Abstract
In cystic fibrosis (CF), airway inflammation causes an increased production of reactive oxygen species, responsible for degradation of cell membranes. During this process, volatile organic compounds (VOCs) are formed. Measurement of VOCs in exhaled breath of CF patients may be useful for the assessment of airway inflammation. This study investigates whether “metabolomics' of VOCs could discriminate between CF and controls, and between CF patients with and without Pseudomonas colonization. One hundred five children (48 with CF, 57 controls) were included in this study. After exhaled breath collection, samples were transferred onto tubes containing active carbon to adsorb and stabilize VOCs. Samples were analyzed by gas chromatography-time of flight-mass spectrometry to assess VOC profiles. Analysis showed that 1099 VOCs had a prevalence of at least 7%. By using 22 VOCs, a 100% correct identification of CF patients and controls was possible. With 10 VOCs, 92% of the subjects were correctly classified. The reproducibility of VOC measurements with a 1-h interval was very good (match factor 0.90 ± 0.038). We conclude that metabolomics of VOCs in exhaled breath was possible in a reproducible way. This new technique was able to discriminate not only between CF patients and controls but also between CF patients with or without Pseudomonas colonization.
Similar content being viewed by others
Main
Airway inflammation plays a central role in the pathophysiology of various chronic lung diseases, such as cystic fibrosis (CF), asthma, and chronic obstructive pulmonary disease (COPD). Diagnosing CF is possible at any age, but it is far less simple to diagnose early pulmonary disease in CF patients, particularly in young children. It is known that there is a poor correlation between airway inflammatory processes and respiratory symptoms (1). Airway infection and inflammation can be present before clinical symptoms are evident. Thus, monitoring of airway inflammation/oxidative stress in CF may be useful in clinical practice.
There has been an increasing interest in noninvasive assessment of airway inflammation and oxidative stress in chronic lung disease. The collection of bronchoalveolar lavage (BAL) fluid or lung biopsies is invasive and, therefore, cannot be applied very easily in children. Noninvasive techniques include measurement of nonvolatile inflammatory markers in exhaled breath condensate and measurement of volatile inflammatory markers in exhaled breath. Fractional exhaled NO (FeNO), carbon monoxide (CO), ethane, and pentane are the most studied volatile markers (2,3), of which FeNO is most standardized (4). In contrast to assessments of preselected inflammatory markers, it is possible to assess profiles of volatile organic compounds (VOCs) in exhaled air.
An increased production of reactive oxygen species (ROS) is caused by the influx of leukocytes, which continuously produce ROS, leading to an imbalance between oxidants and antioxidants (oxidative stress) (5–8). ROS can degrade cell membranes by lipid peroxidation. During this process, VOCs are formed as a result of the degradation of polyunsaturated fatty acids. Endogenous VOCs can be divided into hydrocarbons-, oxygen-, or sulfur-containing compounds and nitrogen-containing substances (9).
Analysis of VOCs in exhaled air is possible by using a gas chromatography-time of flight-mass spectrometer (GC-TOF-MS). This technique is highly sensitive and capable of detecting a wide range of VOCs. A predictive model using nine VOCs was sufficiently sensitive and specific to be considered as a screening tool for lung cancer (10).
The aim of this study was to investigate whether metabolomics of VOCs in exhaled breath was able to discriminate between young subjects with CF and healthy controls and between subgroups of CF patients (with or without Pseudomonas colonization). It is well known that Pseudomonas colonization of the lung is associated with a less favorable prognosis of CF. The reproducibility of the method, as well as the nature and background of the most discriminating compounds, were studied.
METHODS AND MATERIALS
Subjects.
One hundred five subjects aged 5–25 y were included in this cross-sectional study: 48 subjects with a CF diagnosis and 57 control persons. The CF population was recruited from the outpatient clinic of the University Hospital Maastricht, the Netherlands. CF was defined as a combination of typical clinical features and an abnormal sweat test (chloride >60 mM). Children with CF and/or their parents completed the Shwachman-Kulczycki questionnaire, enabling classification of the CF disease status (11). The control group consisted of children without any (history of) respiratory problems, as confirmed by the ISAAC questionnaire (12). Thirty-six (63%) control children were recruited from primary schools, whereas 21 (37%) subjects were included at the outpatient clinic where enuresis nocturna and constipation were the initial reasons for consultation. At the moment of this study, these children were all stable with no signs of infection or any somatic disturbance. We checked the homogeneity of the control group by comparing children recruited from primary schools and outpatient clinic and found no significant differences in VOC patterns between these children (one-way ANOVA tests, p > 0.108). Exclusion criteria for both CF and control children were as follows: 1) patients with mental retardation; 2) active smokers; 3) (congenital) heart disease; 4) technical inability to perform the measurements; and 5) patients with an acute respiratory infection.
Informed consent to participate was obtained from the parents of all children participating in this study. The Ethics Committee of the Maastricht University approved this study. The clinical trial registration number is NCT 00413140.
Sampling.
Subjects were asked to exhale into a resistance-free polycarbonate (plastic) bag (Tedlar bag; SKC, Dorset, United Kingdom). Severe physical exercise before the test was not permitted. At least three exhalations were necessary to fill the 5-L bag. Within 1 h after collection of the sample, the bag was emptied over a stainless steel two-bed sorption tube, filled with carbograph 1 TD/Carbopack × (Markes International, Llantrisant, Wales, United Kingdom). Before and after loading, the tubes were airtight capped. The desorption tubes were stored at room temperature until analysis.
Analysis.
Analysis of the samples started with releasing the volatile compounds trapped on the sorption tubes by thermal desorption, using the Markes International Ultra-Unity automated thermal desorption (ATD) equipment (Markes International). The gaseous mixture of released compounds was then split; 90% of the sample was recollected on a second sorption tube and stored for a possible second analysis, 10% of the sample was loaded onto a cold sorption trap (5°C; Markes U-T2GPH: general purpose hydrophobic trap, designed for sampling VOC C4-C32), from which it was injected into a GC (Trace GC; ThermoFischer Scientific, Austin, TX) and analyzed by TOF mass spectrometry (Tempus Plus; ThermoFischer Scientific). For the GC-MS measurements, the following conditions were used: column: Restek RTX-5 ms, 30 m × 0.25 mm ID; helium was used as the carrier gas at a flow rate of 1.5 mL/min. Transferline temperature was 250°C. The temperature of the GC was programmed as follows: 40°C during 5 min, then raised with 10°C/min until a final maximum temperature of 270°C. In the final step, this temperature was maintained for 5 min. The MS was set as follows: ionizing energy 70 eV, source temperature 200°C at a scan of 5 Hz.
Data analysis.
The GC-MS chromatograms of the breath samples of the 105 subjects involved in this research were recorded and corrected for retention time differences, using retention indices and lining up of easily recognizable component peaks. Corrected retention times were based on 6–10 common components with high intensities (e.g., acetone, toluene, phenol, and benzene). The parts of the chromatograms that occurred at a retention index <0.15 and at a retention index >2.8 were removed from the chromatograms because of unreliable data from these parts as a result of noisy mass spectra at the beginning of the chromatograms and column bleeding at the end of the run. The resulting data files were carefully combined. This was done by means of combination of identical compounds from different samples. Compounds were combined based on similarity of mass spectra and retention times. This resulted in a final database file containing almost 6000 different chromatographic peaks. The total surface below the breathogram was set at 100%. The intensity of a specific VOC corresponds with the surface below that peak. The resulting database was used for statistical analysis.
Data mining.
To determine which compounds were of interest with regard to the classification of CF patients and controls, we used stepwise discriminant analysis, using SPSS (SPSS, Chicago, IL). An attribute (VOC) was only included in the discriminant analysis if its prevalence was 7% or more within the study population. Discriminant analysis was assessed with the grouping variables “diagnosis” (CF, n = 48; controls, n = 57), and “positive Pseudomonas aeruginosa cultures” (yes, n = 23; no, n = 17). To exclude bias by different CF treatments (use of an antibiotic, a corticosteroid, or DNase), VOC patterns of patients with or without this treatment were compared. The homogeneity of the control group was assessed by comparing VOC patterns between children selected at the primary school and the subjects recruited at the outpatient clinic. The quantification of the similarity between the VOC profiles was done by means of calculation of a “distance measure” (dot product rule) or match factor, as been described in detail by Stein and Scott (13). This distance measure is based on the similarity of the entire raw chromatogram. A value of “1” denotes identical samples, the lower the value the lesser the degree of similarity. Values of 0.8 and more can be characterized as very good agreement (13).
Lung function tests.
Lung function tests were performed after exhaled breath sampling. Bronchodilator medication was stopped before lung function testing: short-acting bronchodilators at least 8 h before, and long-acting bronchodilators at least 36 h before the test. Dynamic spirometry was performed by means of a pneumotachograph (Flowscreen; Viasys, Hoechberg, Germany), with measurement of forced expiratory volume in 1 s (FEV1) and forced vital capacity (FVC), according to the standards of the European Respiratory Society (14). The highest values of FEV1 and FVC of three forced expiratory maneuvers were used for data analysis. In CF patients, the bronchodilating response was assessed 15 min after administration of a short-acting bronchodilator [salbutamol (400 μg] and expressed as the increase in FEV1 compared with the predicted value of FEV1. In addition, in the CF population, static lung volumes, residual volume (RV), intrathoracic gas volume (ITGV), and total lung capacity (TLC), were assessed by body plethysmography (Viasys).
Statistical analysis.
All data are expressed as mean ± SE. A normal distribution was present for all patient characteristics. Therefore, two-sided independent-sample t tests were used for the analysis of the subject characteristics; p-values of <0.05 were considered statistically significant. To analyze the VOC profiles, 10 times cross-validation with multiple discriminant analysis was used to minimize type III errors (15). Of 10 subsamples, 9 subsamples are used as a training set, and the remaining single subsample was used to test the model (validation set). The cross-validation process was repeated 10 times, with each of the 10 subsamples used once as the validation data. The 10 results were averaged to produce a single estimation.
Discriminant analysis was applied to the following: 1) investigate differences among groups; 2) determine the most parsimonious way to distinguish among groups; 3) discard variables that are of little interest related to group distinctions; 4) classify cases into groups; and 5) test theory by observing whether cases are classified as predicted.
Reproducibility and influence of breathing pattern.
The influence of the breathing pattern (unforced breathing pattern vs hyperventilation) on VOC profiles and the variation in VOCs across the day and between days was analyzed in 15 healthy control children aged 5–15 y (mean ± SD, 15.5 ± 3 y). Sampling of VOCs was applied during an unforced breathing pattern (conform the entire study population), during hyperventilation, after 1 h, and after 1 d.
Power analysis.
We assume a minimal sensitivity of at least 70% for a potentially valuable inflammatory marker. The SE of the sensitivity and the specificity of an inflammatory marker will be less than 5% when 100 children (50 children with CF and 50 controls) are recruited for this study.
RESULTS
Population characteristics.
Subjects with CF were characterized by a light to moderate airway obstruction, air trapping, and a mild restrictive impairment in comparison with controls (Tables 1 and 2). In the CF group, 49% of subjects had positive cultures with P. aeruginosa in the past 2 y, and 8 persons (17%) showed a history of allergic bronchopulmonary aspergillosis (ABPA). The mean ± SE time between sputum collection and breath sample collection was 50 ± 62 d. Patients were mainly treated with antibiotics, antacids, DNase, and corticosteroids (Table 2).
Exhaled breath collection.
All subjects completed the maneuver correctly. No adverse effects were reported during the exhaled breath collection.
VOC profiles.
Approximately 6000 different VOCs were identified in the chromatograms of the entire study population (Fig. 1). After selection of attributes with a prevalence of at least 7%, 1099 VOCs were included in the analysis (16).
Variation across the day and between the days.
Distance measure calculation of all complementary files within 1 h resulted in a mean ± SD match factor of 0.90 ± 0.038. Similarity of VOC profiles after 1 d was 0.85 ± 0.096. These data indicate a low within-subject variation in VOC patterns after 1 h and after a day.
Influence of breathing patterns.
Samples were assessed with an unforced breathing pattern and during hyperventilation. Characteristics are shown in Table 3. The match factor (mean ± SD) of these breathing patterns was 0.95 ± 0.043, which indicates minimal influence of breathing pattern on VOC profiles.
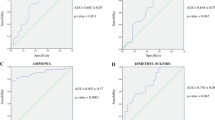
Discriminant analysis: diagnosis of CF.
It was possible to assess distinctive VOC profiles, which discriminated between CF children and controls. Based on 10 times cross-validation, a 100% correct classification of CF patients and controls was found using 22 attributes or more (Figs. 2 and 3). The sensitivity, specificity, and percentage of correct classification increased with increasing attributes in the analysis. The specificity of the models with 1–26 attributes ranged from 91 to 100%, with a corresponding sensitivity of 58–100%. Identification of the 10 most important discriminating VOCs was possible in all cases (Table 4). Six of these VOCs were classified as hydrocarbons with 4–16 carbon atoms. Figure 4 shows the mean relative intensity of the 10 most prominent attributes, which discriminated children with CF from healthy controls. All attributes were not significantly different between CF children with of without the use of antibiotics, corticosteroids, and DNase use (p > 0.130, one-way ANOVA). In the control group, there was no significant difference in between the subjects recruited from the primary school or the children from the outpatient clinic with initial complaints of constipation or enuresis nocturna.
The percentage of correct classification of CF with increasing numbers of attributes using discriminant analysis. The discriminant analysis was performed using 10 times cross-validation. An attribute was only included in the analysis if its prevalence was 7% or more within the study population. This figure shows a 100% correct classification of CF patients and controls with use of 22 attributes or more. The sensitivity of the models assessed with 1–26 attributes ranged from 58 to 100% (⋄). The specificity of these models ranged from 91 to 100% (▪).
As acquisition of P. aeruginosa in the sputum is associated with increased morbidity and mortality, we were interested in VOC profiles of CF subjects with and without positive cultures of Pseudomonas. Within the CF group, it was possible to identify patients with or without positive P. aeruginosa cultures 100% correctly by means of 14 VOCs in exhaled breath (Fig. 5).
The percentage of correct classification of positive or negative Pseudomonas aeruginosa cultures in sputum of CF patients with increasing numbers of attributes using discriminant analysis. The discriminant analysis was performed using 10 times cross-validation. This figure shows a 100% correct classification of CF patients with and without positive Pseudomonas aeruginosa cultures in sputum with use of 14 attributes or more. The sensitivity (⋄) of the models assessed with 1–24 attributes ranged from 34 to 100%; the specificity ranged from 29 to 100% (▪).
DISCUSSION
This study showed that metabolomics of VOCs in exhaled breath of young subjects with CF and healthy controls was possible in a reproducible way, resulting in a 100% correct classification rate by using 22 compounds. Moreover, it was possible to discriminate between CF patients with or without positive P. aeruginosa cultures, a factor which is clearly associated with CF prognosis. The discrimination between CF and controls was mainly based on C5–C16 hydrocarbons and N-methyl-2-methylpropylamine. This study showed good feasibility of exhaled breath collection in 5-L Tedlar bags in children of 5 y and older. More than 1000 different VOCs could be measured in exhaled breath of CF patients and controls with prevalence in the two groups of at least 7%, with good short-term and long-term reproducibility. Breathing patterns did not influence VOC profiles significantly. The match factor, based on a distance measure implementing the dot product rule, was applied to establish the degree of similarity between measured chromatograms (13,17).
We acknowledge some limitations in this study: Variance of data are influenced by a large range of patient-related and technical factors, therefore, there should be some caution in identifying biomarkers. It is of great importance to correct for the selection bias. Ambroise and McLachlan described how selection bias can be assessed and corrected. They recommend 10-fold rather than leave-one-out cross-validation to handle overestimation of the results. Therefore, 10-fold cross-validation was applied in our study (17). Although 10 times cross-validation is a valid method to prevent overestimation of the predictive value of markers, external validation in a control population of patients and controls is necessary in a second stage to further validate the results. The control group in this study was significantly younger that the CF group. This probably did not bias our results as no significant influence of age was found in the discriminant analysis.
As reported previously by van Berkel et al. (18), we did not correct our measurements for chemical background appearing in the samples. This is because of the fact that it will not be possible to correct for the complex interdependencies between excretion and uptake of VOCs by easily subtracting the inhaled from the exhaled air. Moreover, background noise will be randomly distributed between subjects' samples and would, thus, neither exert any discriminatory power nor interfere with the outcome of the analyses. We are aiming with discriminative analysis to select only those compounds that are specific for the disease or condition and should, thus, principally not depend on background chemicals.
In the past few years, there has been increasingly interest in presence of VOCs in exhaled breath of patients with chronic lung diseases. Phillips et al. (10,19) assessed VOCs in exhaled air by means of ATD-GC-MS and classified patients with and without lung cancer, based on 9–22 VOCs. In addition, they studied the potential of VOCs to differentiate between 42 patients with a suspicion of pulmonary tuberculosis and 59 controls, and tuberculosis patients with and without bacterial sputum colonization. These classifications were possible with high sensitivity and specificity (20).
In 2006, Barker et al. (21) studied 12 specific VOCs by means of a customized GC in CF patients and controls. They reported a significant lower level of dimethyl sulfide (DMS) in CF patients compared with controls. However, DMS was not identified as an important discriminating component in this study. Other methods to measure VOCs are sensor systems such as the electronic nose, based on chemical vapor arrays responding to VOCs, and colorimetric sensor arrays. These methods were applied to detect lung cancer (22,23). In contrast to VOC assessment with GC-TOF-MS, the electronic nose consists of a nano-composite array of 32 organic polymer sensors. This is a limitation as the significance of specific VOCs for specific lung diseases is not established yet. First, it is important to specify the VOCs important for a specific disease or a specific question (VOCs important for diagnosis may not be the same ones that appear to be important for disease monitoring). In a second stage, when the relevant VOCs are defined, sensor systems such as the electronic nose might be very helpful, as they are rapid, easy to use, and not very expensive.
Currently, diagnosis of pulmonary CF exacerbations and monitoring of disease activity are mainly based on clinical features and lung function tests. These parameters reflect changes in the functional abnormalities in the airways by infective and inflammatory processes, instead of the inflammation itself (24). Therefore, inflammation may be present before clinical parameters change, introducing a time delay between the onset of a pulmonary CF exacerbation and the start of treatment. Persistent inflammation and repeated cycles of infection are present in CF lungs, resulting in progressive lung damage and pulmonary fibrosis (25). Even in stable patients, chronic airway inflammation is present, as reflected by high airway fluid concentrations of proinflammatory cytokines (26). Analysis of BAL fluid has shown a 1.000-fold increase in the number of neutrophils from the lungs of patients with CF compared with controls (27).
We hypothesize that VOC profiles may be helpful in the early detection of a CF exacerbation even before symptoms occur and lung function deterioration is present and the decision to stop antibiotic treatment in patients recovering from an exacerbation. However, this should be the subject of future longitudinal studies. Based on this study, metabolomics of VOCs in exhaled breath discriminate between CF patients and controls. Dallinga et al. and Dragonieri et al. showed that VOCs could discriminate between children and adults with asthma and healthy controls (5,6). In addition, Fens et al. showed good discrimination between asthmatics and patients with chronic pulmonary obstructive disease by means of the electronic nose (8). Therefore, the hypothesis is that these markers may be of additional value to study ongoing processes of airway inflammation and oxidative stress, in addition to lung function and symptoms. As we were interested in the earliest stages of CF lung disease, the CF population of our study had mild to moderately severe pulmonary CF disease. It is not clear whether the results of this study can be generalized to more severe CF. This study showed good feasibility and safety of VOC collection in children. This is an advantage when compared with invasive methods like biopsies, BAL, and induced sputum. The short-term reproducibility of VOCs was excellent. We expect an even higher reproducibility of a typical VOC pattern, because not only the absolute values but also the values of the spikes relative to each other are important for the reproducibility of a specific pattern. However, this will be the subject of future studies. The objective of this study was to identify VOC profiles of CF disease and control children and to specify which VOCs are important in CF. In our study, products of inhaled medication or their derivatives, such as tobramycin or corticosteroids, were not recovered in exhaled breath and, therefore, did not contribute to the discrimination.
By means of VOC profiles, we were able to differentiate between CF patients with or without positive cultures for P. aeruginosa. This result was consistent, although other microorganisms may be concordantly present in the airways of patients, and a certain time period between collection of sputum samples and the sampling of VOCs was present in some subjects.
Future research on VOCs in exhaled breath should be focused not only on clinical questions but also on methodological issues such as the influence of diet and exercise on VOCs. In addition, VOC profiles should be studied in longitudinal studies to investigate the additional value of VOC measurements to conventional parameters such as symptoms, lung function indices, and sputum analyses. Assessment of VOCs in exhaled breath is a new, promising, noninvasive technique, which, in addition to conventional parameters, can be used to study airway inflammation and oxidative stress in CF patients.
Abbreviations
- CF:
-
cystic fibrosis
- FEV1:
-
forced expiratory volume in 1 second
- GC:
-
gas chromatography
- MS:
-
mass spectrometer
- ROS:
-
reactive oxygen species
- TOF:
-
time of flight
- VOCs:
-
volatile organic compounds
References
Gibson RL, Burns JL, Ramsey BW 2003 Pathophysiology and management of pulmonary infections in cystic fibrosis. Am J Respir Crit Care Med 168: 918–951
Paredi P, Kharitonov SA, Barnes PJ 2000 Elevation of exhaled ethane concentration in asthma. Am J Respir Crit Care Med 162: 1450–1454
Horvath I, MacNee W, Kelly FJ, Dekhuijzen PN, Phillips M, Doring G, Choi AM, Yamaya M, Bach FH, Willis D, Donnelly LE, Chung KF, Barnes PJ 2001 “Haemoxygenase-1 induction and exhaled markers of oxidative stress in lung diseases,” summary of the ERS Research Seminar in Budapest, Hungary, September 1999. Eur Respir J 18: 420–430
American Thoracic Society; European Respiratory Society 2005 ATS/ERS Recommendations for standardized procedures for the online and offline measurement of exhaled lower respiratory nitric oxide and nasal nitric oxide, 2005. Am J Respir Crit Care Med 171: 912–930.
Dallinga JW, Robroeks CM, van Berkel JJ, Moonen EJ, Godschalk RW, Jöbsis Q, Dompeling E, Wouters EF, van Schooten FJ 2010 Volatile organic compounds in exhaled breath as a diagnostic tool for asthma in children. Clin Exp Allergy 40: 68–76
Fens N, Zwinderman AH, van der Schee MP, de Nijs SB, Dijkers E, Roldaan AC, Cheung D, Bel EH, Sterk PJ 2009 Exhaled breath profiling enables discrimination of chronic obstructive pulmonary disease and asthma. Am J Respir Crit Care Med 180: 1076–1082
Delfino RJ, Gong H, Linn WS, Hu Y, Pellizzari ED 2003 Respiratory symptoms and peak expiratory flow in children with asthma in relation to volatile organic compounds in exhaled breath and ambient air. J Expo Anal Environ Epidemiol 13: 348–363
Dragonieri S, Schot R, Mertens BJ, Le Cessie S, Gauw SA, Spanevello A, Resta O, Willard NP, Vink TJ, Rabe KF, Bel EH, Sterk PJ 2007 An electronic nose in the discrimination of patients with asthma and controls. J Allergy Clin Immunol 120: 856–862
Miekisch W, Schubert JK, Noeldge-Schomburg GF 2004 Diagnostic potential of breath analysis—focus on volatile organic compounds. Clin Chim Acta 347: 25–39
Phillips M, Cataneo RN, Cummin AR, Gagliardi AJ, Gleeson K, Greenberg J, Maxfield RA, Rom WN 2003 Detection of lung cancer with volatile markers in the breath. Chest 123: 2115–2123
Shwachman H, Kulczycki LL 1958 Long-term study of one hundred five patients with cystic fibrosis; studies made over a five- to fourteen-year period. AMA J Dis Child 96: 6–15
Burney P, Chinn S, Jarvis D, Luczynska C, Lai E, on behalf of the European Community Respiratory Health Survey 1996 Variations in the prevalence of respiratory symptoms, self-reported asthma attacks, and use of asthma medication in the European Community Respiratory Health Survey (ECRHS). Eur Respir J 9: 687–695
Stein SE, Scott DR 1994 Optimization and testing of mass-spectral library search algorithms for compound identification. J Am Soc Mass Spectrom 5: 859–866
Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC 1993 Lung volumes and forced ventilatory flows. Report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur Respir J ( suppl 16): 5–40
Edwards TL, Torstensen E, Dudek S, Martin ER, Ritchie MD 2010 A cross-validation procedure for general pedigrees and matched odds ratio fitness metric implemented for the multifactor dimensionality reduction pedigree disequilibrium test. Genet Epidemiol 34: 194–199
Penn DJ, Oberzaucher E, Grammer K, Fischer G, Soini HA, Wiesler D, Novotny MV, Dixon SJ, Xu Y, Brereton RG 2007 Individual and gender fingerprints in human body odour. J R Soc Interface 4: 331–340
Ambroise C, McLachlan GJ 2002 Selection bias in gene extraction on the basis of microarray gene-expression data. Proc Natl Acad Sci USA 99: 6562–6566
van Berkel JJ, Dallinga JW, Moller GM, Godschalk RW, Moonen E, Wouters EF, van Schooten FJ 2008 Development of accurate classification method based on the analysis of volatile organic compounds from human exhaled air. J Chromatogr B Analyt Technol Biomed Life Sci 861: 101–107
Phillips M, Gleeson K, Hughes JM, Greenberg J, Cataneo RN, Baker L, McVay WP 1999 Volatile organic compounds in breath as markers of lung cancer: a cross-sectional study. Lancet 353: 1930–1933
Phillips M, Cataneo RN, Condos R, Ring Erickson GA, Greenberg J, La Bombardi V, Munawar MI, Tietje O 2007 Volatile biomarkers of pulmonary tuberculosis in the breath. Tuberculosis (Edinb) 87: 44–52
Barker M, Hengst M, Schmid J, Buers HJ, Mittermaier B, Klemp D, Koppmann R 2006 Volatile organic compounds in the exhaled breath of young patients with cystic fibrosis. Eur Respir J 27: 929–936
Machado RF, Laskowski D, Deffenderfer O, Burch T, Zheng S, Mazzone PJ, Mekhail T, Jennings C, Stoller JK, Pyle J, Duncan J, Dweik RA, Erzurum SC 2005 Detection of lung cancer by sensor array analyses of exhaled breath. Am J Respir Crit Care Med 171: 1286–1291
Mazzone PJ, Hammel J, Dweik R, Na J, Czich C, Laskowski D, Mekhail T 2007 Diagnosis of lung cancer by the analysis of exhaled breath with a colorimetric sensor array. Thorax 62: 565–568
Kharitonov SA, Barnes PJ 2001 Exhaled markers of pulmonary disease. Am J Respir Crit Care Med 163: 1693–1722
McGrath LT, Mallon P, Dowey L, Silke B, McClean E, McDonnell M, Devine A, Copeland S, Elborn S 1999 Oxidative stress during acute respiratory exacerbations in cystic fibrosis. Thorax 54: 518–523
Grasemann H, Ioannidis I, Tomkiewicz RP, de Groot H, Rubin BK, Ratjen F 1998 Nitric oxide metabolites in cystic fibrosis lung disease. Arch Dis Child 78: 49–53
Brown RK, Wyatt H, Price JF, Kelly FJ 1996 Pulmonary dysfunction in cystic fibrosis is associated with oxidative stress. Eur Respir J 9: 334–339
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported with an unrestricted grant of AstraZeneca.
Rights and permissions
About this article
Cite this article
Robroeks, C., van Berkel, J., Dallinga, J. et al. Metabolomics of Volatile Organic Compounds in Cystic Fibrosis Patients and Controls. Pediatr Res 68, 75–80 (2010). https://doi.org/10.1203/PDR.0b013e3181df4ea0
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3181df4ea0
This article is cited by
-
Exhaled volatile organic compounds analysis in clinical pediatrics: a systematic review
Pediatric Research (2021)
-
Breath metabolome of mice infected with Pseudomonas aeruginosa
Metabolomics (2019)
-
Metabolomic studies of Pseudomonas aeruginosa
World Journal of Microbiology and Biotechnology (2019)
-
Volatile molecules from bronchoalveolar lavage fluid can ‘rule-in’ Pseudomonas aeruginosa and ‘rule-out’ Staphylococcus aureus infections in cystic fibrosis patients
Scientific Reports (2018)
-
Exhaled breath analysis: a review of ‘breath-taking’ methods for off-line analysis
Metabolomics (2017)