Abstract
Background:
Uridine diphosphoglucuronate-glucuronosyltransferase 1A1 (UGT1A1) gene mutation was shown to be responsible for neonatal hyperbilirubinemia. This study aimed to investigate whether UGT1A1 gene mutation is associated with neonatal hyperbilirubinemia in Guangxi Heiyi Zhuang and Han populations.
Methods:
Two hundred and eighteen infants with hyperbilirubinemia (118 Heiyi Zhuang, 100 Han) and 190 control subjects (110 Heiyi Zhuang, 80 Han) were enrolled. Polymerase chain reaction and gene sequencing were used to detect the TATA-box and exon 1 of UGT1A1.
Results:
(TA)7 insertion mutation, 211G>A (G71R), 686C>A (P229Q), and 189C>T (D63D) were detected. Logistic regression analysis showed odds ratios (OR) of 2.64 (95% confidence interval (CI) 1.64–4.24; P < 0.001) and 0.69 (95%CI 0.43–1.10; P = 0.115) for neonates who carried UGT1A1 G71R and (TA)7 insertion mutation, respectively. G71R homozygosity increased the odds of dangerous bilirubin levels by a factor 34.23, and G71R heterozygosity only by 2.10.
Conclusion:
We found that UGT1A1 G71R mutation is a risk factor for neonatal hyperbilirubinemia in Guangxi Heiyi Zhuang and Han populations. Meanwhile, the UGT1A1 (TA)7 insertion mutation is not associated with neonatal hyperbilirubinemia in the two ethnic groups.
Similar content being viewed by others
Main
Neonatal hyperbilirubinemia is a common symptom in the neonatal period, with a complex pathogenesis. Recently, UGT1A1 gene mutations have been considered a risk factor for this ailment.
UGT1A1 is a key enzyme in the metabolism of bilirubin (1), and is encoded by the UGT1A1 gene. Ritter et al. (2) first discovered that UGT1A1 gene product shows glucuronosyltransferase activity. UGT1A1 is located at chromosome 2q37 (3), and includes five exons (exons 1–5). The promoter region is close to the upstream of the transcription start site of exon 1, including the TATA-box. Mutations of the UGT1A1 gene may cause decreased or abolished enzyme activity, leading to neonatal hyperbilirubinemia (4).
More than 100 types of UGT1A1 gene mutations have been identified so far. The mutational hotspots are mainly located in the promoter region and exon1 of UGT1A1 (5). According to the previous studies, UGT1A1 gene mutations and its relation to neonatal hyperbilirubinemia may differ among areas and ethnic groups. The (TA)7 insertion in the UGT1A1 promoter is the most common mutation in Caucasians, and appears to cause Gilbert’s syndrome (6,7). Meanwhile, the G71R substitution in exon 1 of the UGT1A1 gene is the most common mutation type described as a risk factor for neonatal hyperbilirubinemia in Asians (8,9).
There is a high incidence of neonatal hyperbilirubinemia in the Guangxi area, which is also a multiethnic region. Han is the largest ethnic group there, followed by Zhuang. Heiyi Zhuang is a major branch of the Zhuang ethnic group, and comprises people mainly living in Napo County, Guangxi, China. We hypothesized that UGT1A1 gene mutations may be related to neonatal hyperbilirubinemia in Guangxi Heiyi Zhuang and Han populations. So, we performed this study to test this hypothesis.
Results
Demographic Factors
Demographic characteristics of the cases and controls are shown in Table 1 . No differences between the two groups were found in gestational age, birth weight, gender, feeding pattern, and population.
UGT1A1 Polymorphisms
The following variations were observed in the promoter TATA-box: A(TA)6TAA/A(TA)6TAA, (TA)6/6; A(TA)6TAA/A(TA)7TAA, (TA)6/7; A(TA)7TAA/A(TA)7TAA, (TA)7/7. Other variations were at nucleotides 211 (G>A, heterozygous and homozygous) and 686 (C>A, heterozygous), in addition to a SNP (rs191471887, 189C>T, heterozygous) in the exon 1 of the UGT1A1 gene.
As shown in Table 2 , 211G>A was the most common mutation in this study. The incidence rates of homozygous variation (A/A), heterozygous variation (G/A), and wild type (G/G) at nucleotide 211 were 3.7, 27.1, and 66.1%, respectively, in the case group, and 0, 16.3, and 83.7%, respectively, in the control group. Meanwhile, (TA)7 insertion mutation was the second common mutation. The incidence rates of homozygous variation ((TA)7/7), heterozygous variation ((TA)6/7), and wild type ((TA)6/6) in the promoter TATA-box were 1.8, 17.4, and 80.7%, respectively, in the case group, and 0.5, 25.2, and 74.2%, respectively, in the control group.
Only one 686C>A (P229Q) heterozygous carrier and two 189C>T (rs191471887) heterozygous carriers were identified in the Han ethnic group. Therefore, statistical analysis was not possible.
Risk Factor of Neonatal Hyperbilirubinemia
Logistic regression analysis ( Table 2 ) showed that the genotypic distribution of UGT1A1 211G>A (G71R) differed significantly between the case and control groups. In addition, 211G>A homozygosity and heterozygosity were both significantly associated with neonatal hyperbilirubinemia. Moreover, the ORs of developing hyperbilirubinemia were even higher in neonates harboring homozygous 211G>A (34.23) compared with their heterozygous counterparts (2.10).
However, the distribution of (TA)7 insertion mutations was not significantly different between the two groups. In addition, no association was found between (TA)7 insertion mutation and neonatal hyperbilirubinemia, either in (TA)7/7 homozygous or (TA)6/7 heterozygous individuals.
Furthermore, breastfeeding was not a significant independent risk factor for neonatal hyperbilirubinemia in Guangxi Heiyi Zhuang and Han populations (OR = 0.65; 95% CI 0.41–1.01; P = 0.079).
Discussion
The exact pathogenesis of neonatal hyperbilirubinemia is not yet clear. Except for other possible risk factors such as congenital malformations, G6PD deficiency, ABO incompatibility, and low birth weight, UGT1A1 gene mutations were found to be closely implicated (10,11,12). This study examined the association of UGT1A1 gene mutations and hyperbilirubinemia in two ethnic subpopulations of China. For the 211G>A genotype, a strong association was found, with estimated ORs of 34 and 2.10 obtained in homozygous and heterozygous individuals, respectively. No association was found for the (TA)7 genotype, and our data indicated that breastfeeding is not an independent risk factor for neonatal hyperbilirubinemia.
The reported mutation types of the UGT1A1 gene include insertion, deletion, missense, nonsense, and synonymous mutations (12). In this study, (TA)7 insertion, 211G>A (G71R) and 686C>A (P229Q) missense, and the synonymous 189C>T mutations were detected; no nonsense mutation was found.
Among the four mutations, 211G>A was the most common as shown above, and resulted in a change of glycine to arginine at position 71 (G71R). The A allele frequency in the case group was 20.4%, which is higher than data from Turkish (4.3%) (13) and North India (0%) (14), but lower than values in Korean (32%) (15) and Japan (34%) (16), and close to our previous study (23.3%) (17). The frequency of the 211G>A mutation was significantly higher in hyperbilirubinemia infants than controls in this study, indicating its close relationship to neonatal hyperbilirubinemia in Guangxi Heiyi Zhuang and Han populations. The same conclusion was reached in most Asian countries such as Korea (15), Japan (16), and other regions of China (18). However, different findings have been reported in Caucasians and Africans (6). Studies in Turkey (19) and the United States (20) found no significant association between 211G>A and neonatal hyperbilirubinemia. In addition, the risk for neonatal hyperbilirubinemia in individuals carrying homozygous 211G>A was higher than in their heterozygous counterparts in this study. Our previous study showed that G71R homozygous subjects have higher incidence of bilirubin encephalopathy compared with wild-type and heterozygous individuals (17). Therefore, more attention should be paid to homozygous 211G>A subjects.
(TA)7 insertion mutations are common in Caucasians and Africans but rare in East Asians (8,21,22,23). Although (TA)7 insertion mutation was the second common mutation in this study, (TA)7/7 homozygous individuals were rare as well. In addition, logistic regression analysis showed that (TA)7 insertion mutation alone is not a risk factor for neonatal hyperbilirubinemia in Guangxi Heiyi Zhuang and Han populations. This corroborated other findings in most of the Asians (9,23). However, discrepant conclusions were reached for Caucasians. Indeed, (TA)7 insertion is the most common mutation causing Gilbert syndrome in Caucasians (6,7), and multiple studies have revealed its relationship with neonatal hyperbilirubinemia in Caucasians (14,24,25,26,27,28,29,30). Roy-Chowdhury et al. (24) reported that the (TA)7 allele may be associated with high TSB levels. Agrawal et al. (14) reported that (TA)n promoter variations are significantly associated with neonatal hyperbilirubinemia in North India. However, the majority of studies assessing Caucasians, including two recent ones, have shown that (TA)7 insertion alone does not necessarily cause neonatal hyperbilirubinemia (20,25,26,27), in agreement with Asian studies. But it increases the risk for hyperbilirubinemia when the neonates also have G6PD deficiency, are breastfed, or have concomitant ABO incompatibility (20,28,29,30).
Previous studies have suggested breastfeeding as a significant risk factor for hyperbilirubinemia (29,31). The possible explanation is that breast milk contains β-glucuronidase, which increases the entero-hepatic circulation and inhibits the hepatic excretion of bilirubin (32). Unlike the studies mentioned above, we did not find any contributory role of breastfeeding in neonatal hyperbilirubinemia, as breastfeeding was universally present in both the case and control groups, in agreement with a previous report (11).
In conclusion, our results showed that UGT1A1 G71R mutation is a strong risk factor for neonatal hyperbilirubinemia in Guangxi Heiyi Zhuang and Han populations. Meanwhile, (TA)7 insertion mutation is not associated with neonatal hyperbilirubinemia in Guangxi Heiyi Zhuang and Han populations. Therefore, a large sample investigation is warranted to confirm our findings.
Methods
Study Subjects
The case-control study method was applied. A total of 408 subjects were included, all full-term newborns who were born in The First Affiliated Hospital of Guangxi Medical University and People’s Hospital of Napo, between June 2012 and October 2013. They were 2–14 d old, with birth weights of 2.5–4.0 kg. The diagnostic standard of neonatal hyperbilirubinemia was done following the 2004 American Academy of Pediatrics guidelines (33). The case group included 218 neonates (118 of Heiyi Zhuang origin, 100 of Han origin) with unexplained hyperbilirubinemia (total serum bilirubin level above the 95th percentile of Bhutani nomogram (33). The neonates had no known risk factors for neonatal hyperbilirubinemia (such as congenital malformations, glucose-6- phosphate dehydrogenase(G6PD) deficiency, ABO incompatibility, small size for gestational age, asphyxia, cephalohematoma, infection, abnormal liver function, polycythemia, low blood sugar and the mother with pregnancy-induced hypertension, anemia, and/or diabetes during pregnancy). The control group comprised 190 neonates (110 of Heiyi Zhuang origin and 80 of Han origin) without hyperbilirubinemia (total serum bilirubin level below the 40th percentile of Bhutani nomogram (33).
The study was approved by the Institutional Review Board and ethics committee of The First Affiliated Hospital of Guangxi Medical University and People’s Hospital of Napo. Signed informed consent forms were obtained from the parents of all infants.
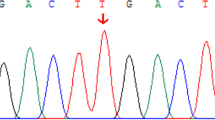
Genotyping
Peripheral blood samples were collected in tubes containing ethylene diamine tetraacetic acid (EDTA). Genomic DNA was extracted using the BloodGen Mini Kit (CWBIO, Beijing, China). The promoter TATA-box and exon 1 of the UGT1A1 gene were amplified by polymerase chain reaction (PCR), using previously described primers (34,35). The PCR mixture (50 µl) was consisted of 2 µl of DNA(≥100 ng/µl); 1 µl of each primer; 25 µl of 2× Taq Master Mix (CWBIO) containing 0.3 U Taq DNA Polymerase, 2× Taq PCR Buffer, 3 mmol/l MgCl2, and 400 µmol/l dNTP mix; 21 µl of deionized water. Fragment 1 was amplified under the following conditions: predenaturation at 95 °C for 5 min; 35 cycles of denaturation at 95 °C for 60 s, annealing at 60 °C for 60 s, extension at 72 °C for 60 s; final extension at 72 °C for 5 min. Fragment 2 was amplified as follows: predenaturation at 94 °C for 2 min; 30 cycles of denaturation at 94 °C for 15 s, annealing at 62 °C for 30 s, extension at 68 °C for 30 s; final extension at 68 °C for 5 min. The PCR products were analyzed by 2% Agarose gel (DOC2000, Bio-Rad laboratories, Hercules, CA) electrophoresis.
Statistical Analysis
The SPSS software (revision 17.0, SPSS, Chicago, IL) was used for statistical analysis. Data were expressed as medians (5–95 percentiles) for continuous variables. T-test was used to compare continuous variables while chi-squared test (χ2) was utilized to compare categorical variables between the case and control groups. Logistic regression analysis was performed to identify the risk factors for neonatal hyperbilirubinemia in Heiyi Zhuang and Han ethnic groups. A P value of less than 0.05 or a 95% CI for OR ≥ 1.0 was considered statistically significant.
Statement of Financial Support
This study was supported by the National Natural Science Foundation of China (Grant 81060055).
Disclosures:
None of the authors have competing financial interests.
References
Tukey RH, Strassburg CP. Human UDP-glucuronosyltransferases: metabolism, expression, and disease. Annu Rev Pharmacol Toxicol 2000;40:581–616.
Ritter JK, Crawford JM, Owens IS. Cloning of two human liver bilirubin UDP-glucuronosyltransferase cDNAs with expression in COS-1 cells. J Biol Chem 1991;266:1043–7.
Watchko JF, Daood MJ, Biniwale M. Understanding neonatal hyperbilirubinaemia in the era of genomics. Semin Neonatol 2002;7:143–52.
Kaplan M, Hammerman C, Maisels MJ. Bilirubin genetics for the nongeneticist: hereditary defects of neonatal bilirubin conjugation. Pediatrics 2003;111(4 Pt 1):886–93.
Canu G, Minucci A, Zuppi C, Capoluongo E. Gilbert and Crigler Najjar syndromes: an update of the UDP-glucuronosyltransferase 1A1 (UGT1A1) gene mutation database. Blood Cells Mol Dis 2013;50:273–80.
Bosma PJ, Chowdhury JR, Bakker C, et al. The genetic basis of the reduced expression of bilirubin UDP-glucuronosyltransferase 1 in Gilbert’s syndrome. N Engl J Med 1995;333:1171–5.
Sato H, Adachi Y, Koiwai O. The genetic basis of Gilbert’s syndrome. Lancet 1996;347:557–8.
Akaba K, Kimura T, Sasaki A, et al. Neonatal hyperbilirubinemia and mutation of the bilirubin uridine diphosphate-glucuronosyltransferase gene: a common missense mutation among Japanese, Koreans and Chinese. Biochem Mol Biol Int 1998;46:21–6.
Long J, Zhang S, Fang X, Luo Y, Liu J. Association of neonatal hyperbilirubinemia with uridine diphosphate-glucuronosyltransferase 1A1 gene polymorphisms: meta-analysis. Pediatr Int 2011;53:530–40.
Huang MJ, Kua KE, Teng HC, Tang KS, Weng HW, Huang CS. Risk factors for severe hyperbilirubinemia in neonates. Pediatr Res 2004;56:682–9.
Tiwari PK, Bhutada A, Agarwal R, Basu S, Raman R, Kumar A. UGT1A1 gene variants and clinical risk factors modulate hyperbilirubinemia risk in newborns. J Perinatol 2014;34:120–4.
Skierka JM, Kotzer KE, Lagerstedt SA, O’Kane DJ, Baudhuin LM. UGT1A1 genetic analysis as a diagnostic aid for individuals with unconjugated hyperbilirubinemia. J Pediatr 2013;162:1146–52, 1152.e1–2.
Kilic I, Koseler A, Cakaloz I, Atalay E. Screening for G71R mutation of the UDP-glucuronosyltransferase 1 (UGT1A1) gene in neonates with pathologic and prolonged hyperbilirubinemia in Turkey. Int J Clin Pharmacol Ther 2010;48:504–8.
Agrawal SK, Kumar P, Rathi R, et al. UGT1A1 gene polymorphisms in North Indian neonates presenting with unconjugated hyperbilirubinemia. Pediatr Res 2009;65:675–80.
Kang H, Lim JH, Kim JS, et al. The association of neonatal hyperbilirubinemia with UGT1A1 and CYP1A2 gene polymorphism in Korean neonates. Korean J Pediatr 2005;48:380–6.
Maruo Y, Nishizawa K, Sato H, Doida Y, Shimada M. Association of neonatal hyperbilirubinemia with bilirubin UDP-glucuronosyltransferase polymorphism. Pediatrics 1999;103(6 Pt 1):1224–7.
Gao ZY, Zhong DN, Liu Y, Liu YN, Wei LM. [Roles of UGT 1A1 gene mutation in the development of neonatal hyperbilirubinemia in Guangxi]. Zhonghua Er Ke Za Zhi 2010;48:646–9.
Long J, Zhang S, Fang X, Luo Y, Liu J. Neonatal hyperbilirubinemia and Gly71Arg mutation of UGT1A1 gene: a Chinese case-control study followed by systematic review of existing evidence. Acta Paediatr 2011;100:966–71.
Narter F, Can G, Ergen A, Isbir T, Ince Z, Çoban A. Neonatal hyperbilirubinemia and G71R mutation of the UGT1A1 gene in Turkish patients. J Matern Fetal Neonatal Med 2011;24:313–6.
Watchko JF, Lin Z, Clark RH, Kelleher AS, Walker MW, Spitzer AR ; Pediatrix Hyperbilirubinemia Study Group. Complex multifactorial nature of significant hyperbilirubinemia in neonates. Pediatrics 2009;124:e868–77.
Nikolac N, Simundic AM, Topic E, et al. Rare TA repeats in promoter TATA box of the UDP glucuronosyltranferase (UGT1A1) gene in Croatian subjects. Clin Chem Lab Med 2008;46:174–8.
Jeon JD, Jo HS, Lee SG, et al. UDP-glucuronosyltransferase 1A1 gene polymorphism in severe neonatal hyperbilirubinemia. J Korean Soc Neonatol 2007;14:46–52.
Waku S, Takeshima Y, Nakamura H, Nishio H, Sumino K. A variant TATA box in the bilirubin UDP-glucuronosyltransferase 1 gene promoter does not contribute to neonatal jaundice in the Japanese population. Arch Dis Child Fetal Neonatal Ed 1999;81:F159.
Roy-Chowdhury N, Deocharan B, Bejjanki HR, et al. Presence of the genetic marker for Gilbert syndrome is associated with increased level and duration of neonatal jaundice. Acta Paediatr 2002;91:100–1.
Carvalho CG, Castro SM, Santin AP, de Azevedo LA, Pereira ML, Giugliani R. Polymorphic variants of UGT1A1 in neonatal jaundice in southern Brazil. J Trop Pediatr 2010;56:366–7.
Travan L, Lega S, Crovella S, Montico M, Panontin E, Demarini S. Severe neonatal hyperbilirubinemia and UGT1A1 promoter polymorphism. J Pediatr 2014;165:42–5.
Petersen JP, Henriksen TB, Hollegaard MV, et al. Extreme neonatal hyperbilirubinemia and a specific genotype: a population-based case-control study. Pediatrics 2014;134:510–5.
Kaplan M, Renbaum P, Levy-Lahad E, Hammerman C, Lahad A, Beutler E. Gilbert syndrome and glucose-6-phosphate dehydrogenase deficiency: a dose-dependent genetic interaction crucial to neonatal hyperbilirubinemia. Proc Natl Acad Sci USA 1997;94:12128–32.
Chang PF, Lin YC, Liu K, Yeh SJ, Ni YH. Risk of hyperbilirubinemia in breast-fed infants. J Pediatr 2011;159:561–5.
Kaplan M, Hammerman C, Renbaum P, Klein G, Levy-Lahad E. Gilbert’s syndrome and hyperbilirubinaemia in ABO-incompatible neonates. Lancet 2000;356:652–3.
Itoh S, Kondo M, Kusaka T, Isobe K, Onishi S. Differences in transcutaneous bilirubin readings in Japanese term infants according to feeding method. Pediatr Int 2001;43:12–5.
Gourley GR. Breast-feeding, neonatal jaundice and kernicterus. Semin Neonatol 2002;7:135–41.
Maisels MJ, Baltz RD, Bhutani VK, et al. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 2004;114:297–316.
Chen QR, Sun SC, Peng YS, Wang Q. Polymorphism of A(TA)nTATAA in promoter region of UGT1A1 gene and its correlation with serum bilirubin. J Diagn Concepts Pract 2012;11:149–52.
Shen J, Wu JX, Li DG. Genetic analysis of UGT1A1 gene in a Chinese family with Gilbert syndrome. Chin J Gastroenterol 2007;12:392–96.
Acknowledgements
We thank People’s Hospital of Napo for providing the subjects.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, XJ., Zhong, DN., Xie, XZ. et al. UGT1A1 gene mutations and neonatal hyperbilirubinemia in Guangxi Heiyi Zhuang and Han populations. Pediatr Res 78, 585–588 (2015). https://doi.org/10.1038/pr.2015.134
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2015.134
This article is cited by
-
Normalizing hyperactivity of the Gunn rat with bilirubin-induced neurological disorders via ketanserin
Pediatric Research (2022)
-
The relationship between hyperbilirubinemia and the promoter region and first exon of UGT1A1 gene polymorphisms in Vietnamese newborns
Pediatric Research (2020)
-
Correlation between UGT1A1 polymorphism and neonatal hyperbilirubinemia of neonates in Wuhan
Current Medical Science (2017)