Abstract
Background:
PRPS1 encodes isoform I of phosphoribosylpyrophosphate synthetase (PRS-I), a key enzyme in nucleotide biosynthesis. Different missense mutations in PRPS1 cause a variety of disorders that include PRS-I superactivity, nonsyndromic sensorineural hearing impairment, Charcot-Marie-Tooth disease, and Arts syndrome. It has been proposed that each mutation would result in a specific phenotype, depending on its effects on the structure and function of the enzyme.
Methods:
Thirteen Spanish unrelated families segregating X-linked hearing impairment were screened for PRPS1 mutations by Sanger sequencing. In two positive pedigrees, segregation of mutations was studied, and clinical data from affected subjects were compared.
Results:
We report two novel missense mutations in PRPS1, p.Ile275Thr and p.Gly306Glu, which were found in the propositi of two unrelated Spanish families, both subjects presenting with nonsyndromic hearing impairment. Further investigation revealed syndromic features in other hemizygous carriers from one of the pedigrees. Sequencing of genes that are functionally related to PRPS1 did not reveal any candidate variant that might act as a phenotype modifier.
Conclusion:
This case of intrafamilial phenotypic variation associated with a single PRPS1 mutation complicates the genotype–phenotype correlations, which makes genetic counseling of mutation carriers difficult because of the wide spectrum of severity of the associated disorders.
Similar content being viewed by others
Main
Phosphoribosylpyrophosphate synthetase (PRS) is a key enzyme in nucleotide synthesis. It catalyzes the transfer of the terminal pyrophosphoryl group of ATP to ribose 5-phosphate to generate phosphoribosyl pyrophosphate, which is essential in its dual role of substrate and cofactor in different steps of the biosynthetic pathways that generate purine and pyrimidine nucleotides (1). In humans, there are three different PRS isoforms (I, II, and III), which are encoded by PRPS1 (MIM 311850), PRPS2 (MIM 311860), and PRPS3 (also known as PRPS1L1; MIM 611566), respectively.
PRPS1 spans over 30 kb on Xq22.3, contains seven exons, and it is more ubiquitously expressed than the two other genes of the family (1). PRPS1 expression is subject to gene silencing by the miR-376 microRNA, for which the 3′ untranslated region (3′-UTR) of PRPS1 includes two binding sites (2). The PRS-I enzyme is a hexamer that consists of three homodimers, each with an active site (comprising binding sites for ATP and ribose-5-phosphate) and two allosteric sites (3). PRS-I activity requires Mg2+ and it is regulated by allosteric competition between inorganic phosphate (which is an activator) and by purine nucleotides (ADP and GDP, which act as inhibitors) (1,2). In addition, two associated proteins, respectively encoded by PRPSAP1 and PRPSAP2, interact with PRS-I to exert a negative regulatory control on the enzyme’s activity.
Mutations in PRPS1 cause a wide variety of disorders that include: (i) PRS-I superactivity (MIM 300661), which results in purine overproduction causing hyperuricemia and hyperuricosuria with infantile or early childhood onset of gout, and with neurodevelopmental abnormalities, which may include intellectual disability, ataxia, hypotonia, delayed motor development, arreflexia, and/or sensorineural deafness (4,5,6,7,8); (ii) Nonsyndromic sensorineural hearing impairment (DFNX1, formerly DFN2, MIM 304500) of prelingual or postlingual onset (9,10,11,12,13); (iii) Charcot-Marie-Tooth disease-5 (CMTX5, also known as Rosenberg-Chutorian syndrome, MIM311070), which may include ataxia, hypotonia, loss of deep tendon reflexes, early-onset hearing impairment, and optic neuropathy (13,14,15); (iv) Arts syndrome (MIM 301835), which comprises the clinical signs of CMTX5 plus intellectual disability, delayed motor development, and increased susceptibility to infections of the upper respiratory tract, which can lead to an early death (16); and (v) A recently described very severe condition that associates prenatal growth restriction, dysmorphic facial features, short stature, intellectual disability, spastic quadraparesis, seizures, hearing impairment, Leber’s congenital amaurosis, and diabetes insipidus (17).
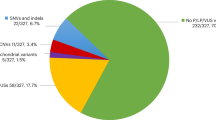
To date, 22 different pathogenic mutations have been reported in the PRPS1 coding region: seven causing PRS-I superactivity (6,7,8), five causing DFNX1 (9,10,11,12,13), five causing CMTX5 (13,14,15), two causing Arts syndrome (16), one causing the recently described very severe syndrome (17), and two causing intermediate phenotypes (one in a patient with PRS-I superactivity and recurrent infections (18), the other in a male subject with an overlap of CMTX5 and Arts syndrome features (19)). Remarkably, all of them are missense mutations. It has been proposed that this variety of phenotypes would correlate with the different effects that the amino acid substitutions exert on the structure of the PRS-I enzyme, depending on the location in the protein and on the biochemical properties of the replacing residue (2).
In this study, we report two novel PRPS1 mutations that were found in the propositi from two unrelated Spanish families, both subjects presenting with nonsyndromic hearing impairment. Further investigation revealed syndromic features in other patients of one of the pedigrees. This case of intrafamilial phenotypic variation is of concern to genetic counseling of subjects with DFNX1 nonsyndromic hearing impairment.
Results
Thirteen Spanish unrelated families with X-linked hearing impairment were selected for this study. In a preliminary step, mutations in the DFNB1 locus (GJB2, encoding connexin-26, and large upstream deletions) (20), which are the most frequent cause of inherited hearing impairment in the Spanish population, were excluded in the propositus of each family. Subsequently, we sequenced the promoter and the seven exons and intron–exon boundaries of PRPS1 (GenBank: NM_002764.3) from each propositus. In two out of them, novel sequence variants were found.
In family S1583, the propositus is the eldest child of nonconsanguineous healthy parents ( Figure 1a ). Pregnancy and delivery were uneventful. At age 14 y, he presented with moderate hearing impairment ( Figure 1b ), which is being treated with hearing aids. No other clinical signs have manifested to date (age 19 y). He has two brothers with normal hearing (ages 17 and 14 y, respectively). His maternal grandfather presented with hearing impairment at age 16 y, and had two affected brothers whose hearing loss manifested also in adulthood. The genetic study revealed a c.824T>C (p.Ile275Thr) mutation in exon 6 of PRPS1 in the propositus (Supplementary Figure S1 online). It was in the heterozygous state in his mother (age 42 y), who had normal hearing ( Figure 1b ), and it was absent in his father and his two healthy brothers. Presence of the mutation in the maternal grandfather and his two affected brothers could not be tested because of unavailability of DNA samples. The mutation was absent in 50 Spanish unrelated control subjects with normal hearing, as well as in 2,535 samples from the 1000-Genomes Project (European Bioinformatics Institute, Hinxton, UK) and in 6,503 samples from the NHLBI Exome Sequencing Project (Washington University, St. Louis, MI). This novel mutation is classified as “disease causing” by the Mutation Taster software, and it affects a residue that is conserved across vertebrates and invertebrates ( Figure 1c ). Molecular modeling of the p.Ile275Thr mutation suggests that it disturbs the local structure of the PRPS1 monomer by destabilizing a hydrophobic pocket and linking two previously unconnected β-strands (Supplementary Figure S2a–c online).
Characterization of two families with novel PRPS1 mutations (a) Pedigrees of Spanish families S1583 and S740, segregating X-linked hearing loss. Blank symbols indicate normal phenotype; shaded symbols indicate different clinical signs, as follows:  nonsyndromic hearing loss;
nonsyndromic hearing loss;  hearing loss, club foot and shortened Achilles tendon;
hearing loss, club foot and shortened Achilles tendon;  hearing loss and seizures;
hearing loss and seizures;  hearing loss, seizures, and intellectual disability. Subjects who were tested for the presence of the mutation in each pedigree are indicated by signs below the symbols, as follows: “+”, hemizygous mutation carrier; “–”, wild type; “±”, heterozygous mutation carrier. (b) Audiograms of subjects from families S1583 and S740. Upper row, an affected male and his normal-hearing mother (family S1583). Lower row, two affected males and a normal-hearing female carrier (family S740). Circles, right ear; crosses, left ear. (c) Alignment of phosphoribosylpyrophosphate synthetase (PRS-I) orthologous sequences from ten model organisms (human, mouse, cattle, grey short tailed opossum, chick, African clawed frog, zebrafish, fruit fly, nematode and yeast; accession numbers on the right of the alignment). Only stretches aligning to human PRS-I residues 263–318 are shown. Asterisks indicate identical residues across all sequences; colons, conserved positions (residues of strongly similar properties); periods, semiconserved positions (residues of weakly similar properties). The locations of mutations p.Ile275Thr and p.Gly306Glu are indicated by vertical arrows.
hearing loss, seizures, and intellectual disability. Subjects who were tested for the presence of the mutation in each pedigree are indicated by signs below the symbols, as follows: “+”, hemizygous mutation carrier; “–”, wild type; “±”, heterozygous mutation carrier. (b) Audiograms of subjects from families S1583 and S740. Upper row, an affected male and his normal-hearing mother (family S1583). Lower row, two affected males and a normal-hearing female carrier (family S740). Circles, right ear; crosses, left ear. (c) Alignment of phosphoribosylpyrophosphate synthetase (PRS-I) orthologous sequences from ten model organisms (human, mouse, cattle, grey short tailed opossum, chick, African clawed frog, zebrafish, fruit fly, nematode and yeast; accession numbers on the right of the alignment). Only stretches aligning to human PRS-I residues 263–318 are shown. Asterisks indicate identical residues across all sequences; colons, conserved positions (residues of strongly similar properties); periods, semiconserved positions (residues of weakly similar properties). The locations of mutations p.Ile275Thr and p.Gly306Glu are indicated by vertical arrows.
In family S740, the propositus (subject V:5, 30 y of age), was referred for genetic study because of a diagnosis of nonsyndromic, prelingual, bilateral hearing impairment. It was a familial case ( Figure 1a ) that included up to nine affected males with prelingual severe to profound hearing impairment ( Figure 1b ). DNA sequencing revealed a novel mutation in the propositus, c.917G>A (p.Gly306Glu), in exon 7 of PRPS1 (Supplementary Figure S1 online). The mutation was absent in 50 Spanish unrelated control subjects with normal hearing, as well as in 2,535 samples from the 1000-Genomes Project, and in 6,503 samples from the NHLBI Exome Sequencing Project. This novel mutation affects a residue that is highly conserved, from yeast to humans ( Figure 1c ), and it is classified as “disease causing” by Mutation Taster. Remarkably, the same residue is affected by another DFNX1-causing mutation, p.Gly306Arg (10). It has been reported that the large side chain of arginine could be accommodated in this mutant PRS-I structure without destabilizing either the allosteric sites or the active site of the enzyme (Supplementary Figure S2 d–f online). Molecular modeling of p.Gly306Glu indicates that the large side chain of the glutamic acid residue can be similarly accommodated. As it occurs with p.Gly306Arg (2), this would affect interactions in the interface of the trimer, and it was expected to result in a DFNX1 phenotype, as in fact it was observed in the propositus.
Search for the mutation in the available samples from other members of family S740 showed that it was present in the propositus’ affected brother (subject V:6, 25 y of age) and, in the heterozygous state, in their normal-hearing mother (IV:4, 49 y of age). Affected male subjects VI:1 (13 y of age at the moment of the study) and VI:2 (6 mo of age) also carried the mutation, and their respective normal-hearing mothers (V:2, age 33 y; and V:4, age 29 y, Figure 1b ) were heterozygotes. Further investigation of the family showed that two of the affected males carrying the mutation (V:6 and VI:1) had additional clinical signs. Neurological evaluation of the four affected males who were available for the study revealed that subject V:6 had mild intellectual disability (IQ test score of 70), global delay in reaching developmental milestones in motor, language and cognitive skills, and complex partial seizures; array Comparative Genomic Hybridization did not reveal any abnormality in this patient. Subject VI:1 had left clubfoot with a shortened Achilles tendon, which was corrected surgically. No clinical sign apart from the hearing impairment was revealed by neurological examination of subjects V:5 and VI:2. Levels of uric acid in blood were normal in all these four affected males, and none of them presented with increased susceptibility to infections. As regards the five male subjects who were not available for mutation testing and neurological evaluation, their relatives reported that four of them (II:3, II:4, IV:12 and V:11) had apparently nonsyndromic hearing impairment, and the other (III:8) had hearing loss and seizures.
Given this intrafamilial phenotypic variability and, specifically, the differences between the two affected brothers V:5 and V:6, we investigated hypothetical modifier effects of genes encoding proteins related to PRS-I: PRPS2 (GenBank: NM_001039091.2), PRPS3 (GenBank: NM_175886.2), PRPSAP1(GenBank: NM_002766.2), and PRPSAP2 (GenBank: NM_002767.3). Sequencing all exons of these four genes, as well as the promoters of PRPS1, PRPS2 and PRPS3, the miR-376 cluster, and the miR-376 target sequences on PRPS1, from subjects V:5 and V:6, did not reveal any mutation that could account for the phenotypic differences.
Discussion
Taking into account the two novel mutations that are described in this study, a total of 24 different pathogenic mutations, all of them of the missense type, have been reported in PRPS1 to date ( Table 1 ). They result in a variety of disorders, so considerable efforts have been made to establish solid genotype–phenotype correlations. According to the current model, the predicted effects of the amino acid substitutions on the protein structure of PRS-I would correlate with the observed phenotypes (2,21).
Mutations affecting the allosteric sites of the enzyme abolish its feedback regulation and result in PRS-I superactivity (4,5,6,7,8,22). They include p.Asp52His and p.Leu129Ile, which directly disturb the local structure near allosteric sites I and II, respectively, and five other mutations that destabilize the homodimer interface, with an indirect effect on allosteric sites, mainly on site II (p.Asn114Ser, p.Ala 190Val, p.Asp183His, p.His193Leu, and p.His193Gln) ( Table 1 ).
Another group of mutations destabilize the ATP binding site and result in CMTX5 (p.Glu43Asp, p.Met115Thr, p.Met115Val, and p.Ala121Gly) (13,14,15), in Arts syndrome (p.Gln133Pro and p.Leu152Pro) (16), or in an intermediate phenotype between CMTX5 and Arts syndrome (p.Gln277Pro) (19) ( Table 1 ). Destabilization of the ATP binding site has been also proposed as the molecular effect of the p.Arg196Trp mutation, which results in one of the most severe forms of PRS-I deficiency (prenatal growth restriction, dysmorphic facial features, short stature, intellectual disability, spastic quadraparesis, seizures, hearing impairment, Leber’s congenital amaurosis, and diabetes insipidus) (17).
Interestingly, a recent report described a novel PRPS1 mutation, p.Val142Leu, which causes an intermediate phenotype of PRS-I superactivity with the recurrent infections that are a feature of Arts syndrome (18). It has been proposed that this mutation would affect simultaneously the ATP binding site and both allosteric sites of PRS-I, so resulting in a enzyme that would have partially lost its activity, but also its allosteric regulation.
Finally, the last group of mutations exert their effects by disturbing the local structure (p.Ala87Thr and p.Ile290Thr) or by affecting interactions in the interface of the trimer (p.Asp65Asn, p.Ala113Ser, and p.Gly306Arg), but not destabilizing either the allosteric sites or the active site. These mutations result in DFNX1 nonsyndromic hearing impairment (9,10,11,12,13) ( Table 1 ). The novel mutation p.Ile275Thr, which was found in this study, would belong to this last group, according to its molecular modeling, which predicts a disturbance of the local structure, and according to the resulting DFNX1 phenotype.
The other mutation that was found in this study, p.Gly306Glu, affects the same amino acid as the DFNX1-causing p.Gly306Arg mutation, which suggests that the Gly306 residue is especially important for the function of PRS-I. Both substitutions replace a glycine by residues having much larger and charged side chains (positive charge in arginine, negative in glutamic acid), but they can be accommodated with no local structural effect, although affecting interactions in the interface of the trimer, where Gly-306 must play an important role, given the high conservation of this residue and that it might be a mutation hotspot. This would lead to a DFNX1 phenotype. However, an unexpected intrafamilial phenotypic variation was observed in males of family S740 who carried the p.Gly306Glu mutation. Six affected males had apparently non-syndromic hearing loss. This was confirmed in two of them, V:5 and VI:2, by neurological examination, although VI:2 is just 6 mo old and so it cannot be formally excluded that he may develop additional signs later in life. In contrast, three other males had hearing impairment and additional clinical signs: seizures (two subjects), mild intellectual disability and developmental delay (one subject), and a shortened Achilles tendon (one subject). The association of these signs in patients could occur just coincidentally, each having a different genetic cause, but they manifest just in male mutation carriers, and not in other members of this large family. On the other hand, these signs have been reported in Arts syndrome, which suggests that they could result from the p.Gly306Glu mutation in PRPS1. Interestingly, in a former study, one of the five DFNX1-affected males carrying the p.Gly306Arg mutation was shown to have mild nonprogressive choreiform tremors of the upper extremities (10). These data suggest that mutations affecting residue Gly306 would result in a loose phenotype that predominantly consists of nonsyndromic hearing loss but that can also include syndromic features in some patients. At this moment, we cannot propose a mechanism for this intrafamilial variability, since mutations in the different candidate modifier genes that we investigated were excluded in family S740.
Conclusion
Mutations in PRPS1 result in a great variety of disorders ranging from nonsyndromic hearing impairment to very complex and severe clinical conditions, which include an expanding spectrum of clinical signs (16). The finding of intermediate phenotypes between the different well-defined clinical entities (17,18) indicates that mutations in PRPS1 have the potential of producing a continuum of clinical features, whose combinations are sometimes difficult to classify. Molecular modeling of the different mutations predicts their effects on the structure of the PRS-I enzyme, and so it provides a first molecular basis for an explanation of the resulting phenotypes. In addition, for loss-of-function mutations, the levels of the residual enzyme activity seem to correlate with the severity of the disease. However, intrafamilial phenotypic variability adds more complexity to the picture, suggesting the existence of other modifiers of the phenotype. Consequently, no diagnosis of DFNX1 nonsyndromic hearing impairment can be firmly established without clear exclusion of syndromic features by thorough clinical (mainly neurological) examinations. Furthermore, genetic counseling of subjects from DFNX1-diagnosed families must take into account the possibility that other clinical signs may accompany hearing loss in their descendants carrying a PRPS1 mutation.
Methods
Thirteen unrelated Spanish families segregating X-linked hearing impairment were enrolled in this study. After approval by the Ethical Committee of Hospital Universitario Ramón y Cajal (in accordance with the 1964 Declaration of Helsinki), written informed consent was obtained from all participating subjects. Hearing was evaluated by pure-tone audiometry, testing for air conduction (frequencies 125–8,000 Hz), and bone conduction (frequencies 250–4,000 Hz). The hearing status of infants was investigated by recording Auditory-evoked Brainstem Responses (ABRs). The degree of hearing loss was determined by calculating the binaural mean of the hearing thresholds for air conduction at frequencies 0.5, 1, and 2 kHz, and it was classified as mild (average thresholds in the range of 21–40 dB), moderate (41–70 dB), severe (71–90 dB), or profound (>90 dB).
DNA was extracted from peripheral blood samples by using the Chemagic MSM I automated system (Chemagen, Baesweiler, Germany). Screening of mutations in GJB2 and large upstream deletions was performed as previously reported (20). Primers were designed for PCR amplification and Sanger DNA sequencing of all exons and exon-intron boundaries of PRPS1, PRPS2, PRPS3, PRPSAP1, and PRPSAP2, as well as the promoters of PRPS1, PRPS2 and PRPS3, the miR-376 cluster, and the miR-376 target sequences on PRPS1 (Supplementary Table S1 online).
Mutation nomenclature is based on cDNA sequence (GenBank accession number NM_002764.3) and follows current Human Genome Variation Society rules as implemented by the Mutalyzer 2.0.3 program (Leiden University Medical Center, Leiden, The Netherlands). The pathogenic potential of the novel missense mutations was evaluated by using the Mutation Taster software (Universitätsmedizin Berlin, Berlin, Germany). Three-dimensional modeling of the novel mutations was based on hexamer model 2h06.pdb1 (23). The altered amino acid side chains in the model were positioned with a backbone-dependent rotamer library, as implemented in the Swiss-Prot PDB Viewer 4.1 program (Biozentrum, Basel, Switzerland) (24).
Statement of Financial Support
This research was supported by grants from Instituto de Salud Carlos III, Madrid, Spain (FIS PI11/00612, National Plan I+D+I 2008–2011, with co-funding from the European Regional Development Fund) and Fundación Ramón Areces, Madrid, Spain.
Disclosure
The authors declare that they have no conflict of interest.
References
Duley JA, Christodoulou J, de Brouwer AP. The PRPP synthetase spectrum: what does it demonstrate about nucleotide syndromes? Nucleosides Nucleotides Nucleic Acids 2011;30:1129–39.
de Brouwer AP, van Bokhoven H, Nabuurs SB, Arts WF, Christodoulou J, Duley J. PRPS1 mutations: four distinct syndromes and potential treatment. Am J Hum Genet 2010;86:506–18.
Tang W, Li X, Zhu Z, et al. Expression, purification, crystallization, and preliminary X-ray diffraction analysis of human phosphoribosyl pyrophosphate synthetase 1 (PRS1). Acta Crystallogr SectF Struct Biol Cryst Commun 2006; 62 (Pt 5):432–4.
Becker MA, Raivio KO, Bakay B, Adams WB, Nyhan WL. Variant human phosphoribosylpyrophosphate synthetase altered in regulatory and catalytic functions. J Clin Invest 1980;65:109–20.
Becker MA, Losman MJ, Wilson J, Simmonds HA. Superactivity of human phosphoribosyl pyrophosphate synthetase due to altered regulation by nucleotide inhibitors and inorganic phosphate. Biochim Biophys Acta 1986;882:168–76.
Roessler BJ, Nosal JM, Smith PR, et al. Human X-linked phosphoribosylpyrophosphate synthetase superactivity is associated with distinct point mutations in the PRPS1 gene. J Biol Chem 1993;268:26476–81.
Becker MA, Smith PR, Taylor W, Mustafi R, Switzer RL. The genetic and functional basis of purine nucleotide feedback-resistant phosphoribosylpyrophosphate synthetase superactivity. J Clin Invest 1995;96:2133–41.
García-Pavía P, Torres RJ, Rivero M, Ahmed M, García-Puig J, Becker MA. Phosphoribosylpyrophosphate synthetase overactivity as a cause of uric acid overproduction in a young woman. Arthritis Rheum 2003;48:2036–41.
Tyson J, Bellman S, Newton V, et al. Mapping of DFN2 to Xq22. Hum Mol Genet 1996;5:2055–60.
Manolis EN, Eavey RD, Sangwatanaroj S, et al. Hereditary postlingual sensorineural hearing loss mapping to chromosome Xq21. Am J Otol 1999;20:621–6.
Cui B, Zhang H, Lu Y, et al. Refinement of the locus for non-syndromic sensorineural deafness (DFN2). J Genet 2004;83:35–8.
Liu X, Han D, Li J, et al. Loss-of-function mutations in the PRPS1 gene cause a type of nonsyndromic X-linked sensorineural deafness, DFN2. Am J Hum Genet 2010;86:65–71.
Robusto M, Fang M, Asselta R, et al. The expanding spectrum of PRPS1-associated phenotypes: three novel mutations segregating with X-linked hearing loss and mild peripheral neuropathy. Eur J Hum Genet in press, doi: 10.1038/ejhg.2014.168.
Kim HJ, Sohn KM, Shy ME, et al. Mutations in PRPS1, which encodes the phosphoribosyl pyrophosphate synthetase enzyme critical for nucleotide biosynthesis, cause hereditary peripheral neuropathy with hearing loss and optic neuropathy (cmtx5). Am J Hum Genet 2007;81:552–8.
Park J, Hyun YS, Kim YJ, et al. Exome Sequencing Reveals a Novel PRPS1 Mutation in a Family with CMTX5 without Optic Atrophy. J Clin Neurol 2013;9:283–8.
de Brouwer AP, Williams KL, Duley JA, et al. Arts syndrome is caused by loss-of-function mutations in PRPS1. Am J Hum Genet 2007;81:507–18.
Al-Maawali A, Dupuis L, Blaser S, et al. Prenatal growth restriction, retinal dystrophy, diabetes insipidus and white matter disease: expanding the spectrum of PRPS1-related disorders. Eur J Hum Genet 2015;23:310–6.
Moran R, Kuilenburg AB, Duley J, et al. Phosphoribosylpyrophosphate synthetase superactivity and recurrent infections is caused by a p.Val142Leu mutation in PRS-I. Am J Med Genet A 2012;158A:455–60.
Synofzik M, Müller vom Hagen J, Haack TB, et al. X-linked Charcot-Marie-Tooth disease, Arts syndrome, and prelingual non-syndromic deafness form a disease continuum: evidence from a family with a novel PRPS1 mutation. Orphanet J Rare Dis 2014;9:24.
del Castillo FJ, Rodríguez-Ballesteros M, Alvarez A, et al. A novel deletion involving the connexin-30 gene, del(GJB6-d13s1854), found in trans with mutations in the GJB2 gene (connexin-26) in subjects with DFNB1 non-syndromic hearing impairment. J Med Genet 2005;42:588–94.
Liu XZ, Xie D, Yuan HJ, de Brouwer AP, Christodoulou J, Yan D. Hearing loss and PRPS1 mutations: Wide spectrum of phenotypes and potential therapy. Int J Audiol 2013;52:23–8.
Chen P, Li J, Ma J, Teng M, Li X. A small disturbance, but a serious disease: the possible mechanism of D52H-mutant of human PRS1 that causes gout. IUBMB Life 2013;65:518–25.
Li S, Lu Y, Peng B, Ding J. Crystal structure of human phosphoribosylpyrophosphate synthetase 1 reveals a novel allosteric site. Biochem J 2007;401:39–47.
Guex N, Peitsch MC. SWISS-MODEL and the Swiss-PdbViewer: an environment for comparative protein modeling. Electrophoresis 1997;18:2714–23.
Acknowledgements
We thank the patients and their relatives for their kind cooperation in this study.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary Figure S1
(TIFF 6851 kb)
Supplementary Figure S2
(JPEG 9527 kb)
Supplementary Table S1
(DOC 88 kb)
PowerPoint slides
Rights and permissions
About this article
Cite this article
Gandía, M., Fernández-Toral, J., Solanellas, J. et al. Mutations in PRPS1 causing syndromic or nonsyndromic hearing impairment: intrafamilial phenotypic variation complicates genetic counseling. Pediatr Res 78, 97–102 (2015). https://doi.org/10.1038/pr.2015.56
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2015.56
This article is cited by
-
A novel mutation in gene of PRPS1 in a young Chinese woman with X-linked gout: a case report and review of the literature
Clinical Rheumatology (2020)
-
Genetic Testing for Deaf and Hard of Hearing Individuals: Genetic Counseling
Current Genetic Medicine Reports (2016)