Abstract
Background:
The consumption of polyunsaturated fatty acids has changed, and the prevalence of adiposity has increased over the past 30 y. A decrease of n-3 polyunsaturated fatty acid content in breast milk has been suggested to be a contributing factor. The objective of this study was to investigate the relationship between docosahexaenoic acid (DHA) content and n-6/n-3 polyunsaturated fatty acid ratio in breast milk, body composition, and timing of adiposity rebound in children.
Methods:
In the Copenhagen Prospective Study on Asthma in Childhood birth cohort, breast milk fatty acid profile was determined in 281 mothers and BMI development was prospectively followed up to the age of 7 y in 222 children. Age and BMI at adiposity rebound were registered. Furthermore, fat mass determination by dual energy X-ray absorptiometry was performed in 207 children at 6–9 y of age.
Results:
There was a significant association between breast milk DHA and BMI from 2 to 7 y, fat mass, and, for the girls, age at adiposity rebound. No associations were found between the breast milk n-6/n-3 polyunsaturated fatty acid ratio and body composition.
Conclusion:
Early intake of DHA may have an effect on body composition. Dietary habits of lactating mothers could contribute to the increased prevalence of obesity in Western societies.
Similar content being viewed by others
Main
Studies have shown that dietary habits in infancy and early childhood may have an effect on BMI development and the timing of adiposity rebound (1,2,3). The exact age at adiposity rebound, around 6 y of age, when BMI reaches nadir and then begins to increase, could represent a valid predictor of the development of obesity in adolescence and adulthood (2,4,5). The onset of the stage, in which fat tissue growth depends on differentiation and hypertrophy of existing cells, is also regarded as a sensitive period to the risk of developing obesity. Some studies show that the capacity of adipocyte precursor cells to divide and possibly undergo self-renewal might be highest during the first year of postnatal life (6,7). The identification of factors that affect development and growth of fat cells and the timing of adiposity rebound is essential to the understanding of the mechanisms underlying the development of obesity in children.
Most studies have found that human milk is protective against the development of overweight (8,9). The relative content of the eicosanoid precursors, n-3 and n-6 polyunsaturated fatty acids (PUFA), in breast milk is one of the factors that could play a role (10,11). Differentiation of preadipocytes into mature adipocytes is a process affected by various hormones and growth factors, among other eicosanoids (12,13,14). The n-6 PUFA–derived eicosanoids have been shown to promote preadipocyte differentiation (12,14). Because of the antagonistic functions between n-3 PUFA and n-6 PUFA in biochemical processes and at the paracrine/endocrine level, increased consumption of n-3 PUFA could represent a way to inhibit fat tissue production in prenatal life and during infancy.
The intake of PUFA has, in many Western societies, changed over the past 30 y, thereby affecting the fatty acid profile in breast milk, with a subsequent increase of the n-6/n-3 PUFA ratio and a decrease of the docosahexaenoic acid (DHA, 22:6n-3) content (15). However, few studies have investigated whether this may increase the risk of adiposity in breastfed children.
The aim of this study was to investigate the relationship between the DHA content of breast milk and body composition, measured as development of BMI from age 2 to 7 y, fat mass percentage at 6–9 y, and the age and BMI at onset of adiposity rebound. Associations between the n-6/n-3 PUFA ratio and body composition were performed as supplementation to primary outcome. This was investigated in a large cohort study, the Copenhagen Prospective Study on Asthma in Childhood (COPSAC).
Results
The processes involved in the study and the number of subjects for the different outcomes are outlined in Figure 1 . Of the 411 women in the COPSAC study, breast milk samples were available from 321 participants. Samples taken <13 or >48 d postpartum were excluded because the time of sampling has an effect on PUFA composition (16), leaving 281 subjects with samples eligible for analyses. The mean breast milk sampling time for the included participants was 22 ± 8 d postpartum. Of the 281 subjects, 222 had at least one annual BMI registration throughout the study period (148 participants had BMI data available at all 11 time points, and 38 participants had <10 measurements) and were thus included in the BMI and adiposity rebound analyses. The fat percentage assessments by dual energy X-ray (DXA) were obtained in 207 of the 281 participants (lacking for 32 of the 222 participants with BMI data; 17 had DXA data but were not included in the BMI analysis). There were no differences in BMI development or BMI and age at adiposity rebound between the participants with and without DXA scans. Furthermore, no difference was observed between the included and excluded participants (those with and without breast milk samples) with respect to parental height (P = 0.47 father and P = 0.22 mother) or physical activity level (P = 0.98), BMI (P = 0.75), and fat mass percentage of the child at 6–9 y of age (P = 0.94), but maternal age at delivery (P = 0.03) and income (P < 0.01) was higher in the included group. Table 1 shows the fatty acid composition of the breast milk and characteristics of the study group.
An inverse association was established between breast milk DHA and BMI from 2 to 7 y of age in the multivariable adjusted model ( Table 2 ). Sex-stratified analyses showed that this effect was only statistically significant in the girls, although the estimated effect sizes were similar in both genders. We also found an overall inverse association between breast milk DHA and percentage of body fat, which also persisted for girls in the sex-stratified analysis, but was nonsignificant in boys ( Table 2 ). Furthermore, we found an inverse association between breast milk DHA content and BMI at 7 y of age for both genders ( Table 2 ).
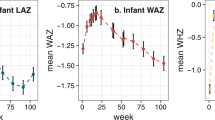
The curves for development of body composition, expressed as mean BMI in the upper quartile compared with the other three quartiles of breast milk DHA, differed significantly ( Figure 2 ), in both crude and adjusted models (data not shown). There was a trend for a positive association between the age at adiposity rebound and the level of DHA in breast milk; this association was significant for girls, whereas no association was observed for boys ( Table 3 and Figure 3 ). Furthermore, a trend of an overall inverse association between BMI at adiposity rebound and DHA in breast milk was established and replicated for girls, but this association was far from significant in boys ( Table 3 ).
No associations were established between the n-6/n-3 PUFA ratio in breast milk and BMI between the age of 2 and 7 y. The breast milk n-6/n-3 PUFA ratio showed a nonsignificant (P = 0.08) tendency of a positive association with percentage of body fat in the adjusted model, but no association was seen with BMI at 7 y. Furthermore, no associations between BMI or age at adiposity rebound and the n-6/n-3 ratio could be established in the adjusted (P = 0.84) or the unadjusted (P = 0.86) models.
Discussion
The key finding in this study was a significant association between DHA in breast milk and BMI development from 2 to 7 y of age and body fat at the ages of 6–9 y. The associations were stronger for girls, who also showed significant association between breast milk DHA and age at adiposity rebound. No significant correlations between breast milk n-6/n-3 PUFA ratio and body composition could be established.
Strengths and Weaknesses
The key strength of this study is that the participants were seen prospectively every 6 mo for 7 consecutive years, because this enabled us to measure growth continuously. The level of participation throughout the study period was high. BMI at 7 y was obtained from 79% of the subjects with milk samples, and data on body fat by DXA scan were obtained from 74% of the subjects. The BMI and fat mass of all participants were measured by experienced examiners using the same device, thereby ensuring high validity of the data. DXA scan is considered a reliable method of quantifying body composition (17). The consistency of the results within the different assessment method confirms the possibility of an adipogenetic effect of dietary PUFA. The study design also ensured a vast amount of data on potential covariates, but we did not have data on parental BMI, and therefore included parental height as a potential covariate. The lack of parental BMI deprived us of a sufficient control for genetic and environmental disposition to body composition (18).
The content of PUFA in breast milk is, by and large, a reflection of the maternal diet (19,20). We obtained only one breast milk sample per participant, which may not be a reliable reflection of the infant’s PUFA supply throughout the lactation period. A study by Lauritzen et al. (21) showed a maximal increase of DHA in breast milk 10 h after ingestion of fish fat and that the effect had almost disappeared after 24 h. It is, therefore, a major weakness in our study that we did not make multiple breast milk samplings. However, all the milk samples were obtained within a narrow range of time, ensuring comparable values of PUFA to which the children were exposed, as the levels of PUFA have been shown to change throughout the lactation period (22). The dietary habits of the mother will inevitably have an effect on her choice of food presented to the child. The observed effect may therefore be a reflection of a dietary lifestyle passed on to the child, which we could not adjust for due to lack of data on the child’s diet in the study period. Previous studies have found associations between socioeconomic status and dietary habits, including PUFA intake (23) and childhood BMI (24). The association found in this study could therefore represent an effect of a healthy lifestyle on multiple levels, hence, not an isolated effect of DHA in breast milk. We sought to adjust for this by including household income and mother’s age at birth, which are associated with maternal education to some extent (25), but this did not change the observed associations with breast milk DHA. This either confirms a DHA-mediated effect or indicates that the chosen confounders are insufficient parameters of socioeconomic status.
The COPSAC cohort consists of children born to atopic mothers. It is possible that both the fatty acid composition in the milk samples and the pattern of growth in the children could be influenced by the underlying atopic disposition. Previous studies have investigated whether atopy is related to breast milk PUFA (26). However, Lauritzen et al. did not find that the fatty acid composition was affected by atopy in the COPSAC cohort (26). The interaction between adiposity and asthma has been extensively studied, mainly focusing on obesity as a cause of asthma (27), but obesity and asthma may have a common etiology. The atopic disposition in the COPSAC cohort could therefore affect the growth pattern in the children and be a factor to take into account when interpreting the results from the study.
Interpretation
To our knowledge, only a few studies have investigated the long-term effect on growth in relation to PUFA supply during lactation. Helland et al. supplemented 314 women with fish oil or corn oil from wk 18 of pregnancy to 3 mo postpartum and did not demonstrate a correlation between breast milk DHA obtained 4 wk and 3 mo postpartum and BMI at 7 y (28). Lauritzen et al. conducted a similar study and found a positive association between DHA in breast milk obtained 4 mo postpartum and BMI in the two-and-a-half year-old children (10), but the effect did not persist when the children reached 7 y of age (29). Both studies were interventional trials, whereas this study is observational, and as a consequence our findings must be interpreted with caution. However, our study differs from previous trials because we have continuous measurements of BMI from 2 to 7 y, enabling us to identify the time of adiposity rebound, an unexplored field in relation to PUFA intake during infancy. We were also able to study the impact of DHA on body fat assessed by DXA. The age of adiposity rebound is regarded as a critical period for development of later adiposity (2,5), and early postnatal life is a critical period during which dietary factors might program adaptive mechanisms with an impact on adiposity rebound and subsequent growth (4). A study by Taylor et al. confirmed from continuous DXA scans, on 39 girls of age 3–6 y, that the onset of adiposity rebound is caused by deposition of fat rather than increased lean mass or slower height acquisition, which could be a possibility when evaluating growth from BMI measurements (30). This is confirmed by our results.
Factors affecting adipocyte differentiation are essential to the growth pattern in childhood. The differentiation of preadipocytes into mature adipose cells is influenced by prostacyclin, a metabolic product of arachidonic acid (13,31). The n-3 PUFA and n-6 PUFA compete in several steps of the metabolic pathway, both with respect to membrane incorporation, eicosanoid production, and eicosanoid action. A diet rich in DHA could suppress the arachidonic acid–mediated effects on adipocyte development, i.e., high levels of DHA in the infants dietary supply could downregulate adipose tissue hyperplasia, and thereby delay the age at adiposity rebound.
Conclusion
This study suggests a relationship between infant DHA exposure and childhood growth, observed by changes in the timing of adiposity rebound, fat mass, and BMI. Our findings add to the many dietary and lifestyle factors involved in the increased prevalence of obesity in children and adults observed in Western societies. Further studies are needed to elucidate a possible causality between the PUFA supply in infancy and the pattern of growth in childhood.
Methods
Subjects
COPSAC is a single-center, birth cohort study designed to assess genetic–environmental interaction in high-risk infants and young children to identify early-life exposures that can be modified to prevent the development of atopic diseases. The COPSAC cohort has previously been described in detail (32,33). A total of 411 infants of asthmatic mothers were enrolled at the age of 1 mo. At 2 y, 93% of the infants were still active in the cohort. Assessments included growth measurements at all visits to the clinical research unit at 6-mo intervals until the age of 7. The study was conducted in accordance with the guiding principles of the Declaration of Helsinki and was approved by the Ethics Committee for Copenhagen (KF 02-118/98) and the Danish Data Protection Agency (1998-1200-359). Data validity was assured by compliance with Good Clinical Practice guidelines and quality control procedures.
Mothers’ Milk Samples
Samples of 2–5 ml of mother’s milk were obtained from the mother ~1 mo after delivery. Time of sampling during the feed was left to the mothers’ choice because the fatty acid composition does not change during feeding (34). Milk aliquots of 2 ml were then added 0.01% 2,6-di-tert-butyl-4-methylphenol (Sigma Chemical, St Louis, MO) and frozen at −80 °C. All milk samples were analyzed within 1 y after collection. Lipids from 1-ml of milk were extracted and methylated with potassium hydroxide in methanol (35). The resulting fatty acid methyl esters were extracted with heptane and separated by gas–liquid chromatography (Hewlett-Packard, Waldbronn, Germany) as previously described (26). We identified peaks from lauric acid (12:0) to DHA based on retention time of commercial standards (Nu-Chek-Prep, Elysian, MN). Ninety-seven percent of the fatty acids in this interval were identified. The content of individual fatty acids or fatty acid classes is given as a percentage by weight of total fatty acid content.
Growth
Height was measured by Harpenden stadiometer (Holtain, Crymych, UK). Weight was measured using calibrated digital weight scales. BMI was calculated as weight (kg)/height (m2). Age and BMI at adiposity rebound were graphically identified from individual BMI curves for each participant. Z-scores were calculated in accordance with World Health Organization recommendations (WHO Child Growth Standards, http://www.who.int/childgrowth/standards/en/). Because the aim of this study was to explore the long-term effect of breast milk PUFA on growth, only growth data from 2 to 7 y of age were used for analyses.
DXA Scanning
DXA scanning was performed between the ages of 6 and 9 y (mean 6.9 ± 0.7, range 6.4–9.6 y) after oral and written informed consent was obtained from the children and parents. The DXA-scanning measures of bone and soft tissue composition were performed for the whole body and subregions such as arms, legs, and trunk (17). A whole-body scan was performed with a Lunar iDXA densitometer (GE Healthcare, Fairfield, CT), with the child lying in situ on his or her back. The scan was done from head to toes in one movement and lasted ~3 min. All scans were performed by three experienced examiners. All scan data were scrutinized by an experienced specialist, and data analyses were performed with enCore software (Minneapolis, MN). Weight and height were registered for all participants on the day of the DXA scan, and percentage of body fat was calculated as the measured fat mass divided by the total body weight.
Physical activity level was registered by an omnidirectional accelerometer Actical (Philips Respironics, Murrysville, PA) placed on the ankle and worn day and night over an average period of 26 d (range 7–28 d). Physical activity level was registered at 5 y (range 4–7) and expressed as counts/min, previously described in detail (36).
Statistical Analyses
Results are given as mean ± SD for all Gaussian-distributed data and as median (25th–75th percentile) for non-Gaussian-distributed data. The distribution of data was tested with Q–Q plots and histograms. Linearity between the variables was tested by scatter plots, and homogeneity of variance was tested using residual plots and Levene’s test. In case of model control deviance, log-transformed values were used for analyses. Statistical analyses were performed with SAS software (version 9.2; SAS Institute, Cary, NC), and P < 0.05 was chosen as the level of significance.
The association between BMI development from 2 to 7 y of age and breast milk DHA and n-6/n-3 PUFA ratio was analyzed by linear mixed models for repeated measurements in a longitudinal design. To further study the long-term effect of breast milk DHA and n-6/n-3 PUFA ratio on growth, the association between the fatty acids and BMI at 7 y was analyzed by multiple regressions using a generalized linear model. Likewise, the association between fatty acids and percentage of body fat by DXA was analyzed by generalized linear models. Analysis between DHA and n-6/n-3 ratio and age and BMI at adiposity rebound was performed by generalized linear models. Potential covariates were chosen in accordance with previous findings and included the duration of exclusively breastfeeding (8,9), sex of the participants, exact age at examination, parental height (parental BMI was not accessible), maternal age at delivery (37), and socioeconomic status classified as household income over the child’s first year (38). Physical activity level was also included as a potential covariate. All the potential covariates were analyzed for correlations to the dependent variables and excluded from the multivariable-adjusted regression analyses by stepwise backward elimination with a cutoff P value of 0.15. Total PUFA content of the breast milk was included as a covariate when analyzing the correlation between n-6/n-3 PUFA ratio and BMI or fat mass.
Statement of Financial Support
The Copenhagen Prospective Studies on Asthma in Childhood (COPSAC) project is funded by private and public research funds (listed on www.copsac.com). The Lundbeck Foundation, the Danish Strategic Research Council, the Pharmacy Foundation of 1991, Augustinus Foundation, the Danish Medical Research Council, and the Danish Pediatric Asthma Centre provided the core support for the COPSAC research center. No pharmaceutical company was involved in the study. The funding agencies did not have any role in design and conduct of the study, collection, management, and interpretation of the data, or preparation, review, or approval of the manuscript.
References
Dietz WH . Critical periods in childhood for the development of obesity. Am J Clin Nutr 1994;59:955–9.
Rolland-Cachera MF, Deheeger M, Bellisle F, Sempé M, Guilloud-Bataille M, Patois E . Adiposity rebound in children: a simple indicator for predicting obesity. Am J Clin Nutr 1984;39:129–35.
Rolland-Cachera MF, Deheeger M, Guilloud-Bataille M, Avons P, Patois E, Sempé M . Tracking the development of adiposity from one month of age to adulthood. Ann Hum Biol 1987;14:219–29.
Rolland-Cachera MF, Deheeger M, Maillot M, Bellisle F . Early adiposity rebound: causes and consequences for obesity in children and adults. Int J Obes (Lond) 2006;30: Suppl 4:S11–7.
Taylor RW, Grant AM, Goulding A, Williams SM . Early adiposity rebound: review of papers linking this to subsequent obesity in children and adults. Curr Opin Clin Nutr Metab Care 2005;8:607–12.
Stettler N, Zemel BS, Kumanyika S, Stallings VA . Infant weight gain and childhood overweight status in a multicenter, cohort study. Pediatrics 2002;109:194–9.
Chomtho S, Wells JC, Williams JE, Davies PS, Lucas A, Fewtrell MS . Infant growth and later body composition: evidence from the 4-component model. Am J Clin Nutr 2008;87:1776–84.
Arenz S, Rückerl R, Koletzko B, von Kries R . Breast-feeding and childhood obesity–a systematic review. Int J Obes Relat Metab Disord 2004;28:1247–56.
Bergmann KE, Bergmann RL, Von Kries R, et al. Early determinants of childhood overweight and adiposity in a birth cohort study: role of breast-feeding. Int J Obes Relat Metab Disord 2003;27:162–72.
Lauritzen L, Hoppe C, Straarup EM, Michaelsen KF . Maternal fish oil supplementation in lactation and growth during the first 2.5 years of life. Pediatr Res 2005;58:235–42.
Lucia Bergmann R, Bergmann KE, Haschke-Becher E, et al. Does maternal docosahexaenoic acid supplementation during pregnancy and lactation lower BMI in late infancy? J Perinat Med 2007;35:295–300.
Ailhaud G, Guesnet P, Cunnane SC . An emerging risk factor for obesity: does disequilibrium of polyunsaturated fatty acid metabolism contribute to excessive adipose tissue development? Br J Nutr 2008;100:461–70.
Gregoire FM, Smas CM, Sul HS . Understanding adipocyte differentiation. Physiol Rev 1998;78:783–809.
Lapillonne A, Clarke SD, Heird WC . Plausible mechanisms for effects of long-chain polyunsaturated fatty acids on growth. J Pediatr 2003;143:Suppl 4:S9–16.
Sanders TA . Polyunsaturated fatty acids in the food chain in Europe. Am J Clin Nutr 2000;71:Suppl 1:176S–8S.
Yu G, Duchén K, Björkstén B . Fatty acid composition in colostrum and mature milk from non-atopic and atopic mothers during the first 6 months of lactation. Acta Paediatr 1998;87:729–36.
Pietrobelli A, Formica C, Wang Z, Heymsfield SB . Dual-energy X-ray absorptiometry body composition model: review of physical concepts. Am J Physiol 1996;271(6 Pt 1):E941–51.
Maffeis C . Aetiology of overweight and obesity in children and adolescents. Eur J Pediatr 2000;159:Suppl 1:35–44.
Jensen CL, Lapillonne A . Docosahexaenoic acid and lactation. Prostaglandins Leukot Essent Fatty Acids 2009;81:175–8.
Scopesi F, Ciangherotti S, Lantieri PB, et al. Maternal dietary PUFAs intake and human milk content relationships during the first month of lactation. Clin Nutr 2001;20:393–7.
Lauritzen L, Jørgensen MH, Hansen HS, Michaelsen KF . Fluctuations in human milk long-chain PUFA levels in relation to dietary fish intake. Lipids 2002;37:237–44.
Makrides M, Simmer K, Neumann M, Gibson R . Changes in the polyunsaturated fatty acids of breast milk from mothers of full-term infants over 30 wk of lactation. Am J Clin Nutr 1995;61:1231–3.
Smith GD, Brunner E . Socio-economic differentials in health: the role of nutrition. Proc Nutr Soc 1997;56(1A):75–90.
Parsons TJ, Power C, Logan S, Summerbell CD . Childhood predictors of adult obesity: a systematic review. Int J Obes Relat Metab Disord 1999;23 : Suppl 8:1–107.
Olsen J, Frische G . Social differences in reproductive health. A study on birth weight, stillbirths and congenital malformations in Denmark. Scand J Soc Med 1993;21:90–7.
Lauritzen L, Halkjaer LB, Mikkelsen TB, et al. Fatty acid composition of human milk in atopic Danish mothers. Am J Clin Nutr 2006;84:190–6.
Shore SA . Obesity and asthma: possible mechanisms. J Allergy Clin Immunol 2008;121:1087–93; quiz 1094–5.
Helland IB, Smith L, Blomén B, Saarem K, Saugstad OD, Drevon CA . Effect of supplementing pregnant and lactating mothers with n-3 very-long-chain fatty acids on children’s IQ and body mass index at 7 years of age. Pediatrics 2008;122:e472–9.
Asserhøj M, Nehammer S, Matthiessen J, Michaelsen KF, Lauritzen L . Maternal fish oil supplementation during lactation may adversely affect long-term blood pressure, energy intake, and physical activity of 7-year-old boys. J Nutr 2009;139:298–304.
Taylor RW, Goulding A, Lewis-Barned NJ, Williams SM . Rate of fat gain is faster in girls undergoing early adiposity rebound. Obes Res 2004;12:1228–30.
Massiera F, Saint-Marc P, Seydoux J, et al. Arachidonic acid and prostacyclin signaling promote adipose tissue development: a human health concern? J Lipid Res 2003;44:271–9.
Bisgaard H . The Copenhagen Prospective Study on Asthma in Childhood (COPSAC): design, rationale, and baseline data from a longitudinal birth cohort study. Ann Allergy Asthma Immunol 2004;93:381–9.
Bisgaard H, Halkjaer LB, Hinge R, et al. Risk analysis of early childhood eczema. J Allergy Clin Immunol 2009;123:1355–60.e5.
Gibson RA, Kneebone GM . Effect of sampling on fatty acid composition of human colostrum. J Nutr 1980;110:1671–5.
Bligh EG, Dyer WJ . A rapid method of total lipid extraction and purification. Can J Biochem Physiol 1959;37:911–7.
Brasholt M, Baty F, Bisgaard H . Physical activity in young children is reduced with increasing bronchial responsiveness. J Allergy Clin Immunol 2010;125:1007–12.
Delbaere I, Verstraelen H, Goetgeluk S, Martens G, De Backer G, Temmerman M . Pregnancy outcome in primiparae of advanced maternal age. Eur J Obstet Gynecol Reprod Biol 2007;135:41–6.
Luo ZC, Wilkins R, Kramer MS; Fetal and Infant Health Study Group of the Canadian Perinatal Surveillance System. Effect of neighbourhood income and maternal education on birth outcomes: a population-based study. CMAJ 2006;174:1415–20.
Acknowledgements
The authors thank the children and parents who participated in the COPSAC cohort and the COPSAC study team.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pedersen, L., Lauritzen, L., Brasholt, M. et al. Polyunsaturated fatty acid content of mother’s milk is associated with childhood body composition. Pediatr Res 72, 631–636 (2012). https://doi.org/10.1038/pr.2012.127
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2012.127
This article is cited by
-
Maternal childhood trauma is associated with offspring body size during the first year of life
Scientific Reports (2022)
-
Early infant adipose deposition is positively associated with the n-6 to n-3 fatty acid ratio in human milk independent of maternal BMI
International Journal of Obesity (2017)
-
Breastmilk from obese mothers has pro-inflammatory properties and decreased neuroprotective factors
Journal of Perinatology (2016)
-
Alpha-linolenic acid (ALA) is inversely related to development of adiposity in school-age children
European Journal of Clinical Nutrition (2015)
-
Effect of maternal n-3 long-chain polyunsaturated fatty acid supplementation during pregnancy and/or lactation on adiposity in childhood: a systematic review and meta-analysis of randomized controlled trials
European Journal of Clinical Nutrition (2014)