Abstract
Infants with chronic lung disease (CLD) have a capacity to maintain functional lung volume despite alterations to their lung mechanics. We hypothesize that they achieve this by altering breathing patterns and dynamic elevation of lung volume, leading to differences in the relationship between respiratory muscle activity, flow and lung volume. Lung function and transcutaneous electromyography of the respiratory muscles (rEMG) were measured in 20 infants with CLD and in 39 healthy age-matched controls during quiet sleep. We compared coefficient of variations (CVs) of rEMG and the temporal relationship of rEMG variables, to flow and lung volume [functional residual capacity (FRC)] between these groups. The time between the start of inspiratory muscle activity and the resulting flow (tria)—in relation to respiratory cycle time—was significantly longer in infants with CLD. Although FRC had similar associations with tria and postinspiratory activity (corrected for respiratory cycle time), the CV of the diaphragmatic rEMG was lower in CLD infants (22.6 versus 31.0%, p = 0.030). The temporal relationship of rEMG to flow and FRC and the loss of adaptive variability provide additional information on coping mechanisms in infants with CLD. This technique could be used for noninvasive bedside monitoring of CLD.
Similar content being viewed by others
Main
Chronic lung disease (CLD) of infancy represents the final common pathway of a heterogeneous group of pulmonary diseases that start in the neonatal period and usually evolve from acute respiratory disorders experienced by newborn infants (1). Tidal breathing parameters, lung volume, and ventilation homogeneity are affected by the morphologic changes in CLD and can be measured by lung function studies. Some studies showed decreased end-expiratory volume [functional residual capacity (FRC)] and lung clearance index (LCI) (2) in sedated infants, whereas other studies in infants during natural sleep could not confirm these observed differences in FRC and LCI between healthy infants and infants with CLD (3). We (4) and other authors (3) indicated that the latter findings are in line with the following clinical observations: infants with CLD in natural sleep may have a high capacity to maintain relatively normal lung volume and relatively normal gas exchange, despite alterations to their lung mechanics, whereas this capacity may be reduced during sedation.
Recently, we described the combination of matched tidal breathing measurements and transcutaneous electromyography of the respiratory muscles (rEMG) in healthy infants (5). Our findings suggested that the interaction of the respiratory muscles and lung mechanics are actively controlled breath to breath and that simultaneous measurement of tidal breathing parameters and rEMG parameters potentially provide a more comprehensive picture of pulmonary mechanics in disease. We hypothesize that infants with CLD attempt to maintain a relatively normal lung volume by altering breathing patterns and dynamical elevation of lung volume. These mechanisms may be detected by differences in the temporal relationship between rEMG, flow pattern and lung volume.
The aim of this study was to determine the temporal relationship between rEMG and tidal flow, the variability of these parameters, and the relationship to lung volume in infants with CLD, in comparison with age-matched healthy controls during unsedated sleep.
METHODS
Study design.
As described below, rEMG was measured at the postmenstrual age of 44 wk, in infants with CLD and age-matched healthy infants, before the fitting of the face mask and on three occasions parallel to standardized lung function tidal flow and volume measurements (6), during quiet unsedated sleep. This was then followed by further rEMG measurements during multibreath FRC measurements, during the same sleep stage.
Subjects.
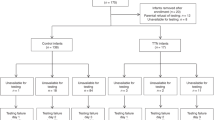
Twenty infants with a history of mild to moderate CLD, defined according to the criteria of Jobe et al. (7), were recruited for this study from the neonatal unit of the University Maternity Hospital (Bern, Switzerland).
Thirty-nine healthy term-born infants were recruited for an ongoing birth cohort study in Bern, Switzerland (5,8,9). Patient data are given in Table 1.
The study was approved by the Medical Ethics Committee of the University Hospital and the Canton of Bern, and written informed consent was obtained from all parents.
Measurement procedure.
Infants were studied during quiet sleep in supine position with the head in midline and with a mask (size 1, Homedica, Cham, Switzerland) placed over the mouth and nose. All measurements were done according to the standards of infant lung function testing, which ensures that resistive properties or dead space of the equipment did not exceed the recommended limits (6,10,11). Sleep state was defined clinically by using the criteria of Prechtl (12).
Lung function.
Flow was measured using a prototype ultrasonic flowmeter (ExhalyzerD; Eco Medics AG, Duernten, Switzerland). Main tidal breathing outcome parameters were respiratory frequency (f), inspiratory time (tI), expiratory time (tE), ratio of time to peak tidal expiratory flow and tE (tPTEF)/tE, tidal volume (VT), and minute ventilation (V′E). Three series of multibreath washout procedures using sulfur hexafluoride tracer gas were performed, and an average was obtained for FRC, calculated using an optimized analysis method (13).
rEMG recordings.
The electrical activity of the diaphragm and intercostal muscles were measured transcutaneously. The technical aspects of the measurements and validation have been previously described (5,14). Thirty breathing cycles of the rEMG-measurement were sampled before lung function measurements were started (T0). The face mask and flow sensor were then placed on the infant, and subsequently the rEMG-activity of the first 30 breaths was recorded in parallel to tidal flow measurements (T1), followed by a sequence of 30 breaths after 2 min (T2) and by a third sequence of 30 breaths (T3) after 8–10 min (the total duration of the measurement).
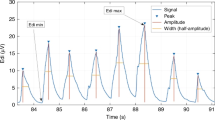
Main rEMG outcome variables (5) were inspiratory time of the rEMG (tI,rEMG), expiratory time of the rEMG (tE,rEMG), postinspiratory activity time (tpia), and ramp inspiratory activity time (tria). The variability in the relative contribution of the respiratory muscles is expressed as the coefficient of variation (CV) of the inspiratory peak value, as the SD was linearly related to the mean. The data processing and analysis were done using the data acquisition and processing package Polybench (Applied Biosignals, Weener, Germany).
Data analysis and statistics.
Dependent on the distribution of the group data, descriptive statistics, t test and nonparametric tests were performed to compare tidal breathing parameters, FRC, and rEMG variables, between healthy infants and infants with CLD. Linear regression analysis was used to compare rEMG, flow timing parameters, and lung volume. Statistical analysis and graphics were performed with SPSS (version 16.0 SPSS Inc., Chicago, IL) and SigmaPlot (version 10.0, Systat Software Inc., Richmond, CA).
RESULTS
Group median values (range) of tidal breathing indices measured at the airway opening and derived from rEMG, and FRC of healthy infants and infants with CLD, are summarized in Table 2. Significant differences between both groups were found for tI,tPTEF/tE,tI,rEMG, and tria corrected for the respiratory cycle time of the rEMG (ttot,rEMG). All other tidal parameters and FRC were not different between the groups.
The mean CV of the intercostal muscles and the diaphragm activity of infants with CLD were 11.2 and 22.6%, respectively (Table 2). The CV of diaphragm activity was significantly lower (p = 0.03) in comparison with healthy infants.
With tidal breathing, f and VT measured at the airway opening changed in both groups in response to the face mask load, even though there was a large variability within the groups. We found a significant decrease of the f (p = 0.002) and V′E (p = 0.003) between T2 and T3 in healthy infants, whereas in contrast, in infants with CLD, there was a significant increase of the f (p = 0.039) between T1 and T2. Furthermore, V′E significantly decreased (p = 0.013) between T2 and T3 in infants with CLD (Table 3).
With regard to the rEMG timing indices, we found a significant increase (p = 0.032) of tpia/ttot,rEMG between T2 and T3 and a significant decrease (p = 0.009) in tria/ttot,rEMG between T2 and T3 in infants with CLD but not in healthy infants. Figure 1 shows the group mean response of the tidal breathing parameters and rEMG variables in response to the face mask load in healthy infants and infants with CLD, at the three time points T1, T2, and T3.
The response of the tidal breathing parameters (f, VT, and V′E) and rEMG parameters (tpia/ttot,rEMG and tria/ttot,rEMG) to the onset of the elastic and compliant face mask load of the three sequence of 30 breaths (T1, T2, T3, see text) in healthy infants and infants with CLD. Solid gray line: healthy infants; solid black line: infants with CLD. *p < 0.05 with Mann-Whitney U test for unpaired measurements (between T1 and T2). **p < 0.05 with Mann-Whitney U test for unpaired measurements (between T2 and T3). Arrow line with § indicates p < 0.05 with Wilcoxon test of the paired measurements.
Although there was no significant difference in FRC corrected for bodyweight between healthy infants and infants with CLD (Table 2), the relationship between respiratory muscle activity and FRC was different between the groups. Although the relationship between muscle activity and FRC was weakly correlated and showed large intrasubject variability, intersubject variability, and overlap between the groups, we nevertheless found a significant positive correlation between tria/ttot,rEMG (means of 30 breaths) and FRC (mL/kg) (r = 0.39, p < 0.001) and a significant negative relation between tpia/ttot,rEMG and FRC expressed in mL/kg (r = −0.33, r2 = 0.11, p < 0.001; Fig. 2) in infants with CLD.
Relationship between tria/ttot,rEMG (A) and FRC (mL/kg) in infants with CLD (•) (r = 0.39, r2 = 0.15, p < 0.001) and healthy infants(▵) (no significant relation). Relationship between tpia/ttot,rEMG (B) and FRC (mL/kg) (r = −0.33, r2 = 0.11, p < 0.001) in infants with CLD (•) and healthy infants (▵) (r = 0.34, r2 = 0.12, p < 0.001).
In healthy infants, we determined a significant positive correlation between tpia/ttot,rEMG (means of 30 breaths) and FRC expressed in mL/kg (r = 0.34, p < 0.001) and no correlation between the FRC and the ratio tria/ttot,rEMG (Fig. 2). This cross-sectional analysis was performed in all measurements per group.
DISCUSSION
In this study, comparison of tidal breathing and rEMG variables between healthy infants and infants with CLD showed a significantly longer delay between the start of inspiratory muscle activity and the resulting flow, corrected for the respiratory cycle time and a significantly shorter tI and tPTEF/tE in the CLD group. This indicates longer inspiratory muscle efforts at the end of expiration before inspiratory flow at the airway opening can occur. Respiratory rate, VT, tria/ttot,rEMG, and tpia/ttot,rEMG responded differently to the fitting of the face mask in the CLD group.
Although FRC was similar in healthy infants and in infants with CLD, it was found to be weakly but positively correlated on a group level to tpia/ttot,rEMG in healthy infants and negatively correlated in infants with CLD. Unlike in healthy infants, we found a positive relation between tria/ttot,rEMG and FRC in infants with CLD. The variability of the diaphragmatic muscle activity in infants was higher in CLD in comparison with the healthy infants at a similar sleep stage.
Interpretation of the findings and possible mechanism.
As previously reported in unsedated infants with and without CLD (4), and consistent with Hulskamp et al. (3), we found no differences between FRC corrected for bodyweight in infants with CLD in comparison with healthy infants. These findings are consistent with previous observations, which found that infants have a high capacity to dynamically maintain their lung volume (15–17). Postinspiratory muscle activity and ramp inspiratory muscle activity during expiration are important to actively control end-expiratory level in infants (17–19). Our current findings suggest that infants with CLD attempt to control their end-expiratory level by using different breathing strategies and different respiratory muscle activation patterns, compared with those used by healthy infants. Infants with CLD start their inspiratory muscle activity much earlier during expiration than healthy infants.
In healthy infants, ramp inspiratory muscle activity was not positively correlated to FRC, but longer postinspiratory muscle activity was correlated with FRC. Our findings are consistent with the hypothesis that healthy infants dynamically elevate their end-expiratory volume by increasing their postinspiratory muscle activity. We speculate that these breathings strategies are energetically less demanding than the breathing strategies that are needed in restrictive and obstructive lung mechanics in CLD. However, the relationship between these timing indices and FRC are very weak and highly variable on a group level. These changes in timing indices of the muscle-flow interaction must be seen as indirect markers of how neurorespiratory control reacts on changes in lung mechanics.
Neurorespiratory control is based on a feedback loop system influenced by many factors. These feedback loops consist of the respiratory oscillator in the brainstem, efferent neural activity, muscle characteristics and their activation pattern, lung and upper airway mechanics, and afferent mechano- and chemoreceptor activity (20). Most of these components can adapt breath by breath, resulting in a highly variable breathing pattern in infants (21–23). If one of these components is altered or restricted, then the system loses a certain degree of freedom and likely variability. In our previous work in healthy infants, we found that breath-to-breath variability is mostly seen in the diaphragm (5). In disease, this variability is decreased, consistent with a loss of breath-to-breath adaptive capacity of the respiratory system in disease, and the control system becomes more deterministic.
Another possible explanation for the reduced variability of diaphragm activity compared with term infants could be abnormalities in diaphragm function caused by prolonged mechanical ventilation (24), which may well persist into the postweaning period. Although these factors cannot be examined in detail in this study, dysfunction may be additionally exacerbated by impaired muscular function from atrophy, apoptosis, and altered composition due to ventilation, exposure to reactive oxygen species, sepsis, drugs (25), and so on in infants with CLD.
Effect of the face mask load.
Both healthy infants and infants with CLD changed their V′E in response to the resistive and elastic mechanical load of a face mask and flow sensor. This may also be seen as a model of the adaptive response. Both groups first increased their respiratory rate and decreased their VT. Then, healthy infants were able to elevate their VT and decrease their respiratory rate, whereas infants with CLD compensated with a further decrease of their VT and a stabilized respiratory rate. Thus, infants with CLD compensate with different strategies to achieve optimal ventilation. The changes on the response on the face mask in the different groups are small, and the patterns were similar. However, we hypothesize that a possible explanation for this difference is the low compliance of the lung in infants with CLD, whereby the muscle activity to increase pressure needed to generate higher tidal volumes is greater (although this difference was not significant). Moreover, ramp inspiratory activity was prolonged in response to the load. This is theoretically consistent with an increase in expiratory pressure or with higher lung volumes.
Clinical relevance.
In addition to the physiologic insights provided, the observation per se of differences in timing and variability between health and CLD in the absence of differences in FRC is potentially of clinical significance. A larger study investigating whether this apparent lack of coupling between FRC and EMG measurements are related to clinical parameters relevant to CLD would be necessary to ascertain its diagnostic or monitoring value.
Recently, long-term outcome studies of preterm children without and with CLD showed an impaired lung function and increasing respiratory morbidity at older age (26–28). Such alterations are often not easy to identify in newborn infants with CLD due to the adaptive mechanisms, which can come into play when infants are not sedated. Combined rEMG-measurements with matched tidal flow will improve the understanding of changes in lung function and physiologic development in infants with CLD. Our findings demonstrate that this combination of measurements may help to understand why infants with CLD can maintain relatively normal lung volume and gas exchange if they are spontaneously breathing but not when their neurorespiratory control is reduced during sedation.
Methodological aspects.
The transcutaneous way of assessing electrical activity of the respiratory muscles is favorable in infants with CLD because it is noninvasive. Transcutaneous recordings of the electrical activity of the respiratory muscles have been criticized, especially because of contamination of these signals by the electrical activity of other muscles (29). In an earlier case report, we clearly showed the absence of contamination of abdominal muscle activity during the measurements during quiet sleep (30). This is in line with the observation of Praud et al. (31) who reported no activity of abdominal muscles during quiet sleep.
A further limitation of the study is that the relationship between rEMG-flow time indices and lung volume is based on intraindividual and interindividual data. As infants have to be studied during their natural sleep, there is no other way to get this information other than by observational studies. The advantage of the observational approach is the fact that the findings represent a real-life situation.
Summary.
Although V′E and FRC were similar in infants with CLD, the temporal dynamic interaction between respiratory muscle activity, resulting flow and lung volume was altered. The temporal relationship of rEMG to flow and the loss of variability provide additional information on coping mechanisms in infants with impaired lung mechanics, which are not obvious from tidal breathing and lung volume measurements alone. This information is easy to obtain with rEMG measurements, with matched tidal breathing measurements and may be useful as noninvasive clinical monitoring tools for disease progression in the future. Furthermore, with the increasing interest in EMG-triggered ventilation of infants with lung disease, our findings are crucial because the timing relationship between muscle activity, resulting flow and lung volume is different in health and disease.
Abbreviations
- CLD:
-
chronic lung disease
- CV:
-
coefficient of variation
- f :
-
respiratory frequency
- FRC:
-
functional residual capacity
- LCI:
-
lung clearance index
- rEMG:
-
transcutaneous electromyography of the respiratory muscles
- t E :
-
expiratory time
- t I :
-
inspiratory time
- t pia :
-
postinspiratory activity time
- tPTEF/tE:
-
ratio of time to peak tidal expiratory flow and tE
- t ria :
-
ramp inspiratory activity time
- t tot, rEMG :
-
the respiratory cycle time of the rEMG
- V′ E :
-
minute ventilation
- V T :
-
tidal volume
References
Allen J, Zwerdling R, Ehrenkranz R, Gaultier C, Geggel R, Greenough A, Kleinman R, Klijanowicz A, Martinez F, Ozdemir A, Panitch HB, Nickerson B, Stein MT, Tomezsko J, Van Der AJ 2003 Statement on the care of the child with chronic lung disease of infancy and childhood. Am J Respir Crit Care Med 168: 356–396
Hjalmarson O, Sandberg K 2002 Abnormal lung function in healthy preterm infants. Am J Respir Crit Care Med 165: 83–87
Hülskamp G, Lum S, Stocks J, Wade A, Hoo AF, Costeloe K, Hawdon J, Deeptha K, Pillow JJ 2009 Association of prematurity, lung disease and body size with lung volume and ventilation inhomogeneity in unsedated neonates: a multicentre study. Thorax 64: 240–245
Latzin P, Roth S, Thamrin C, Hutten GJ, Pramana I, Kuehni CE, Casaulta C, Nelle M, Riedel T, Frey U 2009 Lung volume, breathing pattern and ventilation inhomogeneity in preterm and term infants. PLoS One 4: e4635
Hutten GJ, van Eykern LA, Latzin P, Kyburz M, van Aalderen WM, Frey U 2008 Relative impact of respiratory muscle activity on tidal flow and end expiratory volume in healthy neonates. Pediatr Pulmonol 43: 882–891
Bates JH, Schmalisch G, Filbrun D, Stocks J 2000 Tidal breath analysis for infant pulmonary function testing. ERS/ATS Task Force on Standards for Infant Respiratory Function Testing. European Respiratory Society/American Thoracic Society. Eur Respir J 16: 1180–1192
Jobe AH, Bancalari E 2001 Bronchopulmonary dysplasia. Am J Respir Crit Care Med 163: 1723–1729
Latzin P, Kuehni CE, Baldwin DN, Roiha HL, Casaulta C, Frey U 2006 Elevated exhaled nitric oxide in newborns of atopic mothers precedes respiratory symptoms. Am J Respir Crit Care Med 174: 1292–1298
Thamrin C, Latzin P, Sauteur L, Riedel T, Hall GL, Frey U 2007 Deadspace estimation from CO2 versus molar mass measurements in infants. Pediatr Pulmonol 42: 920–927
Frey U, Stocks J, Coates A, Sly P, Bates J 2000 Specifications for equipment used for infant pulmonary function testing. ERS/ATS Task Force on Standards for Infant Respiratory Function Testing. European Respiratory Society/American Thoracic Society. Eur Respir J 16: 731–740
Frey U, Stocks J, Sly P, Bates J 2000 Specification for signal processing and data handling used for infant pulmonary function testing. ERS/ATS Task Force on Standards for Infant Respiratory Function Testing. European Respiratory Society/American Thoracic Society. Eur Respir J 16: 1016–1022
Prechtl HF 1974 The behavioural states of the newborn infant [a review]. Brain Res 76: 185–212
Latzin P, Sauteur L, Thamrin C, Schibler A, Baldwin D, Hutten GJ, Kyburz M, Kraemer R, Riedel T, Frey U 2007 Optimized temperature and deadspace correction improve analysis of multiple breath washout measurements by ultrasonic flowmeter in infants. Pediatr Pulmonol 42: 888–897
Maarsingh EJ, van Eykern LA, Sprikkelman AB, Hoekstra MO, van Aalderen WM 2000 Respiratory muscle activity measured with a noninvasive EMG technique: technical aspects and reproducibility. J Appl Physiol 88: 1955–1961
Kosch PC, Stark AR 1984 Dynamic maintenance of end-expiratory lung volume in full-term infants. J Appl Physiol 57: 1126–1133
Lopes J, Muller NL, Bryan MH, Bryan AC 1981 Importance of inspiratory muscle tone in maintenance of FRC in the newborn. J Appl Physiol 51: 830–834
Mortola JP, Fisher JT, Smith B, Fox G, Weeks S 1982 Dynamics of breathing in infants. J Appl Physiol 52: 1209–1215
Kosch PC, Davenport PW, Wozniak JA, Stark AR 1985 Reflex control of expiratory duration in newborn infants. J Appl Physiol 58: 575–581
Kosch PC, Davenport PW, Wozniak JA, Stark AR 1986 Reflex control of inspiratory duration in newborn infants. J Appl Physiol 60: 2007–2014
Richter DW 1982 Generation and maintenance of the respiratory rhythm. J Exp Biol 100: 93–107
Cernelc M, Suki B, Reinmann B, Hall GL, Frey U 2002 Correlation properties of tidal volume and end-tidal O2 and CO2 concentrations in healthy infants. J Appl Physiol 92: 1817–1827
Frey U, Brodbeck T, Majumdar A, Taylor DR, Town GI, Silverman M, Suki B 2005 Risk of severe asthma episodes predicted from fluctuation analysis of airway function. Nature 438: 667–670
Suki B, Alencar AM, Sujeer MK, Lutchen KR, Collins JJ, Andrade JS Jr, Ingenito EP, Zapperi S, Stanley HE 1998 Life-support system benefits from noise. Nature 393: 127–128
Powers SK, Kavazis AN, Levine S 2009 Prolonged mechanical ventilation alters diaphragmatic structure and function. Crit Care Med 37: S347–S353.
Sassoon CS, Caiozzo VJ 2009 Bench-to-bedside review: diaphragm muscle function in disuse and acute high-dose corticosteroid treatment. Crit Care 13: 221
Baraldi E, Filippone M 2007 Chronic lung disease after premature birth. N Engl J Med 357: 1946–1955
Vrijlandt EJ, Gerritsen J, Boezen HM, Grevink RG, Duiverman EJ 2006 Lung function and exercise capacity in young adults born prematurely. Am J Respir Crit Care Med 173: 890–896
Vrijlandt EJ, Boezen HM, Gerritsen J, Stremmelaar EF, Duiverman EJ 2007 Respiratory health in prematurely born preschool children with and without bronchopulmonary dysplasia. J Pediatr 150: 256–261
Stegeman DF, Blok JH, Hermens HJ, Roeleveld K 2000 Surface EMG models: properties and applications. J Electromyogr Kinesiol 10: 313–326
Hutten J, van Eykern LA, Cobben JM, van Aalderen WM 2007 Cross talk of respiratory muscles It is possible to distinguish different muscle activity?. Respir Physiol Neurobiol 158: 1–2
Praud JP, Egreteau L, Benlabed M, Curzi-Dascalova L, Nedelcoux H, Gaultier C 1991 Abdominal muscle activity during CO2 rebreathing in sleeping neonates. J Appl Physiol 70: 1344–1350
Acknowledgements
We are grateful to Christine Becher, Monika Graf, Barbara Hofer, Gisela Wirz, and Sandra Lüscher for their help during lung function measurements. We also thank Matthias Nelle for help with patient recruitment.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by European Respiratory Society Fellowship Grant 221 and Dutch Asthma Foundation 05.032 (G.J.H.) and Swiss National Foundation Grant 3200-B0-112099 (U.F. and P.L.).
Rights and permissions
About this article
Cite this article
Hutten, G., van Eykern, L., Latzin, P. et al. Respiratory Muscle Activity Related to Flow and Lung Volume in Preterm Infants Compared With Term Infants. Pediatr Res 68, 339–343 (2010). https://doi.org/10.1203/PDR.0b013e3181eeeaf4
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3181eeeaf4
This article is cited by
-
Cardiorespiratory measures shortly after extubation and extubation outcomes in extremely preterm infants
Pediatric Research (2023)
-
Respiratory muscle function in the newborn: a narrative review
Pediatric Research (2022)
-
Diaphragmatic activity and neural breathing variability during a 5-min endotracheal continuous positive airway pressure trial in extremely preterm infants
Pediatric Research (2021)
-
Electromyographic activity of the sternocleidomastoid muscle in infants with bronchopulmonary dysplasia
Research on Biomedical Engineering (2021)