Abstract
Background:
B-type natriuretic peptide (BNP) has not been evaluated in newborns with congenital diaphragmatic hernia (CDH). We hypothesized that BNP and severity of pulmonary hypertension (PH) would predict clinical outcome in these infants.
Methods:
We measured BNP levels and assessed severity of PH by echocardiography at 1 d and 1 wk of life. Outcome was classified by status at 56 d (or prior discharge): Good (n = 13) if alive on room air and Poor (n = 14) if expired or receiving respiratory support. We estimated area under the curve (AUC) and 95% confidence interval (CI).
Results:
BNP levels were higher at 1 d in newborns with Poor outcome (median 220 pg/ml vs. 55 pg/ml, P < 0.01). At 1 wk, there was no significant difference in BNP level (median 547 pg/ml vs. 364 pg/ml, P = 0.70, for Poor and Good outcomes). At 1 d, BNP level predicted outcome (AUC = 0.91, 95% CI = 0.77–1.0), but this relationship dissipated by 1 wk (AUC = 0.55, 95% CI = 0.31–0.79). Severity of PH did not predict outcome at 1 d (AUC = 0.51, 95% CI = 0.27–0.74), but prediction improved at 1 wk (AUC = 0.80, 95% CI = 0.61–0.99).
Conclusion:
BNP is a strong predictor of clinical outcome in newborns with CDH at 1 d of life.
Similar content being viewed by others
Main
Congenital diaphragmatic hernia (CDH) occurs in approximately 1/5,000 live births (1). The hallmark of this birth defect is lung hypoplasia, which is variable in severity (2,3,4). While the majority of infants with CDH have elevated estimated pulmonary artery pressures (PAp) measured by echocardiography soon after birth, improvement and persistence of pulmonary hypertension (PH), which has been associated with worse outcome, is variable (5,6). Early identification of infants at risk for adverse outcome may allow for more targeted treatment inpatient subgroups.
B-type natriuretic peptide (BNP) is a polypeptide secreted from both cardiac ventricles due to wall stress. Physiologically, BNP counteracts elevated ventricular volume by its natriuretic, diuretic and vasoactive properties (7,8). Plasma BNP levels have been correlated with hemodynamic measurements in adults with primary (9,10) and secondary PH (11), and are predictive of survival (12,13). Similarly, in pediatric patients, BNP levels have been associated with more impaired function of the right ventricle (RV) and worse functional class, and, in children with primary PH, BNP also predicts survival (14). BNP has also been shown to correlate with estimated PAp in newborns with persistent pulmonary hypertension of the newborn (PPHN), but without CDH (15). The only prior systematic study of the BNP pathway in infants with CDH was done by Baptista and colleagues, who evaluated N-terminal-pro-BNP (NT-proBNP) in 13 infants with CDH. They found that higher levels were predictive of death (16).
The pathophysiology of PH in infants with CDH differs from that of other patient groups. Features of the fetal circulation and structural abnormalities are related to the degree of lung hypoplasia with relatively decreased fetal left ventricular (LV) output associated with higher neonatal mortality (2,17,18). In addition, the severity of PH is related to major developmental alterations in the pulmonary vascular bed (3,4). This suggests that chronically increased fetal RV output and temporary alterations in LV conformation may impact the transition to postnatal circulation in CDH. Our study aim was to investigate the prognostic value of plasma BNP and the severity of PH measured by echocardiography at 1 d and 1 wk of life for prolonged respiratory support or death in newborns with CDH. We hypothesized that elevated BNP and more severe PH would be associated with this adverse clinical outcome.
Results
Table 1 shows baseline characteristics of the study population (n = 27). There were 14 infants (52%) with Good outcome (survival and breathing room air without additional respiratory support at 56 d). Of the 13 infants with Poor outcome (death or persistent respiratory support at 56 d), 5 (38%) died and 8 (62%) received prolonged respiratory support.
Blood for BNP level was collected at a median of 9 h of age (range 2–28 h) for the first sample and a median of 7 d of age (range 6–11 d) for the second sample. Echocardiograms were obtained within 24 h of BNP level collection for the first study (median 1 d of age, range 1–2 d) and within 48 h for the second study (median 8 d of age, range 6–10 d). The first BNP sample was collected in 14/14 infants with Good outcome and 11/13 infants with Poor outcome. The second BNP sample was collected in 11/14 infants with Good outcome and 13/13 infants with Poor outcome. Clinical status is summarized for infants with Good and Poor outcome at the time of BNP measurement in Table 2 (concurrent treatment with inhaled nitric oxide (iNO), support with mechanical ventilation and high-frequency ventilation, fraction of inspired oxygen concentration and oxygenation index), or contemporaneous echocardiogram (presence of persistent ductus arteriosus (PDA)).
On the first day of life, median BNP level for the whole cohort was 112 pg/ml (range 6–967 pg/ml). In infants with Poor outcome, BNP levels were significantly higher (median 220 pg/ml, range 30–967 pg/ml) than BNP levels in infants with Good outcome (median 55 pg/ml, range 6–195 pg/ml, P < 0.01, Figure 1 ). At 1 wk of life, median BNP level for the whole cohort was 464 pg/ml (range 76–1,860). At this time point, BNP levels were not significantly different between the two groups (median 547 pg/ml, range 76–1,860 pg/ml in the Poor outcome group vs. median 364 pg/ml, range 84–1,180 pg/ml in the Good outcome group, P = 0.70).
Box and whiskers plots of plasma B-type natriuretic peptide (BNP) levels (pg/ml) in infants surviving and on room air at 56 d of age (Good outcome) and those who died or were on respiratory support at 56 d (Poor outcome) on the (a) first day of life and (b) 1 wk of age. Black dots indicate outliers. * P < 0.01, ** P = 0.7.
BNP levels were available at both time points for 22 infants. In infants with Good outcome (n = 11) the BNP level increased significantly between the two time points (median 40 pg/ml in the first day vs. median 364 pg/ml at 1 wk, P < 0.001). In infants with Poor outcome (n = 11), BNP levels increased between the two time points, but this difference was not statistically significant (median 220 pg/ml in the first day vs. median 547 pg/ml at 1 wk, P = 0.40).
All infants (11/11) with Poor outcome and 13 of 14 (93%) with Good outcome had ≥2/3 systemic pressure estimate by echocardiography in the first 48 h of life ( Figure 2 ). In contrast, at 1 wk of age, 12/13 (92%) of the infants with Poor outcome still had an elevated pressure estimate (PAp ≥ 2/3 systemic), whereas only 6/11 (55%) of the good outcome group had persistent elevated PAp (P = 0.06 for comparison between groups).
Estimated pulmonary artery pressure in infants surviving and on room air (Good outcome) and those who died or were on respiratory support at 56 d (Poor outcome) on (a) the first day of life and (b) 1 wk of age. Black colored area: <2/3 systemic pressure, white colored area: 2/3 to systemic-to-systemic pressure, hatched area: systemic-to-suprasystemic pressure.
The AUC for prediction of clinical outcome by BNP level in the first day was 0.91 (95% CI = 0.77–1.0, Figure 3 ). BNP >188 pg/ml classified 88% correctly with a sensitivity of 82% and a specificity of 93%. For a BNP >188 pg/ml, the positive likelihood ratio (LR) was 11.45 and the negative LR was 0.2, demonstrating that this cut-off may be a robust indicator of outcome in the first day of life in this patient population. At 1 wk, the AUC decreased to 0.55 (95% CI = 0.30–0.79);BNP >496 pg/ml only classified 67% correctly (sensitivity 62% and specificity 73%). In contrast, in the first 48 h of life, the AUC for echocardiographic severity of PH (systemic-to-suprasystemic, 2/3 systemic-to-systemic, and <2/3 systemic) as a predictor of clinical outcome was only 0.51 (95% CI = 0.27–0.74). The predictive ability of echocardiographic classification of PH improved at 1 wk with an AUC of 0.80 (95% CI = 0.61–0.99).
Receiver operator characteristic curves for B-type natriuretic peptide levels (a) in the first day of life (2–28 h, area under the curve (AUC) = 0.91 (95% confidence interval (CI) = 0.77–1.0)) and (b) at 1 wk of age (6–11 d, AUC = 0.55 (95% CI = 0.3–0.79)).
To directly assess the difference between the predictive utility of the two biomarkers (BNP and severity of PH), we compared the ROC curves for each biomarker (i) to each other at 1 d and 1 wk of age and (ii) to itself, assessing the change from 1 d to 1 wk of age. For these analyses, we included only those infants with both measurements available at both time points (n = 22), producing slightly different AUC and 95% CI than reported above ( Table 3 ). At 1 d of age, the AUC for BNP level was significantly better than the AUC for the severity of PH (P = 0.01), but there was no significant difference at 1 wk. In addition, the AUC for BNP level was significantly higher in the first day than at 1 wk (P = 0.01), but there was no significant difference between the two time points for severity of PH.
Discussion
In this prospective cohort, we demonstrate that plasma BNP level on the first day of life is a sensitive and specific prognostic marker for clinical outcome in infants with CDH (AUC = 0.91, 95% CI = 0.77–1.0), superior to estimates of PH severity by contemporaneous echocardiography, which is non-discriminatory. However, BNP loses its discriminative ability for prediction of clinical outcome at 1 wk of life with increasing BNP levels in both the Good and Poor outcome groups. In contrast, as estimated PH severity by echocardiography evolves, echocardiography at 1 wk of age becomes a more useful predictor of outcome (AUC = 0.80, 95% CI = 0.61–0.99).
The only prior systematic study of the BNP pathway in infants with CDH was done by Baptista and colleagues, who evaluated N-terminal-pro-BNP (NT-proBNP) in 13 infants with CDH (16). NT-proBNP is generated from the BNP preprohormone, and it has a longer half-life than BNP. This study identified an NT-proBNP cut-off of 11,500 pg/ml on the first day of life as a sensitive, but not specific, predictor of death. NT-proBNP levels were also correlated with estimated PAp and measures of RV dysfunction.
Various thresholds for BNP have been proposed in the literature for prognostication in patients with PH. Lammers et al. (14) evaluated BNP values as a prognostic biomarker in 27 children (mean 8.4 y) with primary PH. A BNP >130 pg/ml was predictive of death or need for lung transplantation, similar to the findings in our study. In contrast, Reynolds et al. proposed a much higher cut-off value of BNP >550 pg/ml at 1–2 d for diagnosis of PPHN from diverse etiologies (idiopathic, meconium aspiration, birth asphyxia and sepsis (15)). Despite the fact 24/25 infants in our cohort had elevated PAp estimates (≥2/3 systemic) and 15/25 had systemic-to-suprasystemic PH in the first 2 d, BNP levels in both our Good and Poor outcome groups are generally lower than those in the Reynolds study (median BNP for PPHN, 1,610 pg/ml, for respiratory distress without PPHN, 132 pg/ml, and for room air, 248 pg/ml). Ventricular loading may differ in newborns with CDH, given their unique fetal pathophysiology. The decreased left-sided contribution to combined ventricular output may allow the RV to be pre-conditioned to better accommodate the failure to transition to normal postnatal hemodynamic relationships (17,18,19).
The increase in BNP levels over the first week of life in our patients is also notable. In healthy infants, BNP decreases over this time period, the same pattern demonstrated in infants with PPHN in the Reynolds study (20). This most likely reflects resolution of the underlying disease in PPHN. In contrast, in infants with CDH, there may be (i) persistent structural abnormalities in both the Good and Poor outcome groups, and/or (ii) closure of the ductus arteriosus (which occurred in the majority of infants with a Good outcome). It has previously been noted that PH can recur in infants with CDH who had previous resolution by echocardiography, indicating that the normalization of the structural pulmonary vascular abnormalities in CDH can lag behind the improvements seen by imaging (21,22).
The different patterns of our two evolving biomarkers are intriguing. The severity of PH appears to be improving at 1 wk of age in infants with Good outcome, yet BNP levels increase significantly. BNP levels also increase in infants with Poor outcome, while the severity of PH is not improving in these patients. In addition to more severe structural abnormalities, infants with Poor outcome may have increasing vascular dysfunction. We have previously shown that circulating inflammatory markers are elevated in fetuses with more severe CDH (defined as persistence of neonatal PH), and that endothelin-1 levels are elevated at 1 and 2 wk of age in newborns with CDH with Poor outcome (death or discharge on supplemental oxygen (5,23)). In addition, infants with Poor outcome continue to receive substantial oxygen supplementation while on mechanical ventilation at 1 wk of age ( Table 2 ), and supra-physiological oxygen exposure impairs vascular function, as oxygen-reduction balance is altered, endothelial nitric oxide synthase expression and activity are decreased and phosphodiesterase-5 expression and activity are increased (24,25). These initial and exacerbating factors in the face of more profound lung hypoplasia may result in the persistence of more severe PH by echocardiography and more pronounced ventricular wall stress. This pattern over the first 1–2 wk of life in the lung and pulmonary vascular bed of these infants might be critical, and affect subsequent lung growth and function.
The strength of this study is its design. Since BNP levels were only measured for research purposes after sample storage, the treatment team was blinded at all times to BNP values. Thus, BNP did not influence clinical decision-making, eliminating the risk of incorporation bias. Further, although clinical teams were aware of echocardiographic findings at the time of that study, the retrospective scoring based on digitally stored echocardiographic images was done by a single observer blinded to the initial clinical reports and without knowledge of the infant’s outcome.
However, there are limitations. First, there is the possibility that a lack of association is due to low power, which could be a factor in our ROC analyses. But, we have demonstrated alterations in our biomarkers over time, suggesting that patient physiology is changing, and the import of the biomarkers reflects that change.
A second limitation is the short-term nature of the outcome measurement. Poor outcome was defined at 56 d of life. However, we have previously shown that supplemental oxygen at hospital discharge in infants with CDH is associated with worse neurodevelopmental outcomes and multiple medical morbidities (26,27). A final limitation is the lack of accurate estimates of PAp and PVR by echocardiography (28). As a consequence, we categorized estimated PAp into three groups in relation to systemic pressure. However, this limitation may be the precise reason that BNP measurement in the first day of life could be more useful for prognosticating outcome in infants with CDH.
While our results suggest that BNP is a promising early biomarker for outcome in CDH, a multicenter study is necessary to validate the current findings. Additionally, such a design could provide the required power to evaluate the utility of combining multiple fetal and neonatal assessments in a prediction model to improve prognostic accuracy, such as antenatal measurements, BNP and echocardiographic markers.
In conclusion, our results are somewhat surprising. BNP levels are discriminatory for Poor outcome in the first day of life, whereas echocardiography is not. Initial BNP levels are lower than those previously described in PPHN and they increase over the first week, counter to the pattern seen in PPHN and healthy newborns. These findings may be explained by the unique fetal physiology of CDH, demonstrated by circulatory and biochemical differences. Thus, there may be clinical implications for prognostication, as well as targeted therapies, which could be applied during critical periods in lung and pulmonary vascular adaptation in CDH.
Methods
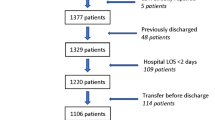
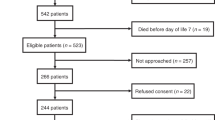
Study Enrollment
Infants with congenital diaphragmatic hernia were eligible if admitted to the Intensive Care Nursery at UCSF Benioff Children’s Hospital. Infants were excluded if they had a multiple malformation syndrome affecting prognosis, Morgagni hernia, or structural congenital heart disease other than an atrial septal defect or patent ductus arteriosus (PDA). Infants were consecutively recruited over 29 mo (May 2011 to September 2013). Thirty-eight infants were admitted; eight declined plasma collection, one died before consent was obtained, and two were excluded. Written informed consent was obtained from at least one parent. The study was approved by the University of California San Francisco Institutional Review Board.
Clinical Management and Data Collection
All infants were intubated and mechanically ventilated immediately after birth. Infants were managed with consistent lung protective ventilation strategies including permissive hypercapnia (pH > 7.2, pCO2 45–65 mmHg), peak inspiratory pressure limitation (PIP < 26 cm H2O), short inspiratory times, to maintain an inspiratory:expiratory ratio of ~1:2 with physiological ventilator rates of 50–90, and permissive hypoxemia (preductal saturation >87%), with allowance for a ductal-level shunt. HFOV was used if infant was unable to be ventilated adequately with the above described conventional mechanical ventilation strategies (with a target mean airway pressure ≤15 cm H2O). Inhaled nitric oxide (iNO) was administered for substantially impaired oxygenation thought to be secondary to PH. Infants with imminent inadequate oxygen delivery were placed on extracorporeal membrane oxygenation (ECMO) support. Dopamine was used to keep mean arterial blood pressure >40 mmHg, Milrinone was used for sever pulmonary hypertension. Surgical repair was performed after clinical stabilization. Once assisted ventilation could be discontinued, supplemental oxygen was administered via nasal cannula to maintain oxygen saturation by pulse oximetry (SpO2) ≥95%. Infants who failed to consistently maintain target SpO2 were discharged on supplemental oxygen. Clinical information, including detailed respiratory support data, was collected.
BNP Levels
Whole blood (1 ml) was collected from an indwelling arterial catheter into a chilled ethylenediaminetetraacetic acid tube on the first day of life and at 1 wk of age. Sample collection was timed with echocardiography whenever possible. Samples were immediately put on ice and centrifuged at 2,000 rpm for 15 min. Plasma was stored (−80 °C) and BNP levels were later measured (Triage Meter Plus, Alere, Waltham, MA), and thus not available to the treatment team. The Triage Meter Plus was calibrated with the Reagent CODE CHIP Module when a new lot of Test Devices was opened. The quality control device was used before each measuring session as suggested by the company. Given the limited amount of plasma available, the samples were not run in duplicates. The coefficient of variation for the Triage Meter Plus is 9.2% −11.4 from low to high BNP concentrations (Triage BNP Test Product Insert, Alere).
Echocardiographic Data
Echocardiography was performed as per clinical protocols using commercially available ultrasound systems (Acuson Sequoia C256 or C512 Ultrasound System, Mountain View, CA) in the first day of life and approximately 1 wk later, per clinical routine. Transthoracic echocardiographic views were retrospectively reviewed by a reader masked to clinical outcome for classification of estimated (PAp) in relationship to systemic systolic blood pressure as previously described (5): <2/3 systemic pressure, 2/3 systemic-to-systemic pressure, or systemic-to-suprasystemic pressure. Three measurements (in descending order of importance) were used to classify the pulmonary-to-systemic pressure relationship by echocardiogram and assess PH due to elevated pulmonary vascular resistance (PVR): (i) pressure differential by direction and velocity of ductus arteriosus flow (Bernoulli equation); (29) (ii) two-dimensional interventricular septum position (parasternal short axis) graded as normal, flat, or D-shaped, with a substantially flattened septum indicating RV pressure 2/3 systemic-to-systemic pressure and D-shaped indicating systemic-to-suprasystemic pressure (30,31); and (iii) peak tricuspid regurgitant jet velocity measured by Doppler with RV systolic pressure estimated by the modified Bernoulli equation and right atrial pressure estimated at 0 mmHg (28).
Primary Outcome
Poor outcome was defined as a composite of death or need for ongoing respiratory support (including oxygen supplementation) at 56 d of age or discharge, whichever came first. This definition of prolonged respiratory support was based on a proposal for the definition of moderate-to-severe bronchopulmonary dysplasia (BPD) for infants born at >32 wk (32). Conversely, Good outcome was defined in surviving infants who were breathing room air without additional respiratory support by 56 d. Although prolonged respiratory support at 56 d has not been validated with respect to later outcomes, we previously showed that infants with CDH discharged on supplemental oxygen had higher rates of neurodevelopmental disability (26).
Statistical Analysis
Non-parametric rank sum test and Fisher exact test were used as appropriate. P values <0.05 were considered significant. Receiver operator characteristic (ROC) curves were analyzed to assess the relationship of BNP level and severity of PH to clinical outcome, with area under the curve (AUC) and 95% CI reported for these estimates (Stata 13.0; College Station, TX).
Statement of Financial Support
This publication was supported by the National Center for Advancing Translational Sciences (USA), National Institutes of Health (NIH; Bethesda, MD, USA), through UCSF-CTSI Grant Number UL1 TR000004 and UL1 RR024131 and HL61284 (J.R.F.). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Disclosure
The authors declare no conflict of interest.
References
Balayla J, Abenhaim HA . Incidence, predictors and outcomes of congenital diaphragmatic hernia: a population-based study of 32 million births in the United States. J Matern Fetal Neonatal Med 2014;27:1438–44.
Naeye RL, Shochat SJ, Whitman V, Maisels MJ . Unsuspected pulmonary vascular abnormalities associated with diaphragmatic hernia. Pediatrics 1976;58:902–6.
Vacanti JP, Crone RK, Murphy JD, et al. The pulmonary hemodynamic response to perioperative anesthesia in the treatment of high-risk infants with congenital diaphragmatic hernia. J Pediatr Surg 1984;19:672–9.
Geggel RL, Murphy JD, Langleben D, Crone RK, Vacanti JP, Reid LM . Congenital diaphragmatic hernia: arterial structural changes and persistent pulmonary hypertension after surgical repair. J Pediatr 1985;107:457–64.
Keller RL, Tacy TA, Hendricks-Munoz K, et al. Congenital diaphragmatic hernia: endothelin-1, pulmonary hypertension, and disease severity. Am J Respir Crit Care Med 2010;182:555–61.
Dillon PW, Cilley RE, Mauger D, Zachary C, Meier A . The relationship of pulmonary artery pressure and survival in congenital diaphragmatic hernia. J Pediatr Surg 2004;39:307–12; discussion 307–12.
Sudoh T, Kangawa K, Minamino N, Matsuo H . A new natriuretic peptide in porcine brain. Nature 1988;332:78–81.
Levin ER, Gardner DG, Samson WK . Natriuretic peptides. N Engl J Med 1998;339:321–8.
Nagaya N, Nishikimi T, Okano Y, et al. Plasma brain natriuretic peptide levels increase in proportion to the extent of right ventricular dysfunction in pulmonary hypertension. J Am Coll Cardiol 1998;31:202–8.
Leuchte HH, Holzapfel M, Baumgartner RA, Neurohr C, Vogeser M, Behr J . Characterization of brain natriuretic peptide in long-term follow-up of pulmonary arterial hypertension. Chest 2005;128:2368–74.
Leuchte HH, Neurohr C, Baumgartner R, et al. Brain natriuretic peptide and exercise capacity in lung fibrosis and pulmonary hypertension. Am J Respir Crit Care Med 2004;170:360–5.
Nagaya N, Nishikimi T, Uematsu M, et al. Plasma brain natriuretic peptide as a prognostic indicator in patients with primary pulmonary hypertension. Circulation 2000;102:865–70.
Surie S, Reesink HJ, van der Plas MN, et al. Plasma brain natriuretic peptide as a biomarker for haemodynamic outcome and mortality following pulmonary endarterectomy for chronic thromboembolic pulmonary hypertension. Interact Cardiovasc Thorac Surg 2012;15:973–8.
Lammers AE, Hislop AA, Haworth SG . Prognostic value of B-type natriuretic peptide in children with pulmonary hypertension. Int J Cardiol 2009;135:21–6.
Reynolds EW, Ellington JG, Vranicar M, Bada HS . Brain-type natriuretic peptide in the diagnosis and management of persistent pulmonary hypertension of the newborn. Pediatrics 2004;114:1297–304.
Baptista MJ, Rocha G, Clemente F, et al. N-terminal-pro-B type natriuretic peptide as a useful tool to evaluate pulmonary hypertension and cardiac function in CDH infants. Neonatology 2008;94:22–30.
Stressig R, Fimmers R, Eising K, Gembruch U, Kohl T . Intrathoracic herniation of the liver (‘liver-up’) is associated with predominant left heart hypoplasia in human fetuses with left diaphragmatic hernia. Ultrasound Obstet Gynecol 2011;37:272–6.
Vogel M, McElhinney DB, Marcus E, Morash D, Jennings RW, Tworetzky W . Significance and outcome of left heart hypoplasia in fetal congenital diaphragmatic hernia. Ultrasound Obstet Gynecol 2010;35:310–7.
Broth RE, Wood DC, Rasanen J, et al. Prenatal prediction of lethal pulmonary hypoplasia: the hyperoxygenation test for pulmonary artery reactivity. Am J Obstet Gynecol 2002;187:940–5.
Koch A, Singer H . Normal values of B type natriuretic peptide in infants, children, and adolescents. Heart (British Cardiac Society) 2003;89:875–8.
Thibeault DW, Mabry SM, Ekekezie II, Truog WE . Lung elastic tissue maturation and perturbations during the evolution of chronic lung disease. Pediatrics 2000;106:1452–9.
Payne NR, Wright G, Kriesmer PJ, et al. Recurrent pulmonary arterial hypertension following neonatal treatment with extracorporeal membrane oxygenation. Crit Care Med 1991;19:1210–2.
Fleck S, Bautista G, Keating SM, et al. Fetal production of growth factors and inflammatory mediators predicts pulmonary hypertension in congenital diaphragmatic hernia. Pediatr Res 2013;74:290–8.
Farrow KN, Groh BS, Schumacker PT, et al. Hyperoxia increases phosphodiesterase 5 expression and activity in ovine fetal pulmonary artery smooth muscle cells. Circ Res 2008;102:226–33.
Farrow KN, Wedgwood S, Lee KJ, et al. Mitochondrial oxidant stress increases PDE5 activity in persistent pulmonary hypertension of the newborn. Respir Physiol Neurobiol 2010;174:272–81.
Cortes RA, Keller RL, Townsend T, et al. Survival of severe congenital diaphragmatic hernia has morbid consequences. J Pediatr Surg 2005;40:36–45; discussion 45–6.
Keller RL, Jancelewicz T, Vu L, et al. Perinatal anatomic and physiologic factors predict neurodevelopmental (ND) disability in congential diaphragmatic hernia (CDH). Abstract Pediatric Academic Society (E-PAS) 2013. (http://www.abstracts2view.com/pasall.)
Mourani PM, Sontag MK, Younoszai A, Ivy DD, Abman SH . Clinical utility of echocardiography for the diagnosis and management of pulmonary vascular disease in young children with chronic lung disease. Pediatrics 2008;121:317–25.
Musewe NN, Smallhorn JF, Benson LN, Burrows PE, Freedom RM . Validation of Doppler-derived pulmonary arterial pressure in patients with ductus arteriosus under different hemodynamic states. Circulation 1987;76:1081–91.
Reisner SA, Azzam Z, Halmann M, et al. Septal/free wall curvature ratio: a noninvasive index of pulmonary arterial pressure. J Am Soc Echocardiogr 1994;7:27–35.
Dong SJ, Smith ER, Tyberg JV . Changes in the radius of curvature of the ventricular septum at end diastole during pulmonary arterial and aortic constrictions in the dog. Circulation 1992;86:1280–90.
Bancalari E, Jobe AH . Bronchopulmonary dysplasia. AJRCCM 2001;163:1723–9.
Acknowledgements
We are grateful to the neonatal research nurses for their help in acquiring and processing the infants’ blood samples, and to the families of the children, for their participation in our research. The results from this study were presented in part at the Pediatric Academic Societies meetings in Washington, DC, and Vancouver, Canada, in May 2013 and 2014.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Steurer, M., Moon-Grady, A., Fineman, J. et al. B-type natriuretic peptide: prognostic marker in congenital diaphragmatic hernia. Pediatr Res 76, 549–554 (2014). https://doi.org/10.1038/pr.2014.136
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2014.136
This article is cited by
-
CA125: a novel cardiac biomarker for infants with congenital diaphragmatic hernia
Pediatric Research (2023)
-
Congenital diaphragmatic hernia
Nature Reviews Disease Primers (2022)
-
Early diagnosis and targeted approaches to pulmonary vascular disease in bronchopulmonary dysplasia
Pediatric Research (2022)
-
Predicting death or extended length of stay in infants with congenital diaphragmatic hernia
Journal of Perinatology (2016)
-
B-type natriuretic peptide as a parameter for pulmonary hypertension in children. A systematic review
European Journal of Pediatrics (2015)