Abstract
Sildenafil is a pulmonary vasodilator shown to be effective in neonates, but conflicting data exist regarding its effect on arterial oxygenation. To address this issue, we tested the sildenafil effect on the piglet's hypoxic pulmonary vasoconstriction (HPV) response. A segmental lung atelectasis was created by obstructing the corresponding bronchus. Total pulmonary and specific flows to the atelectatic and contra-lateral lobes were measured by magnetic resonance (MR) before and 30-min post sildenafil (0.2 and 1 mg/kg i.v.) or saline administration. Flow was reduced (p < 0.01) in the atelectatic and increased in the contra-lateral lobe indicating an effective HPV response. Sildenafil at both doses significantly (p < 0.01) increased flow solely to the atelectatic lobe. At a dose of 1 mg/kg, sildenafil induced a decrease in Pao2 from 285 ± 37 to 161 ± 22 mm Hg (p < 0.01). We conclude that the HPV response in the newborn is capable of almost completely reducing blood flow to nonventilated lung units and is reversed following sildenafil i.v. administration in a dose-dependent manner. In the presence of lung parenchymal disease, the use of i.v. sildenafil as a pulmonary vasodilator may worsen arterial oxygenation by reversing the HPV response in nonventilated lung units.
Similar content being viewed by others
Main
Inhaled nitric oxide (NO) is a selective pulmonary vasodilator that significantly reduces the neonatal morbidity and mortality associated with pulmonary hypertension (1,2). Given the cost and need for a dedicated apparatus to administered inhaled NO, there has been a recent interest in alternative pharmacological approaches to achieve pulmonary vasodilation in infants.
Among the clinically approved and commercially available compounds, sildenafil, a phosphodiesterase 5 (PDE-5) inhibitor, is one of the most comprehensively studied drugs and found beneficial in the pulmonary hypertension treatment of adult and pediatric subjects (3). Except for the penile vasculature, PDE-5 expression is highest in the lung and even when parenterally administered, sildenafil has a pulmonary preferential vasodilatory effect (4).
The use of sildenafil as a pulmonary vasodilator in infants with lung disease is controversial. On one hand, innumerous clinical studies documented a significant improvement in arterial oxygenation (2,3,5–8). Yet, lung parenchymal disease (e.g. meconium aspiration syndrome) is commonly associated with pulmonary hypertension (9) and worsening of arterial oxygenation has been reported in animal models of this disease (10–12). As such, it has been suggested that sildenafil inhibits the hypoxic pulmonary vasoconstrictor (HPV) response leading to increased blood flow to nonventilated lung units (10). This speculative mechanism has never been properly evaluated.
Little is known about the HPV response in the newborn. When compared with the adult animal data, the HPV response is reduced early in life in sheep and rabbits (13–15), but after repeated stimulation, its magnitude is increased in the newborn pig (16).
Thus, the issue at stake is whether parenteral sildenafil administration at doses low enough to treat pulmonary hypertension reverses the HPV response in the newborn. A single recent study attempted to evaluate the intravenous sildenafil effect on the regional pulmonary blood flow of the meconium-induced pulmonary hypertension piglet model (17). In that study, sildenafil, at a dose of 0.2 mg/kg i.v., reduced pulmonary arterial pressure without significantly altering arterial oxygenation. Yet, the interpretation of the sildenafil effect on regional blood flow to well and poorly ventilated areas was made technically impossible to evaluate in that study, given the widespread parenchymal disease associated with meconium aspiration.
The purpose of this study was to comparatively evaluate blood flow changes to ventilated and nonventilated lung units in a newborn animal model of acute lobar atelectasis by flow-sensitive magnetic resonance (MR) imaging methods. We hypothesized that in the newborn, i.v. sildenafil, even in low doses, reverses the HPV response of nonventilated (atelectatic) lung units.
METHODS AND MATERIALS
Twenty newborn pigs (4–6 d old) were studied. General anesthesia was induced with ketamine (20 mg/Kg, i.m.) and akemizine (0.5 mg/Kg, i.m.) and initially maintained with 2% isoflurane and subsequent to the placement of a femoral vein catheter with intravenous pentobarbital (30 mg/kg induction followed by continuous infusion of 0.2 mg/kg/min).
The animals were maintained warm with the use of a heating blanket and the body temperature together with heart rate, respiratory rate, oxygen saturation (pulse oximetry, Novametrix Cosmo, Pittsburgh, PA, USA), and end-tidal CO2 (Puritan Bennett, Pleasanton, CA, USA) continuously measured. At the end of the study, the animals were killed with an overdose of pentobarbital and the lung tissue frozen for cGMP content measurement. All procedures were conducted according to criteria established by the Canadian Council on Animal Care and approved by The Hospital for Sick Children Research Institute Animal Care Review Committee.
Mechanical ventilation and hemodynamic measurements.
An incision was made in the neck, and both internal jugular vein and carotid artery were dissected. A 5-F Argyle umbilical catheter was introduced in the carotid artery and advanced into the aorta and a 3.5 F Swan-Ganz catheter into the jugular vein and guided into the pulmonary artery by fluoroscopy (OmniDiagnost Eleva Philips, USA). Both catheters were connected to Hewlett-Packard 1280 transducers for continuous measurement of systemic and pulmonary arterial pressures (Hewlett-Packard, Waltham, MA, USA).
A tracheostomy was performed and a cuffed tracheal tube inserted for mechanical ventilation (Servo 300-Siemens Medical Systems, Erlangen, Germany). The animals were ventilated on pure oxygen at a tidal volume of 5 mL/kg, positive end expiratory pressure = 5 cm H2O. The ventilatory rates were adjusted to maintain an end-tidal Pco2 = 40 mm Hg.
Right lobar atelectasis.
To induce right lower lobe atelectasis, a 3.5-F vascular balloon catheter (Stouffville, Ontario, Canada) was advanced through the endotracheal tube and fluoroscopy guided to place its tip immediately above the entrance to the right lower lobe bronchus. MR measurements were obtained before and after bronchus occlusion (inflation of the vascular balloon catheter). In preliminary experiments, we determined that right lower lobe atelectasis was consistently obtained in less than 5-min postbronchial occlusion (Fig. 1).
Sildenafil administration.
The sildenafil powder (generously supplied by Pfizer, New York, New York, USA) was reconstituted in normal saline (2 mg/mL) and administered intravenously over 10 min at a dose of 0.2 (n = 7) or 1 mg/kg (n = 7). Control animals (n = 6) received a similar volume of saline solution. Measurements were obtained pre and 30-min postsildenafil or saline administration.
cGMP tissue content.
Cyclic guanine monophosphate (cGMP) lung tissue content was measured as a surrogate marker for PDE-5 activity in the atelectatic and contralateral lobes of control animals (n = 3) to comparatively evaluate the effect of alveolar hypoxia (30 min). The Perkin-Elmer kit (AlphaScreen® cGMP assay, Montreal Quebec, Canada) was used for this purpose, following manufacturer instructions.
Magnetic resonance imaging.
Studies were performed on a 1.5 Tesla MR scanner (GE Signa EXCITE III; General Electric Healthcare, Milwaukee, WI, USA) equipped with high-performance gradients (slew rate of 150 mT/m/ms; amplitude of 40 mT/m) and an eight-channel birdcage receiver coil.
The anesthetized animals were imaged supine and mechanically ventilated using an MR-compatible ventilator (LTV model 1200, Viasys Health Care, Minneapolis, MN, USA). Electrocardiographic leads were attached to the chest to provide a gating signal for the MR data acquisition.
For localization, three sets of images covering the chest in the coronal, axial, and sagittal planes were acquired at the beginning of the examination using a two-dimensional nongated steady state free precession imaging sequence. Visualization of the previously inserted balloon was possible by momentarily inflating the balloon with saline during the acquisition of these images.
Regional pulmonary blood flow was then measured using a velocity-sensitive MR technique known as phase-contrast (PC) MRI (18) and proven to have an accuracy of within 3% of the actual measurement (19). The vessel feeding the lower right segment was targeted first by prescribing an imaging plane perpendicular to the vessel at the level of the balloon. The contralateral vessel was then targeted and the scan was repeated. These cardiac-gated scans resulted in 20 cross-sectional images of each peripheral artery throughout the cardiac cycle, with pixel intensities equal to the blood-flow velocity through the imaging plane (Fig. 2). Velocity scans of both the vessels were repeated after induction of segmental atelectasis, and again after administration of sildenafil, the resulting change in volume flow was calculated.
Representative MR blood-flow measurement in one animal. (A) Anatomical slice depicting the artery feeding the right lower segment of the lung (arrow). (B) Two velocity maps corresponding to the boxed area in (A) but taken from different points in the cardiac cycle: systolic flow (top) and diastolic flow (bottom). Bright pixels indicate superior flow and dark pixels inferior flow. (C) Blood flow measured in the feeding artery before (•) and after (▴) atelectasis of the right lower segment of the lung. Flow integrated over the cardiac cycle was approximately 1.0 mL and 0.3 mL before and after collapse, respectively.
Specific imaging parameters for this sequence were field-of-view = 12 × 12 cm, in-plane spatial resolution ≈ 0.5 × 0.5 mm2, slice thickness = 5 mm, aliasing velocity = ±100 cm/s, effective temporal resolution = 17 to 34 ms, and number of signal averages = 3.
Flow analysis.
Quantitative analysis of the PC MR data was performed using commercial software with customized routines (MATLAB–Mathworks, Natick, MA, USA). First, conventional background-phase correction was applied to the data to remove background velocity errors from the images (20). A region of interest (ROI) was then drawn to identify the lumen of each targeted pulmonary artery in the PC MR data. The average velocity over the ROI was multiplied by the area of the ROI to calculate the flow volume in each image. Summation of these volumes over all 20 images produced the volume flow per cardiac cycle. From these values, percentage changes in flow relative to baseline (i.e. before atelectasis) were calculated at each stage of the experiment.
Data analysis.
Data were evaluated by one-way analysis of variance with multiple comparisons obtained by the Tukey-Krammer test when appropriate. Statistical significance was accepted at p < 0.05. All statistical analyses were performed with the Number Cruncher Statistical System (NCSS, Kaysville, Utah, USA). Results are presented as mean ± SEM.
RESULTS
Hemodynamic and oxygenation changes induced by right lobar atelectasis.
Right lower lobe atelectasis resulted in a significant increase in mean pulmonary arterial pressure (p < 0.01) and decrease in PaO2 (p < 0.01) without altering cardiac output or systemic blood pressure (Table 1). Regional blood flow to the atelectatic lung lobe was significantly (p < 0.01) reduced by 64%, whereas the flow to the contralateral lung region tended to increase, but the change was not statistically significant (p = 0.25; Table 1).
Sildenafil effect.
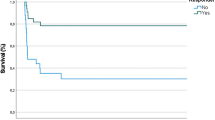
Sildenafil infusion resulted in a significant (p < 0.01) decrease in pulmonary and systemic arterial pressures (Fig. 3). At a dose of 0.2 mg/kg, sildenafil reduced the pulmonary arterial pressure to a level comparable to the preatelectasis measurement. A further nonstatistically significant reduction in pulmonary arterial pressure was observed in the animals treated with 1 mg/kg.
Figure 4 illustrates the total and regional changes in pulmonary blood flow in the control and sildenafil-treated animals. Administration of 1 mg/kg sildenafil significantly increased the regional blood flow to the right lower atelectatic lobe (p < 0.01) without statistically altering the flow in the contralateral lower lobe (Fig. 4). The regional flows shown in Fig. 4 represent only that fraction of the cardiac output reaching the lower segments of the left and right lungs, and as such are not equal to the total flow.
Sildenafil did not significantly alter either the total pulmonary blood flow (cardiac output) or pulmonary or systemic vascular resistance (Fig. 5). When compared with the control group, arterial oxygenation progressively decreased after sildenafil administration and was significantly lower (p < 0.01) at the 1 mg/kg dose (Fig. 6).
The cGMP content of the atelectatic right lobe was 115 ± 12 pmol/mg tissue protein and not significantly different when compared with the left contralateral lobe (127 ± 15 pmol/mg tissue protein). These tissue cGMP content data suggest that atelectasis does not acutely increase PDE-5 activity in the piglet lung.
DISCUSSION
Ventilating anesthetized adult cats with a hypoxic gas mixture, Liljestrand was the first to report the association between alveolar hypoxia and increased pulmonary vascular resistance (21). This physiologic response minimizes ventilation-perfusion mismatch, by reducing blood flow to poorly ventilated areas, thus optimizing blood oxygenation. In the newborn, the HPV response has been documented to exist, but it remains unknown how this response varies with age in humans. In sheep (14,22) and rabbit (15), the magnitude of response was reported to be lowest in the newborn and increased with age.
Lung parenchymal disease is a common finding in infants with pulmonary hypertension, and meconium aspiration is the most common associated pathology and present in as many as 41% of the patients in one study (9). If intact, the HPV response would limit blood flow to lung units filled with meconium, thus maximizing ventilation-perfusion mismatch. The goal of this study was to evaluate whether intravenous administration of sildenafil reverses the HPV response in the newborn.
We developed a newborn animal model of unilateral lobar atelectasis and used PC MR imaging to simultaneously measure regional blood flow to the atelectatic and contralateral lung units. We purposefully did not attempt to use pulmonary vasoconstrictor agonists (i.e. thromboxane A2 analogue) to further increase the pulmonary arterial pressure. This was done to study the sildenafil effect on the atelectasis-induced physiologically mediated HPV response in the absence of other confounding pharmacological agonist effects on the pulmonary circulation.
In this study, we documented the reversal of HPV response with sildenafil in a dose-dependent manner, resulting in increased ventilation-perfusion mismatch and reduced arterial oxygenation in piglets. These data are in-keeping with previous reports of intravenous sildenafil use in a piglet model of meconium-induced pulmonary hypertension, where worsening of oxygenation was also observed (10–12). In contrast with these previous studies, ours is the first to evaluate the effect of the drug on the HPV response of a noninjured lung.
In adult humans and animals, sildenafil administered either orally or intravenously suppresses the HPV response (23,24). In adult dogs, sildenafil partially reversed pulmonary vasoconstriction induced by inhaled hypoxic gas, but less so than inhaled NO (24). Yet a significant decrease in oxygenation and increase in V/Q mismatch was reported following intravenous administration of prostacyclin, but were not observed after oral administration of sildenafil to human subjects with chronic parenchymal lung disease (25).
Sildenafil has been advocated for the treatment of infants with pulmonary hypertension based on favorable anecdotal and small-scale clinical studies (2). Oral (5,26) intratracheal or intravenous (27) therapeutic use of sildenafil has been reported to result in improvement in the arterial oxygenation of children with pulmonary hypertension. Sildenafil, however, is not a selective pulmonary vasodilator, and its intravenous administration has been shown to cause systemic hypotension in animals and humans (24,28,29).
A recently published Cochrane review of sildenafil use as a pulmonary vasodilator in infants reported a favorable clinical response, reduction of mortality, and absence of significant side effects, but did not recommend it as a standard therapy (30). Yet, there are reports of worsening oxygenation after sildenafil administration to infants for the treatment of surgically induced pulmonary hypertension (31–33).
The possible explanation for the apparent discrepancy in the sildenafil effect on oxygenation among the different studies lies in the acute nature of the animal experimental models and the chronic characteristics of lung parenchymal disease. Exposure to hypoxia for at least 3 hours selectively suppresses the HPV response and animals living at high altitude exhibit a weak or absent response (34). The HPV response has also been shown to markedly decrease after 5 days in adult rabbits exposed to chronic hypoxia,(35) possibly secondary to an increase in NO production that abrogates the HPV response (36).
We speculate that in infants with pulmonary hypertension and associated lung disease the HPV response wanes over time contributing to the worsening gas exchange. Under these conditions of a time-suppressed HPV response, the sildenafil pulmonary vasodilatory effect will enhance blood perfusion to ventilated segments without altering it to the nonventilated lung units. As such, the end result will improve oxygenation. A similar phenomenon may be present in adults with chronic parenchymal lung disease accounting for the therapeutically beneficial effect of sildenafil (25). Furthermore, experimental testing of sildenafil in chronic animal models of lung parenchymal disease is necessary to test this hypothesis.
Last, hypoxia has been shown to upregulate PDE-5 activity in some (37), but not other chronic animal models (38). In vitro experiments on the magnitude of NO generation under hypoxic conditions support this speculation. Grimminger et al. showed that in rabbit lungs examined ex vivo, exhaled NO was significantly reduced after hypoxia (39), possibly as a result of an O2-dependent reduction in airway epithelial NO production (40). The NO-mediated vasorelaxation was also found to be reduced in the perfused rabbit lungs (41), lending further support to the speculation that chronic hypoxia upregulates PDE-5 activity.
In this study, we evaluated the effect of acute hypoxia (reduced alveolar ventilation) on the PDE-5 activity. We used the lung cGMP level as a surrogate marker for PDE-5 activity. No significant differences in cGMP levels were observed in the atelectatic when compared with the contralateral lobe 30 min after balloon inflation. In rats, pentobarbital anesthesia and mechanical ventilation acutely increase the lung tissue cGMP content (42), possibly as a result of decreased PDE-5 activity. Thus, it is possible that a similar effect on the piglet preparation used in this study masked any alveolar hypoxia (atelectasis)-induced PDE-5 activity increase.
Anesthetics can also alter the HPV response, and isoflurane is known to significantly reduce its magnitude (43). A similar HPV response lowering effect was observed with pentobarbital in the ex vivo sheep lung (44). In this study, the atelectatic and nonatelectatic lung units were comparatively evaluated in each animal. As such, any anesthesia effect on the measurements would be similar for both lung regions.
In summary, we demonstrated that the newborn pig can mount a significant and effective acute HPV response that is acutely reversed by intravenous sildenafil in a dose-dependent manner. The present results are in keeping with other data showing a reduction in arterial oxygenation after sildenafil treatment. Although not a model of pulmonary hypertension, the newborn piglet data obtained in this study raise concern regarding the therapeutic use of sildenafil as a pulmonary vasodilator when associated with acute lung parenchymal disease.
Abbreviations
- HPV:
-
hypoxic pulmonary vasoconstriction response
- PDE-5:
-
phosphodiesterase-5
- PC:
-
phase contrast
- ROI:
-
region of interest
References
Cook LN, Stewart DL 2005 Inhaled nitric oxide in the treatment of persistent pulmonary hypertension/hypoxic respiratory failure in neonates: an update. J Ky Med Assoc 103: 138–147
Abman SH 2007 Recent advances in the pathogenesis and treatment of persistent pulmonary hypertension of the newborn. Neonatology 91: 283–290
Juliana AE, Abbad FC 2005 Severe persistent pulmonary hypertension of the newborn in a setting where limited resources exclude the use of inhaled nitric oxide: successful treatment with sildenafil. Eur J Pediatr 164: 626–629
Hemnes AR, Champion HC 2006 Sildenafil, a PDE5 inhibitor, in the treatment of pulmonary hypertension. Expert Rev Cardiovasc Ther 4: 293–300
Baquero H, Soliz A, Neira F, Venegas ME, Sola A 2006 Oral sildenafil in infants with persistent pulmonary hypertension of the newborn: a pilot randomized blinded study. Pediatrics 117: 1077–1083
Martell M, Blasina F, Silvera F, Tellechea S, Godoy C, Vaamonde L, Benenatti L, Olivera W 2007 Intratracheal sildenafil in the newborn with pulmonary hypertension. Pediatrics 119: 215–216
Obaid L, Johnson ST, Bigam DL, Cheung PY 2006 Intratracheal administration of sildenafil and surfactant alleviates the pulmonary hypertension in newborn piglets. Resuscitation 69: 287–294
Simiyu DE, Okello C, Nyakundi EG, Tawakal AH 2006 Sildenafil in management of persistent pulmonary hypertension of the newborn: report of two cases. East Afr Med J 83: 337–340
Walsh-Sukys MC, Tyson JE, Wright LL, Bauer CR, Korones SB, Stevenson DK, Verter J, Stoll BJ, Lemons JA, Papile LA, Shankaran S, Donovan EF, Oh W, Ehrenkranz RA, Fanaroff AA 2000 Persistent pulmonary hypertension of the newborn in the era before nitric oxide: practice variation and outcomes. Pediatrics 105: 14–20
Ryhammer PK, Shekerdemian LS, Penny DJ, Ravn HB 2006 Effect of intravenous sildenafil on pulmonary hemodynamics and gas exchange in the presence and absence of acute lung injury in piglets. Pediatr Res 59: 762–766
Shekerdemian LS, Ravn HB, Penny DJ 2004 Interaction between inhaled nitric oxide and intravenous sildenafil in a porcine model of meconium aspiration syndrome. Pediatr Res 55: 413–418
Shekerdemian LS, Ravn HB, Penny DJ 2002 Intravenous sildenafil lowers pulmonary vascular resistance in a model of neonatal pulmonary hypertension. Am J Respir Crit Care Med 165: 1098–1102
de Clety SC, Decell MK, Tod ML, Sirois P, Gordon JB 1998 Developmental changes in synthesis of and responsiveness to prostaglandins I2 and E2 in hypoxic lamb lungs. Can J Physiol Pharmacol 76: 764–771
Gordon JB, Tod ML, Wetzel RC, McGeady ML, Adkinson NF Jr Sylvester JT 1988 Age-dependent effects of indomethacin on hypoxic vasoconstriction in neonatal lamb lungs. Pediatr Res 23: 580–584
Fike CD, Hansen TN 1987 Hypoxic vasoconstriction increases with postnatal age in lungs from newborn rabbits. Circ Res 60: 297–303
Belik J, Sienko A, Light RB 1990 The effect of repeated intermittent hypoxia on pulmonary vasoconstriction in the newborn. Can J Physiol Pharmacol 68: 355–362
Ryhammer P, Pedersen M, Ringgaard S, Ravn H 2007 Regional pulmonary perfusion using model-free analysis of contrast-enhanced MRI in meconium-aspirated piglets. J Magn Reson Imaging 26: 296–303
Lotz J, Meier C, Leppert A, Galanski M 2002 Cardiovascular flow measurement with phase-contrast MR imaging: basic facts and implementation. Radiographics 22: 651–671
Lankhaar JW, Hofman MB, Marcus JT, Zwanenburg JJ, Faes TJ, Vonk-Noordegraaf A 2005 Correction of phase offset errors in main pulmonary artery flow quantification. J Magn Reson Imaging 22: 73–79
Walker PG, Cranney GB, Scheidegger MB, Waseleski G, Pohost GM, Yoganathan AP 1993 Semiautomated method for noise reduction and background phase error correction in MR phase velocity data. J Magn Reson Imaging 3: 521–530
Liljestrand G 1958 Chemical control of the distribution of the pulmonary blood flow. Acta Physiol Scand 44: 216–240
Gordon JB, Hortop J, Hakim TS 1989 Developmental effects of hypoxia and indomethacin on distribution of vascular resistances in lamb lungs. Pediatr Res 26: 325–329
Zhao L, Mason NA, Morrell NW, Kojonazarov B, Sadykov A, Maripov A, Mirrakhimov MM, Aldashev A, Wilkins MR 2001 Sildenafil inhibits hypoxia-induced pulmonary hypertension. Circulation 104: 424–428
Fesler P, Pagnamenta A, Rondelet B, Kerbaul F, Naeije R 2006 Effects of sildenafil on hypoxic pulmonary vascular function in dogs. J Appl Physiol 101: 1085–1090
Ghofrani HA, Wiedemann R, Rose F, Schermuly RT, Olschewski H, Weissmann N, Gunther A, Walmrath D, Seeger W, Grimminger F 2002 Sildenafil for treatment of lung fibrosis and pulmonary hypertension: a randomised controlled trial. Lancet 360: 895–900
Abrams D, Schulze-Neick I, Magee AG 2000 Sildenafil as a selective pulmonary vasodilator in childhood primary pulmonary hypertension. Heart 84: E4
Nagdyman N, Fleck T, Bitterling B, Ewert P, Abdul-Khaliq H, Stiller B, Hubler M, Lange PE, Berger F, Schulze-Neick I 2006 Influence of intravenous sildenafil on cerebral oxygenation measured by near-infrared spectroscopy in infants after cardiac surgery. Pediatr Res 59: 462–465
Nieminen T, Koobi T, Tammela TL, Kahonen M 2006 Hypotensive potential of sildenafil and tamsulosin during orthostasis. Clin Drug Investig 26: 667–671
Jackson G, Montorsi P, Cheitlin MD 2006 Cardiovascular safety of sildenafil citrate (Viagra): an updated perspective. Urology 68: 47–60
Shah PS, Ohlsson A 2007 Sildenafil for pulmonary hypertension in neonates. Cochrane Database Syst Rev: CD005494
Schulze-Neick I, Hartenstein P, Li J, Stiller B, Nagdyman N, Hubler M, Butrous G, Petros A, Lange P, Redington AN 2003 Intravenous sildenafil is a potent pulmonary vasodilator in children with congenital heart disease. Circulation 108: II167–II173
Schulze-Neick I, Redington AN 2004 Sildenafil, nitric oxide, and acute lung injury: pathophysiology beats pharmacotherapy?. Pediatr Res 55: 370–371
Stocker C, Penny DJ, Brizard CP, Cochrane AD, Soto R, Shekerdemian LS 2003 Intravenous sildenafil and inhaled nitric oxide: a randomised trial in infants after cardiac surgery. Intensive Care Med 29: 1996–2003
Moudgil R, Michelakis ED, Archer SL 2005 Hypoxic pulmonary vasoconstriction. J Appl Physiol 98: 390–403
Weissmann N, Nollen M, Gerigk B, Ardeschir GH, Schermuly RT, Gunther A, Quanz K, Fink L, Hanze J, Rose F, Seeger W, Grimminger F 2003 Downregulation of hypoxic vasoconstriction by chronic hypoxia in rabbits: effects of nitric oxide. Am J Physiol Heart Circ Physiol 284: H931–H938
Archer SL, Tolins JP, Raij L, Weir EK 1989 Hypoxic pulmonary vasoconstriction is enhanced by inhibition of the synthesis of an endothelium derived relaxing factor. Biochem Biophys Res Commun 164: 1198–1205
MacLean MR, Johnston ED, McCulloch KM, Pooley L, Houslay MD, Sweeney G 1997 Phosphodiesterase isoforms in the pulmonary arterial circulation of the rat: changes in pulmonary hypertension. J Pharmacol Exp Ther 283: 619–624
Kirsch M, Kemp-Harper B, Weissmann N, Grimminger F, Schmidt HH 2008 Sildenafil in hypoxic pulmonary hypertension potentiates a compensatory up-regulation of NO-cGMP signaling. FASEB J 22: 30–40
Grimminger F, Spriestersbach R, Weissmann N, Walmrath D, Seeger W 1995 Nitric oxide generation and hypoxic vasoconstriction in buffer-perfused rabbit lungs. J Appl Physiol 78: 1509–1515
Ide H, Nakano H, Ogasa T, Osanai S, Kikuchi K, Iwamoto J 1999 Regulation of pulmonary circulation by alveolar oxygen tension via airway nitric oxide. J Appl Physiol 87: 1629–1636
Weissmann N, Winterhalder S, Nollen M, Voswinckel R, Quanz K, Ghofrani HA, Schermuly RT, Seeger W, Grimminger F 2001 NO and reactive oxygen species are involved in biphasic hypoxic vasoconstriction of isolated rabbit lungs. Am J Physiol Lung Cell Mol Physiol 280: L638–L645
Klass DJ 1978 Lung tissue guanosine 3′,5′-monophosphate: effects of ventilation and anesthesia. J Appl Physiol 45: 487–494
Mathers J, Benumof JL, Wahrenbrock EA 1977 General anesthetics and regional hypoxic pulmonary vasoconstriction. Anesthesiology 46: 111–114
Wetzel RC, Martin LD 1989 Pentobarbital attenuates pulmonary vasoconstriction in isolated sheep lungs. Am J Physiol 257: H898–H903
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by grants from the Canadian Institutes of Health Research.
Rights and permissions
About this article
Cite this article
Tessler, R., Wu, S., Fiori, R. et al. Sildenafil Acutely Reverses the Hypoxic Pulmonary Vasoconstriction Response of the Newborn Pig. Pediatr Res 64, 251–255 (2008). https://doi.org/10.1203/PDR.0b013e31817d9b93
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e31817d9b93