodes in preterm infants: do they matter? Neonatology 2011;100:303–10.
Saugstad OD, Aune D. Optimal oxygenation of extremely low birth weight infants: a meta-analysis and systematic review of the oxygen saturation target studies. Neonatology 2014;105:55–63.
Esquer C, Claure N, D’Ugard C, Wada Y, Bancalari E. Mechanisms of hypoxemia episodes in spontaneously breathing preterm infants after mechanical ventilation. Neonatology 2008;94:100–4.
Martin RJ, Abu-Shaweesh JM, Baird TM. Pathophysiologic Mechanisms Underlying Apnea of Prematurity. Neoreviews 2002;3:59e–65.
van Zanten HA, Tan RN, Thio M, et al. The risk for hyperoxaemia after apnoea, bradycardia and hypoxaemia in preterm infants. Arch Dis Child Fetal Neonatal Ed 2014;99:F269–73.
Mohr MA, Fairchild KD, Patel M, et al. Quantification of periodic breathing in premature infants. Physiol Meas 2015;36:1415–27.
Herlenius E. An inflammatory pathway to apnea and autonomic dysregulation. Respir Physiol Neurobiol 2011;178:449–57.
Hofstetter AO, Saha S, Siljehav V, Jakobsson PJ, Herlenius E. The induced prostaglandin E2 pathway is a key regulator of the respiratory response to infection and hypoxia in neonates. Proc Natl Acad Sci USA 2007;104:9894–9.
Siljehav V, Hofstetter AM, Leifsdottir K, Herlenius E. Prostaglandin E2 Mediates Cardiorespiratory Disturbances during Infection in Neonates. J Pediatr 2015;167:1207–13.e3.
Poets CF, Stebbens VA, Richard D, Southall DP. Prolonged episodes of hypoxemia in preterm infants undetectable by cardiorespiratory monitors. Pediatrics 1995;95:860–3.
Gerhardt T, Bancalari E. Apnea of prematurity: II. Respiratory reflexes. Pediatrics 1984;74:63–6.
Fajardo C, Alvarez J, Wong A, Kwiatkowski K, Rigatto H. The incidence of obstructive apneas in preterm infants with and without bronchopulmonary dysplasia. Early Hum Dev 1993;32:197–206.
DeMeo SD, Raman SR, Hornik CP, Wilson CC, Clark R, Smith PB. Adverse Events after routine immunization of extremely low-birth-weight infants. JAMA Pediatr 2015;169:740–5.
Subhani M, Katz S, DeCristofaro JD. Prediction of postdischarge complications by predischarge event recordings in infants with apnea of prematurity. J Perinatol 2000;20:92–5.
Zupancic JA, Richardson DK, O’Brien BJ, Eichenwald EC, Weinstein MC. Cost-effectiveness analysis of predischarge monitoring for apnea of prematurity. Pediatrics 2003;111:146–52.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary Figure S1
(TIFF 236 kb)
Supplementary Figure S2
(TIFF 75 kb)
Rights and permissions
About this article
Cite this article
Fairchild, K., Mohr, M., Paget-Brown, A. et al. Clinical associations of immature breathing in preterm infants: part 1—central apnea. Pediatr Res 80, 21–27 (2016). https://doi.org/10.1038/pr.2016.43
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2016.43
This article is cited by
-
Cardiorespiratory signature of neonatal sepsis: development and validation of prediction models in 3 NICUs
Pediatric Research (2023)
-
Artificial and human intelligence for early identification of neonatal sepsis
Pediatric Research (2023)
-
Developmental consequences of short apneas and periodic breathing in preterm infants
Journal of Perinatology (2023)
-
Maturation of cardioventilatory physiological trajectories in extremely preterm infants
Pediatric Research (2023)
-
Vital signs as physiomarkers of neonatal sepsis
Pediatric Research (2022)