Abstract
Magnetic resonance imaging studies have contributed to recognize the patterns of cerebral injury related to neonatal encephalopathy (NE). We assessed whether a smaller corpus callosum (CC) explained the difference in motor performance between school-age children with NE and controls. Frontal, middle, and posterior areas of the CC were measured in 61 9–10-y-old children with NE and in 47 controls. Motor performance was determined using the Movement Assessment Battery for Children (M-ABC). Linear regression was used to assess whether differences in M-ABC between NE children and controls could be explained by CC size. The CC of 11/30 children with NE type I according to Sarnat (NE I) and 19/36 children with NE type II according to Sarnat (NE II) showed generalized or focal thinning, compared with 8/49 controls. Children with NE II had significantly smaller middle and posterior parts and total areas of the CC. Children with NE scored significantly worse on the M-ABC than controls. The reduction in size of the posterior part of the CC partly explained the mean differences on the M-ABC. Children with NE have poorer motor skills than controls, which is partly explained by a smaller size of the CC.
Similar content being viewed by others
Main
Neonatal encephalopathy (NE) related to perinatal asphyxia has a prevalence of 1–6/1000 live-born, full-term infants (1). Long-term follow-up data of neurodevelopmental outcome are still scarce but have shown significantly more problems at school age in children with moderate NE (NE II) according to the criteria of Sarnat (2) compared with children with mild NE according to the criteria of Sarnat (NE I) and matched controls (3–6). Magnetic resonance imaging (MRI) studies have made a major contribution to recognize the different patterns of NE-related cerebral lesions, which have been shown to be predictive of long-term neurodevelopmental outcome (7–10).
The corpus callosum (CC) links associative areas of the two cerebral hemispheres. The genu of the CC is formed between 8 and 13 wk of gestation. After 20 wk gestational age the total CC is formed (11). The CC is among the last structures to be completed during postnatal maturation. Its size increases with age until early adulthood because of the ongoing myelinization process, which begins to appear at about 4 mo of age in the splenium and at 6 mo in the genu (12,13). Due to its longer myelogenetic cycle, the CC is vulnerable to hemorrhage and ischemia (14). Fibers from the frontal lobe and the anterior part of the parietal lobe course through the rostrum and genu of the CC. Fibers from the temporal, posterior part of the parietal and occipital lobe are carried in the caudal portion of the body of the CC and in the splenium (14,15).
Several studies have shown a relation between the CC size and motor outcome in preterm infants (16–18). Maneru et al. (19) demonstrated that the CC was smaller in adolescents who suffered from moderate asphyxia than in controls. The CC measurements correlated with neuropsychological performance.
In the present study, we assessed the difference in motor performance between school-age children with NE and controls, and whether the size of the CC could partly explain this difference.
PATIENTS AND METHODS
Patients.
Between 1993 and 1996, 129 children with NE I or II were admitted to the Neonatal Intensive Care Unit of the Wilhelmina Children's Hospital. Children who developed NE during the first few days of life and fulfilled at least three of the following criteria during the perinatal period were enrolled in a long-term follow-up study: 1) late decelerations on fetal monitoring or meconium staining, 2) delayed onset of respiration, 3) arterial cord blood pH less than 7.10, 4) Apgar score less than 6 at 5 min, and 5) multi-organ failure (20).
Of the total cohort, 26 children (20.2%) died in the neonatal period. During follow-up, 12 children (9.3%) developed cerebral palsy (CP). All children with CP had NE II. Six of these children were too severely affected to be able to participate in the study. Of the remaining 97 children, 8 (8.2%; NE I: 4; NE II: 4) could not be traced due to moving, and the parents of 18 (NE I: 11; NE II: 7) children (18.6%) refused to participate. Finally, 71 of the 97 children (73.2%) were included in the study, and 6 of these (8.5%) had CP. There were no significant differences in GA, BW, gender, and Sarnat classification between the included children and the nonparticipants.
All survivors were seen in the follow-up clinic up to 18 mo of age and only beyond when they showed an abnormal neurologic outcome. At the age of 9 or 10 y, all children were invited to the hospital for neurodevelopmental assessment.
The control children were partly recruited from the same schools as the children with NE and partly from other schools in the same region. All controls were matched for age and gender. Children born preterm, born by assisted instrumental delivery, or with any complications known to be associated with developmental delays (admission to the neonatal unit, congenital or acquired chronic illness, or malformations of the CNS) were excluded.
Informed parental consent was obtained for the MRI examination. The study was approved by the Medical Ethical Committee of the University Medical Center Utrecht.
Brain imaging.
The children were imaged on a 1.5-Tesla Philips ACS-NT system (Philips Medical Systems, Best, the Netherlands). Midsagittal T1 SE images were used for the present study (2D image, FoV 250 × 250 mm, matrix 256 × 256, pixel size 0.98 × 0.98 mm, TR 515 ms, TE 15.00 ms, gap 0.6 mm, slice thickness 4 mm). The MRI was performed without sedation. The children had eye contact with a parent, using a mirror placed above their head, and they could listen to their favorite music during the examination. Sixty-six of the 71 children with NE had an MRI. Five children were too anxious to cooperate (two with NE I and three with NE II, including one child with CP). In the group of 50 controls, one MRI could not be obtained due to claustrophobia.
CC measurements.
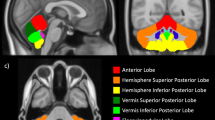
The shape of the CC was assessed visually by a pediatric radiologist (R.A.J.N.) classifying them as having a normal shape (Fig. 1A), focal (anterior, middle, and posterior), or generalized thinning (Fig. 1B). The MRI data were transferred in digital format to an Easy Vision Workstation. All measurements were analyzed by one examiner (B.J.M.K.), who was blinded to the results of the Movement Assessment Battery for Children (M-ABC). The images were first enlarged to an extent at which the contour of the CC could be easily manually traced with a mouse-controlled cursor. A natural incurvation is present near the level of the genu and the splenium. One centimeter from this incurvation, a line was drawn perpendicular to the contour and to the middle of the CC (Fig. 2). The different parts of the CC (anterior, middle, and posterior) were identified and the areas (mm2) were measured separately. The total area of the CC was the sum of these different parts. In a similar way, the midsagittal cerebral size (MCS), not including the cerebellum was measured to allow for adjustment for brain size.
Whalley et al. (21) have shown there is a good correlation between the size of the CC expressed as its cross-sectional area and its volume. Therefore, the two-dimensional measurement of the CC on the midline sagittal image is considered to estimate its real volume.
All cases were measured twice to assess intraobserver variability of the measurements. A mean difference between 2.9% and 3.4% was found for the two measurements of each of the subregions and of 1.9% for the total area, similar to data reported by Rauch and Jinkins (22).
Motor function.
All children were seen at the age of 9 or 10 y by a psychologist (M.H.) who was blinded to the MRI data and to the data from the neonatal period. Motor function was assessed using the M-ABC band 3 for age 9 and 10 y (23).
The test consists of three domains: manual dexterity (shifting pegs, screw nuts on a bolt, and drawing a flower trail), ball skills (catch with two hands and throw beanbag into box), and static and dynamic balance (balance on a board, hop into squares, and balance a ball). Items in each domain are scored between 0 (best score) and 5 (worst score), with a maximum score of 15 for manual skills, 10 for ball skills, and 15 for static and dynamic balance. The total impairment score (TIS) is the sum of the subscores. The scores are converted to percentile (P) scores and these are classified as follows: abnormal ≤P5; borderline P6–P15; normal >P15.
Cognitive tests were also performed. The results of these assessments will be reported separately.
Data analysis.
For descriptive purposes, group-specific means (standard deviation: SD) and proportions were calculated.
Proportional data on the associations between shape of the CC and disease status were tested using χ2 tests. With the one-way ANOVA test, the mean group differences in CC size were assessed. To correct for multiple comparisons, Tukey HSD was used as a post hoc multiple comparisons test.
Linear regression analysis was used to assess mean differences in (components of) M-ABC scores between children with NE and controls. These models were also used to evaluate whether these differences could be explained by group differences in CC area. All linear regression models were also used to adjust for the possible confounders: gender, age, and MCS. SPSS version 12.0 (SPSS Inc., Chicago, IL) was used for all analyses. Confidence intervals not including 0 (p < 0.05) were considered statistically significant.
RESULTS
Clinical findings.
Of the 71 children, 32 (45.1%) children had NE I and 39 (54.9%) children NE II. The mean gestational age (GA) was 40.29 wk (SD 1.43) and the mean birth weight (BW) was 3441 g (SD 582). There were 37 (52.1%) boys and 34 (47.9%) girls (Table 1).
At the time of the assessments, the children had a mean age of 118 mo (SD 6). Fifteen children (21.1%) attended schools for special education.
The reference group consisted of 50 children with a mean age of 120 mo (SD 6). All children were in mainstream education. Their mean GA was 40.00 wk (SD 1.29) and their mean BW 3514 g (SD 471 g) (Table 1).
MRI findings.
On visual analysis of the thickness of the CC, 11/30 (36.7%) children with NE I and 19/36 (52.8%) children with NE II had an abnormal shape. The abnormal shape in children with NE I consisted of generalized thinning in 1 (3.3%) and of focal thinning in 10 (33.3%) children. In the group with NE II, 4 (11.1%) children showed generalized thinning and 15 (41.7%) had focal thinning. In both groups, focal thinning most commonly involved the middle part of the CC (Table 2).
Eight of 49 (16.3%) controls had an abnormal shape of the CC; 1 (2.0%) had anterior thinning and 7 (14.3%) thinning of the middle part.
The CC size could be reliably measured in 61 children with NE and 47 control children, due to motion artefacts in 5 children with NE and in 2 controls.
Table 2 shows the absolute areas of the different CC parts, the mean area of the MCS and the CC/MCS ratio. Children with NE II showed significantly smaller middle, posterior, and total areas of the CC compared with the controls (respectively, p = 0.011, p < 0.001, and p = 0.003). There was no significant difference between children with NE I and both controls (respectively, p = 0.740, p = 0.157, and p = 0.257) and children with NE II (respectively, p = 0.130, p = 0.107, and p = 0.260).
Table 3 shows the mean differences of the CC measurements between the children with NE II and the controls. Age, gender, and MCS could affect the size of the CC. However, adjustment for these confounders did not change the findings.
Few other abnormalities were seen on the MRI of the children with NE. Detailed results of brain imaging findings will be reported separately. The children with CP showed focal or more diffuse other lesions as well. These children were excluded from the analyses.
M-ABC.
The mean scores for the M-ABC are shown in Table 4. In the children with NE, the TIS of two children who could not cooperate were missing. The six children with CP were excluded, because the M-ABC is not suitable to test their general movement abilities. In the group of children with NE I, 9 children (29.0%) had a TIS below or at the 5th percentile (abnormal), 9 (29.0%) scored between the 6th and 15th percentile (borderline), and 13 children (41.9%) scored above the 15th percentile (normal). Twelve (37.5%) children with NE II had an abnormal score, 9 (28.1%) scored borderline, and 11 children (34.4%) had a normal score. Seven (14.0%) controls had an abnormal score, 10 (20.0%) scored borderline, and 33 (66.0%) had a normal score. The differences in the TIS between controls and both children with NE I and NE II were significant. The TIS of children with NE I did not differ significantly from children with NE II (not shown).
Association between M-ABC, CC area, and neonatal encephalopathy.
The children with CP were excluded from the analysis to assess the association between the M-ABC and the CC area.
We aimed to show whether differences in (components of) the M-ABC and CC size between children with NE and controls were interrelated. Figure 3 illustrates that a smaller posterior part of the CC is related to a higher TIS on the M-ABC in children with NE. The regression coefficient of the line in this figure was –0.05. No data were available of the measurements of the CC of three out of six children with a TIS above 20.0 (one did not have a MRI, the others had moved too much to reliably measure the CC).
Table 5 shows the mean differences in M-ABC scores between NE children and controls both before and after adjustment for the size of the posterior part of the CC. Before adjustment, the TIS of all children with NE was significantly higher than in controls, indicating poorer motor skills. The mean TIS of children with NE was 4.2 points higher than the mean TIS of the controls (Table 5, second column). With adjusting for the size of the CC, the mean differences in M-ABC scores can be assessed without the effect of the CC size on the score. After adjustment, the mean differences decreased and became less significant, indicating that the size of this part of the CC partly explained the differences in M-ABC scores between NE children and controls. For example, the difference in mean TIS between all children with NE and the controls decreased from 4.2 to 2.8 (Table 5, fourth column). The mean differences of the subdomains manual dexterity, ball skills, and static and dynamic balance between children with NE and controls were also significant, but the latter two were only significant in children with NE II. Again, the posterior part of the CC partly explained these differences. In addition, the total area of the CC partly explained the differences of (components of) the M-ABC, although less pronounced (not shown).
DISCUSSION
In the present study, poorer motor skills were found in children with NE compared with controls. A smaller size of the CC, particularly the posterior part, partly explained these findings.
Maneru et al. (19) found the CC to be smaller in adolescents who were born at term and suffered moderate perinatal asphyxia. They measured the CC in 6 patients with NE I and in 15 patients with NE II. The CC was automatically delineated by means of the intensity threshold routine from the ANALYZE program and corrected manually. The CC was divided in seven parts by using the analysis described in Witelson (24). They reported atrophy of the genu and of the isthmus region to be more common in the NE II group compared with the control group. There were no significant differences between the NE I group and controls. In our study, the middle and posterior part of the CC were reduced in size. The isthmus region described by Maneru is situated at the border of our middle and posterior part of the CC. In contrast to Maneru's data, we did not find a reduction of the anterior part in children with NE II. The differences in results could be due to the different methods that were used, but additionally one should take into account that the number of children studied by Maneru et al. (19) is rather small, especially the number of the NE I group.
In our study, there was a significant difference in CC size between children with NE II and controls, but no significant difference was found between children with NE I and both children with NE II and controls. It seems that the area of the CC shows a gradual reduction in size associated with the increase in grade of encephalopathy.
Both Whalley et al. (21) and Rauch and Jinkins (22) reported that the volume of the CC can be approximated by measuring its cross-sectional area on MRI. By choosing the midsagittal plane one has a reproducible site for the measurement and the contours of the CC are clearly seen because of the cerebral spinal fluid surrounding almost its entire course (22).
The differences in shape and area of the CC found in the children with NE are slightly different from those previously reported in infants born preterm, who tend to have a less diffuse distribution of CC lesions. Periventricular leukomalacia found in preterms mainly affect the parietal and occipital periventricular white matter and therefore the area of the posterior part of the CC is especially reduced (16,25). In contrast, full-term infants with NE show more widespread and different patterns of cerebral lesions, like watershed injury and/or involvement of the deep gray nuclei (7–10). These patterns can explain the more diffuse involvement of the CC (26). Results of the imaging data will be reported separately. It was of interest that visual assessment of the CC noted thinning of especially the middle part of the CC, while measurement showed that the posterior part was mainly reduced, showing that the measurements provided different but more reliable information than the visual assessment.
Suboptimal head growth and secondary microcephaly is not uncommon in infants with NE (27,28). This has been shown to be related to white matter lesions and severe basal ganglia and thalamic lesions. A suboptimal rate of head growth predicts an abnormal neurodevelopmental outcome (28,29). After adjusting for MCS as a possible confounder, the M-ABC scores were still related to the CC size. Boys have a larger brain size and a larger CC than girls. Once the CC was adjusted for MCS, no gender differences were found in total area of the CC (30). After correcting for gender, our results with relation to the measurements of the CC did not change. The CC is known to increase in size into early adulthood (12). To limit the effect of age, our children were nine or ten years old at the time of the examination.
All NE children showed a significantly poorer TIS on the M-ABC than the controls and there was no significant difference between children with NE I and NE II. This is of interest, because in the literature children with NE I are reported to have a normal outcome. Long-term follow-up data are, however, scarce and the time span of follow-up in previous studies is usually limited. The differences in the used assessments and in age at time of testing could be an explanation for the conclusion in this study and those reported in previous studies.
The mean difference between the M-ABC scores of children with NE and controls decreased after adjusting for size of the posterior part of the CC. This suggests that a reduction of this area partly explained the increase of the scores on the M-ABC: the smaller this area, the worse the motor outcome. If the CC size would not be an explanation, the difference in M-ABC scores would be the same before and after adjustment for the size. If the CC would fully explain the difference, the difference after adjustment would be zero and statistically nonsignificant. The CC links associative areas of the two cerebral hemispheres. Due to brain damage following asphyxia there are fewer fibers connecting both hemispheres. According to the data obtained in this study, this could affect motor performance. Further research should be done to assess whether special therapy early in life could limit this decrease in the number of fibers and so improve motor outcome.
The M-ABC does not purely assess motor performance. The outcome is also affected by cognition, attention, visual perception, behavioral problems, and sociodemographic factors (31,32). These possible confounders play a role in many assessments and further evaluation should be done to assess what their effect can be on motor performance. It is suggested that attention-deficit/hyperactivity disorder (ADHD) occurs more often in children with NE than in controls. However, Miyahara et al. (33) supported the motor deficit rather than the attention deficit hypothesis of manual incoordination in ADHD.
The number of participants was 73%, which was lower than anticipated. Many parents refused, due to lack of time or more commonly because of the MRI being part of the study protocol.
MRIs were not successfully performed in two children with NE I, three with NE II, and one control because of anxiety. Due to motion artifacts, the CC could not be reliably measured in one child with NE I, four children with NE II, and in two controls. There were only six children with NE (without CP), who had a TIS on the M-ABC above 20.0. In three of them, the CC could not (reliably) be measured. The two children with a MRI showed focal thinning. If it would have been possible to measure their areas of the CC, it is very likely that they would have been in the “lower range,” increasing the inverse association shown in Figure 3.
The M-ABC is not suitable to test the motor function of children with CP. After exclusion of these children, our results with regard to the size of the CC and the association between the CC and the M-ABC remained significant.
Little is known about the long-term outcome of children with NE (3–6). In this study, 21 children (33.3%) with NE had an abnormal outcome on the M-ABC (≤5th percentile) and 18 (28.6%) had a TIS between the 6th and 15th percentile. All survivors were seen in the follow-up clinic until 18 mo of age and only beyond when they showed an abnormal neurologic outcome. Our data show that children with NE experience more motor problems than was expected. The motor performance of our controls was within the normal range in 66% of the children, which is a lower percentage than the expected 85%. The reason remains as yet unexplained, but this observation once again shows the importance of having a control group. In view of our findings, it is strongly recommended to follow children with NE beyond infancy till school age, to enable recognition of cognitive and motor problems at an earlier age, and to start timely intervention.
In conclusion, children with both NE I and NE II without CP have poorer motor skills than controls, which is partly explained by a smaller size of especially the posterior part of the corpus callosum.
Abbreviations
- CC:
-
corpus callosum
- M-ABC:
-
Movement Assessment Battery for Children
- MCS:
-
midsagittal cerebral size
- NE:
-
neonatal encephalopathy
- NE I:
-
mild neonatal encephalopathy
- NE II:
-
moderate neonatal encephalopathy
- TIS:
-
Total Impairment Score
References
Ferriero DM 2004 Neonatal brain injury. N Engl J Med 351: 1985–1995
Sarnat HB, Sarnat MS 1976 Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch Neurol 33: 696–705
Marlow N, Rose AS, Rands CE, Draper ES 2005 Neuropsychological and educational problems at school age associated with neonatal encephalopathy. Arch Dis Child Fetal Neonatal Ed 90: F380–F387
Robertson CM, Finer NN 1993 Long-term follow-up of term neonates with perinatal asphyxia. Clin Perinatol 20: 483–500
van Handel M, Swaab H, de Vries LS, Jongmans MJ 2007 Long-term cognitive and behavioral consequences of neonatal encephalopathy following perinatal asphyxia: a review. Eur J Pediatr 166: 645–654
Gonzalez FF, Miller SP 2006 Does perinatal asphyxia impair cognitive function without cerebral palsy?. Arch Dis Child Fetal Neonatal Ed 91: F454–F459
Barnett A, Mercuri E, Rutherford M, Haataja L, Frisone MF, Henderson S, Cowan F, Dubowitz L 2002 Neurological and perceptual-motor outcome at 5–6 years of age in children with neonatal encephalopathy: relationship with neonatal brain MRI. Neuropediatrics 33: 242–248
Belet N, Belet U, Incesu L, Uysal S, Ozinal S, Keskin T, Sunter AT, Kucukoduk S 2004 Hypoxic-ischemic encephalopathy: correlation of serial MRI and outcome. Pediatr Neurol 31: 267–274
Rutherford M, Ward P, Allsop J, Malamatentiou C, Counsell S 2005 Magnetic resonance imaging in neonatal encephalopathy. Early Hum Dev 81: 13–25
Sie LT, van der Knaap MS, Oosting J, de Vries LS, Lafeber HN, Valk J 2000 MR patterns of hypoxic-ischemic brain damage after prenatal, perinatal or postnatal asphyxia. Neuropediatrics 31: 128–136
Barkovich AJ, Norman D 1988 Anomalies of the corpus callosum: correlation with further anomalies of the brain. AJR Am J Roentgenol 151: 171–179
Pujol J, Vendrell P, Junque C, Marti-Vilalta JL, Capdevila A 1993 When does human brain development end? Evidence of corpus callosum growth up to adulthood. Ann Neurol 34: 71–75
Barkovich AJ, Kjos BO 1988 Normal postnatal development of the corpus callosum as demonstrated by MR imaging. AJNR Am J Neuroradiol 9: 487–491
Santhouse AM, Ffytche DH, Howard RJ, Williams SC, Stewart AL, Rooney M, Wyatt JS, Rifkin L, Murray RM 2002 The functional significance of perinatal corpus callosum damage: an fMRI study in young adults. Brain 125: 1782–1792
de Lacoste MC, Kirkpatrick JB, Ross ED 1985 Topography of the human corpus callosum. J Neuropathol Exp Neurol 44: 578–591
Rademaker KJ, Lam JN, Van Haastert IC, Uiterwaal CS, Lieftink AF, Groenendaal F, Grobbee DE, de Vries LS 2004 Larger corpus callosum size with better motor performance in prematurely born children. Semin Perinatol 28: 279–287
Iai M, Tanabe Y, Goto M, Sugita K, Niimi H 1994 A comparative magnetic resonance imaging study of the corpus callosum in neurologically normal children and children with spastic diplegia. Acta Paediatr 83: 1086–1090
Mercuri E, Jongmans M, Henderson S, Pennock J, Chung YL, de Vries L, Dubowitz L 1996 Evaluation of the corpus callosum in clumsy children born prematurely: a functional and morphological study. Neuropediatrics 27: 317–322
Maneru C, Junque C, Salgado-Pineda P, Serra-Grabulosa JM, Bartres-Faz D, Ramirez-Ruiz B, Bargallo N, Tallada M, Botet F 2003 Corpus callosum atrophy in adolescents with antecedents of moderate perinatal asphyxia. Brain Inj 17: 1003–1009
Cowan F, Rutherford M, Groenendaal F, Eken P, Mercuri E, Bydder GM, Meiners LC, Dubowitz LM, de Vries LS 2003 Origin and timing of brain lesions in term infants with neonatal encephalopathy. Lancet 361: 736–742
Whalley HC, Wardlaw JM 2001 Accuracy and reproducibility of simple cross-sectional linear and area measurements of brain structures and their comparison with volume measurements. Neuroradiology 43: 263–271
Rauch RA, Jinkins JR 1994 Analysis of cross-sectional area measurements of the corpus callosum adjusted for brain size in male and female subjects from childhood to adulthood. Behav Brain Res 64: 65–78
Henderson SE, Sugden DA, Smits-Engelsman BC 1998 Specifieke instructies voor de afname van de Movement ABC test. Movement Assessment Battery for Children. Swets & Zeitlinger, Lisse, Netherlands, pp 67–85
Witelson SF 1989 Hand and sex differences in the isthmus and genu of the human corpus callosum. A postmortem morphological study. Brain 112: 799–835
Nosarti C, Rushe TM, Woodruff PW, Stewart AL, Rifkin L, Murray RM 2004 Corpus callosum size and very preterm birth: relationship to neuropsychological outcome. Brain 127: 2080–2089
Miller SP, Ramaswamy V, Michelson D, Barkovich AJ, Holshouser B, Wycliffe N, Glidden DV, Deming D, Partridge JC, Wu YW, Ashwal S, Ferriero DM 2005 Patterns of brain injury in term neonatal encephalopathy. J Pediatr 146: 453–460
Cordes I, Roland EH, Lupton BA, Hill A 1994 Early prediction of the development of microcephaly after hypoxic-ischemic encephalopathy in the full-term newborn. Pediatrics 93: 703–707
Mercuri E, Ricci D, Cowan FM, Lessing D, Frisone MF, Haataja L, Counsell SJ, Dubowitz LM, Rutherford MA 2000 Head growth in infants with hypoxic-ischemic encephalopathy: correlation with neonatal magnetic resonance imaging. Pediatrics 106: 235–243
Gale CR, O'Callaghan FJ, Godfrey KM, Law CM, Martyn CN 2004 Critical periods of brain growth and cognitive function in children. Brain 127: 321–329
Bishop KM, Wahlsten D 1997 Sex differences in the human corpus callosum: myth or reality?. Neurosci Biobehav Rev 21: 581–601
Ozmert EN, Yurdakok K, Soysal S, Kulak-Kayikci ME, Belgin E, Ozmert E, Laleli Y, Saracbasi O 2005 Relationship between physical, environmental and sociodemographic factors and school performance in primary schoolchildren. J Trop Pediatr 51: 25–32
Resnick MB, Gueorguieva RV, Carter RL, Ariet M, Sun Y, Roth J, Bucciarelli RL, Curran JS, Mahan CS 1999 The impact of low birth weight, perinatal conditions, and sociodemographic factors on educational outcome in kindergarten. Pediatrics 104: e74
Miyahara M, Piek J, Barrett N 2006 Accuracy of drawing in a dual-task and resistance-to-distraction study: motor or attention deficit?. Hum Mov Sci 25: 100–109
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Kooij, B., van Handel, M., Uiterwaal, C. et al. Corpus Callosum Size in Relation to Motor Performance in 9- to 10-Year-Old Children with Neonatal Encephalopathy. Pediatr Res 63, 103–108 (2008). https://doi.org/10.1203/PDR.0b013e31815b4435
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e31815b4435
This article is cited by
-
Comparison of MRI and neurosonogram 1- and 2-dimensional morphological measurements of the newborn corpus callosum
Pediatric Research (2019)
-
The long-term effect of perinatal asphyxia on hippocampal volumes
Pediatric Research (2019)
-
Neurodevelopmental outcome in survivors of hypoxic ischemic encephalopathy without cerebral palsy
European Journal of Pediatrics (2018)
-
Biometry of the corpus callosum assessed by 3D ultrasound and its correlation to neurodevelopmental outcome in very low birth weight infants
Journal of Perinatology (2017)