Abstract
We investigated possible influences of single nucleotide polymorphisms (SNPs) on first-year growth velocity in response to growth hormone (GH) therapy in GH-deficient (GHD) children. We recruited a total of 154 GHD prepubertal children who had undergone GH therapy for 1 y. To exclude the possibility that the genotype/allele variants influenced the height of GHD patients, we studied the same gene polymorphisms in 208 familial short stature (FSS) patients and 100 normal control individuals. In the present study, the first-year growth velocities of GHD patients treated with GH were measured and then compared with the allelic frequencies of various SNP of genes involved in the GH–insulinlike growth factor-I (IGF-I) axis. Only c.1319 G>T of the GH receptor (GHR) gene showed significant correlation with first-year growth velocity (p = 0.02). However, the genetic frequency of the c.1319 G>T polymorphism of GHD did not correlate with FSS and normal controls. Therefore, the c.1319 G>T polymorphism does not influence the height of individuals but can affect the therapeutic efficacy of GH in GHD patients. Moreover, the GHR c.1319 T allele showed higher transcriptional activity and stronger signal transducers and activators of transcription (STAT)-5 Tyr694 phosphorylation. Based on these findings, we conclude that the GHRc.1319 T allele is associated with the therapeutic efficacy of GH replacement therapy.
Similar content being viewed by others
Main
Growth hormone (GH) is a pleiotropic cytokine that plays a central role in growth differentiation and metabolism by altering gene expression in target cells. The growth hormone receptor (GHR) is widely expressed in many tissues, including the liver, heart, kidney, intestine, skeletal muscle, pancreases, brain, and testis. Binding of the GH protein to its receptor induces a cascade of cellular events, such as the dimerization of the GHR and phosphorylation of Janus-activated kinase 2 (JAK2). These molecules serve in signal transduction by phosphorylating signal transducers and activators of transcription-5 (1). Signal transducers and activators of transcription (STATs) then induce the transcription of insulinlike growth factor (IGF)-I and IGF-II and modulation of the expression of other genes. IGFs are found in plasma bound to a family of proteins called IGF binding proteins (IGFBPs). The majority of IGFs bind to IGFBP-3; this binary complex then binds to a third protein known as the acid-labile subunit (ALS) to form a ternary complex in serum (2). IGF-I is thought to interact with target organs such as growing cartilage and muscle to induce growth (1–3). Suppressor of cytokine signaling-2 (SOCS-2) is a member of the suppressor of cytokine signaling family, a group of related proteins implicated in the negative regulation of cytokine action through inhibition of the JAK-STAT signaling pathway. Genetic studies have shown that SOCS-2 plays important roles in growth and development. For example, SOCS-2 knockout mice grew significantly larger than their wild-type littermates. Furthermore, STAT5 signaling has been shown to be prolonged in SOCS-2–deficient hepatocytes after stimulation with GH (4).
GH therapy given to typical growth hormone deficiency (GHD) children accelerates growth from a pretreatment rate of 3–4 cm/y to 6–12 cm/y in the first year of therapy. The therapeutic effect can be further improved by treating children earlier, administering larger doses, and increasing the frequency of administered recombinant GH (5). However, the therapeutic efficacy has been shown to vary among individuals. Some GHD children respond poorly (6–7 cm), while others respond very well (10–12 cm) during the first year of therapy. The mechanism by which GH regulates growth velocity involves a complex cascade of numerous genes and factors. Several studies have reported that bone age, mid-parental height, age at treatment, treatment duration, and GH concentration influence the efficacy of GH therapy in GHD children; however, the genetic factors associated with GH replacement therapy remain poorly defined.
Single nucleotide polymorphisms (SNPs) are used as a tool for mapping complex disease genes. We evaluated known SNP of some of the genes involved in the cascade of GH stimulation to see whether they influence the efficacy of GH replacement therapy in GHD children in Taiwan. In this study, the first-year growth velocities of GHD patients treated with GH were measured and then compared with the allelic frequencies of various SNPs of genes involved in the GH–IGF-I axis. Polymorphisms of the following genes were evaluated: GHR (c.1319 G>T, c. 1473 T>C, c. 1483 A>C, c. 1630 C>A), JAK2 (c.1752 T>A), STAT-5a (c.1903 C>T), STAT-5b (c.389 C>T), IGF-I (c.5 G>A), IGFBP-3 (c.1323 G>A), ALS (c.1386 C>T), and SOCS-2 (c.140-132 T>C, c.20 A>G). GHR (c.1319 G>T, c.1473 T>C, c.1483 A>C) and SOCS-2 (c.140-132 T>C) were also confirmed at the National Genotyping Center at Academia Sinica, Taipei, Taiwan, by mass spectrometry. A common GHR polymorphism generated by exon 3 retention or deletion (d3-GHR) has been shown to be associated with first-year growth velocity after GH treatment in Brazilian children (7). Therefore, we also evaluated the d3-GHR polymorphism in this study. Body height is determined by various genetic, nutritional, and environmental factors. Therefore, we investigated the relationship among polymorphisms of multiple growth-related genes and clinical parameters such as body weight, gender, body mass index (BMI), height of parents, and hypothalamic condition in GHC children. We also used statistical methods to analyze the difference in growth response after 1 y of GH treatment. This research will lead to improvements in adult height prediction before treating GHD patients with GH replacement therapy, as well as to a better treatment regimen for children with GHD.
METHODS
Patients.
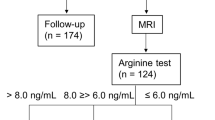
We studied 154 prepubertal GHD children (108 boys and 46 girls) who had undergone 1 y of GH therapy. The pubertal status was evaluated by a Chinese version of a self-administered rating scale for pubertal development. The forms were completed by the patients or at least one of their parents (8). All patients met the following inclusion criteria: 1) height SD score had to be more than 2 SD below the mean chronological age at the initial endocrine evaluation; 2) growth velocity had to be <4 cm/y; 3) all participants had to have a bone age delay of >2 y; 4) peak GH had to be <10 ng/mL after 2 SDs [insulin tolerance test (insulin-induced hypoglycemia) and clonidine evocation test)] GH-provocative tests; 5) participants had to be prepubertal at the end of 1 y of GH therapy. All patients had been evaluated for 1 y for growth velocity before GH replacement therapy was begun. The height was expressed in centimeters and SDs according to Taiwan standards (9). Other clinical data evaluated before treatment included birth weight, height of parents, maximal peak GH value, and the size and shape of pituitary gland detected by magnetic resonance imaging (MRI). We excluded patients with any additional pituitary hormone deficiency, malformation syndromes, chronic diseases, central nervous system tumors, anatomic abnormality of the pituitary gland on MRI, patients who were born small for gestational age (SGA), and patients who had received previous GH therapy. GH (Genotropin, Pfizer) 0.18 mg/kg/wk was administered by s.c. injection on a daily basis in the evening for 12 mo. Growth velocity was measured every 2 mo within the observation period of 12 mo. Left hand and wrist radiographs were assessed for bone age determination by three observers based on the method reported by Greulich and Pyle (10).
To elucidate whether the genotype/allele variants influenced the height of GHD patients, a total of 208 familial short stature (FSS) children and 100 control individuals were recruited in this study. FSS was defined when the child's predicted adult height was <−2 SDs below average height (149 cm in females, 160 cm in males) as well as the absence of malnutrition, chronic disease, and endocrinological disorders. Predicted adult height was calculated using the following equation: (father's height + mother's height)/2 + 6.5 cm for boys or −6.5 cm for girls. Other clinical records were selected for FSS, including birth weight, height of parents, maximal peak GH value, and the size and shape of pituitary gland detected by MRI. Normal controls were defined height SD score had to be between ±2 SDs the mean chronological age and no evidence of any endocrinological disease. Clinical and auxological characteristics of GHD, FSS, and control individuals are shown in Table 1. This study was approved by the ethics committee and institutional review board of the China Medical University Hospital. Informed consent was obtained from all patients and the controls or their guardians.
SNP genotyping. Polymerase chain reaction (PCR)–restriction fragment length polymorphism (RFLP) and PCR experiments were conducted to detect the SNP in the following genes: GHR (c.1319 G>T, c. 1473 T>C, c. 1483 A>C, c. 1630 C>A), JAK2 (c.1752 T>A), STAT-5a (c.1903 C>T), STAT-5b (c.389 C>T), IGF-I (c.5 G>A), IGFBP-3 (c.1323 G>A), ALS (c.1386 C>T), and SOCS-2 (c.140-132 T>C, c.20 A>G). PCRs were carried out in a total volume of 25 μL, containing 50 ng genomic DNA; 2–6 pmole of each primer; 1× Taq polymerase buffer (1.5 mM MgCl2); and 0.25 units of AmpliTaq DNA polymerase (Applied Biosystems). After PCR amplification, the individual gene polymorphisms were analyzed by restriction digestion with individual restriction enzymes (New England Biolabs). The PCR products were mixed together, and then 10 μL of this solution was loaded into 3% agarose gel containing ethidium bromide for electrophoresis.
GHR (c.1319 G>T, c.1473 T>C, c.1483 A>C) and SOCS-2 (c.140-132 T>C) were also determined at the National Genotyping Center at Academia Sinica, Taipei, Taiwan, to confirm our RFLP results. Briefly, the primers and probes were designed by SpectroDESIGNER software (Sequenom). PCR was performed, and unincorporated dNTPs were dephosphorylated by shrimp alkaline phosphatase followed by primer extension. The extended DNA fragments were spotted onto a 384-element silicon chip (SpectroCHIP, Sequenom), and then analyzed by a Bruker Biflex III MALDI-TOF SpectroREADER mass spectrometer (Sequenom).
Genotyping of d3-GHR was done according to the method developed by Pantel et al. (11) with modifications (12,13). For a given sample, we separately amplified full-length GHR isoforms and exon 3-deleted isoforms by two different PCRs using primer pairs G1:G3 and G1:G2, respectively. The sequences of G1, G2, and G3 primers are G1: 5′-TGTGCTGGTCTGTTGGTCTG-3′, G2: 5′-AGTCGTTCCTGGGACAGAGA-3′, and G3: 5′-CCTGGATTAACACTTTGCAGACTC-3′. PCRs were carried out in a total volume of 25 μL, containing 50 ng genomic DNA; 2–6 pmole of each primer; 1× Taq polymerase buffer; and 0.25 units of AmpliTaq DNA polymerase (Applied Biosystems). Amplication products were analyzed by gel electrophoresis on a 1% agarose gel containing ethidium bromide.
Statistical analysis.
Correlations were evaluated among these gene polymorphisms, clinical variants, and growth velocity after 1 y of GH therapy. Statistical analyses included analysis of variance (ANOVA), independent t test, χ2 test, and univariate and multivariate regression analyses. The relationship between growth rate and clinical parameters (bone age, birth weight, height of parents, BMI, and maximal peak GH value in GHD patients) was evaluated by multiple linear regression. A p value of <0.05 was considered statistically significant.
Reporter assay.
We performed a reporter assay to evaluate the relationship between the GHR c.1319 G>T polymorphism and GH treatment response. cDNA encoding full-length GHR was obtained from Dr. Michel Goosen (Institut National de la Sante et de la Recherche Medicale (INSERM), U91, Hôpital Henri Mondor, Creteil, France) (14). GHR cDNA was subcloned into a pcDNA3 vector (Invitrogen) between restriction enzyme cutting sites (human GHR-BamHI-F: 5′-TTTGGATCCCCTACAGGTATGGATCTCTGG-3′ and human GHR-XhoI-R: 5′-TTTCTCGAGAAGAAAGGCTAAGGCATGAT-3′) by PCR; the resulting plasmid was called pcGHR-G. Site-directed mutagenesis was carried out using the Clontech Transformer Site-Directed Mutagenesis Kit according to the manufacturer's instructions. The selection and mutagenic primer sequences were 5′-GGTTCTCCGGTTGCTTGGGTGG-3′ and 5′-CATGATGCTTTCCCTGCTACTC-3′. The mutated plasmid was called pcGHR-T. All constructs were checked by DNA sequencing to confirm that the only difference between the two copies of the GHR was c.1319 G or T. An artificial promoter containing six tandem repeats of lactogenic hormone response element (LHRE) (6) and the minimal thymidine kinase promoter were cloned into pTAL-SEAP (Clontech) for use as the STAT-5 response element. CHO-k1 cells were plated in six-well plates (106 cells per well) and then transfected with 1 μg pcGHR, 0.5 μg LHRE-TK-SEAP, and 0.5 μg pGL3-Control (Promega) per well. Cells were incubated for 24 h with serum-free medium containing either 100 ng/mL human GH and 250 nM dexamethasone or 250 nM dexamethasone alone. Cell culture supernatants and cell lysates were collected to determine secreted alkaline phosphatase and luciferase activities. Luciferase activity was normalized to the alkaline phosphatase activity; the results are represented as the mean (SEM) of three independent experiments done in triplicate.
Western blotting.
Western blotting was performed on CHO cells that had been transfected with either pcGHR-G or pcGHR-C, starved overnight in serum-free medium, and stimulated with GH at a concentration of 50 or 100 ng/mL. Cells were harvested 2 min (JAK2), 10 min [Erk1/2, p38, and c-Jun N-terminal kinase (Jnk)], and 30 min (STAT-1, -3, -5) after GH administration. Cells were washed three times with 10 mL of phosphate-buffered saline and lysed with M-PER (Pierce) containing Halt phosphatase inhibitor cocktail (Pierce). Antiphosphoprotein antibodies were obtained from Cell Signaling Technology. Proteins were separated on a 7.5% sodium dodecyl–polyacrylamide gel electrophoresis (SD-PAGE) gel and blotted onto polyvinylidene difluoride membrane. For visualization, membranes were probed with a species-specific secondary antibody conjugated to horseradish peroxidase; binding was detected by SuperSignal West Pico Chemiluminescent Substrate according to the manufacturer's instructions (Pierce). Blots shown are representative of at least three individual experiments.
RESULTS
We analyzed the first-year growth response of GHD patients who had been treated with GH. A total of 154 prepubertal children (108 boys and 46 girls) with GHD were included in the present study. To elucidate whether the genotypes influence height, 208 FSS individuals and 100 normal individuals were included as controls. The genotype frequencies of 13 gene polymorphisms were measured to evaluate the correlation between genotype and first-year growth velocity. GHR (c.1473 T>C), IGFBP-3 (c.1323 G>A), JAK2 (c.1752 T>A), IGF-I (c.5 G>A), STAT-5a (c.1903C>T), STAT-5b (c.389 C>T), and SOCS-2 (c.20 A>G) showed no DNA sequence polymorphisms. Among d3-GHR, GHR (c.1319 G>T, c.1483A>C, c.1630C>A), ALS (c.1386C>T), and SOCS-2 (c.140-302 T>C), only GHR c.1319 G>T was significantly correlated (p = 0.02) with the first-year growth velocity post–GH replacement therapy (Table 2). The genotype frequencies of GHR were 70.8% GG, 27.3% GT, and 1.9% TT; they were associated with a first-year growth velocity of 7.78 ± 2.03 cm, 8.64 ± 2.4 cm, and 11.8 ± 1.85 cm, respectively (Table 3). Furthermore, there was a statistically significant difference in change in height SD after GH therapy (Table 3). Height growth rates were higher in children with the T allele (GT and TT; Table 3); however, the frequency of c.1319 G>T polymorphism did not correlate with the body height of patients when compared with individuals with FSS or with individuals with normal height (Table 4). Furthermore, no significant differences were found in genotype/allele frequencies of the other SNP between GHD and FSS or GHD and control individuals (Table 4).
The growth response to GH treatment is influenced by various factors; therefore, we analyzed the correlation between the first-year growth velocity and the following variables by multiple linear regression analyses: growth velocity, gender, age, bone age, paternal height, maternal height, and birth weight, as well as BMI SD before and after GH replacement therapy, maximal concentration of serum GH (ng/mL) after evocation test, and GHR c.1319 G>T polymorphism. The only significant correlation was between c.1319 G>T and the first-year growth velocity. First-year growth velocity of the children with GG homozygote was used as the baseline to compare the one with GT heterozygote and TT homozygote. The G homozygote was associated with low growth velocity, the GT heterozygote corresponded with moderate growth velocity, and the T homozygote correlated with high growth velocity (Table 3). We also compared first-year growth velocity after GH replacement therapy with the d3-GHR polymorphism (Table 3); however, no significant correlation was found.
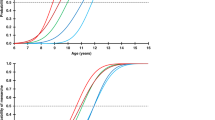
To elucidate the biologic function of the GHR c.1319 G>T polymorphism, plasmids with full-length GHR encoding either c.1319 G or T were transfected into CHO-k1 cells. LHRE was used as the GH response element. When cells were exposed to GH, GHR c.1319 T induced higher transcriptional activity of the GHR gene than GHR c.1319 G (Fig. 1). To our knowledge, this is the first report to compare the bioactivity of GHR c.1319 T and G in vitro. To understand the molecular mechanisms underlying the higher bioactivity of GHR c.1319 T, we performed Western blot analyses to analyze the phosphorylation of STAT-5 at Tyr694, which indicates the activation of STAT-5. As shown in Figure 2, the activation of STAT-5 was higher in GHR c.1319 T than in GHR c.1319 G, which explained the higher transcriptional activity of GHR c.1319 T.
Effects of GHR c.1319 G>T on LHRE-TK-SEAP induction. CHO cells were transfected with either pcGHR-T or pcGHR-G and LHRE-TK-SEAP and stimulated with either 50 or 100 ng/mL GH as indicated. Values are expressed as fold-induction relative to the basic activity of the unstimulated wells and represent the mean SEs of duplicate wells of three experiments. Paired-comparison t tests were conducted for GHR-TT vs GHR-GG. *p < 0.05; **p < 0.05.
Tyrosine phosphorylation of STAT-5 by GH in human GHR transfected CHO-k1 cells. (A) Cells were cultured in serum-free Dulbecco modified Eagle medium for 24 h and incubated with or without GH (100 ng/mL) for 30 min at 37°C. Whole cell lysates subjected to anti–phospho-STAT-5 (Tyr694) antibody (pY-STAT-5) for SD-PAGE and Western blot analysis. The same blot was stripped and then reprobed with anti–STAT-5 and anti-actin antibodies. (B) The blots were scanned by a densitometer. The pY-STAT-5 was normalized with actin and expressed as relative concentration. *p values for the paired comparisons GHR-TT vs GHR-GG were <0.05.
DISCUSSION
GH is the major regulator of postnatal body growth. Patients with GHD are usually affected with severe short stature. These patients often undergo GH replacement therapy; however, responsiveness to GH therapy varies from patient to patient because of genetic differences in the GH–IGF-I cascade among individuals. In the present study, we investigated 13 different genetic polymorphisms in the GH–IGF-I cascade that might affect growth velocity in prepubertal GHD patients who had undergone GH treatment for 1 y. We found that children with the GHR c.1319 T polymorphism showed statistically greater first-year growth velocity after 1 y of GH therapy than GHD children without that sequence variant. Furthermore, no correlation between the c.1319 G>T polymorphism and height was observed among individuals in the GHD, FSS, or control groups.
In 2004, Dos Santos et al. (6) demonstrated that children with the d3-GHR allele who were born SGA or had idiopathic short stature (ISS) grew taller than other GHD children after 1 y of GH therapy. Since then, several reports have been published that describe the influence of the d3-GHR allele on growth velocity in GHD patients. However, the findings are controversial. Jorge et al. (7) reported that GHD patients with the d3-GHR allele had more first-year growth velocity after GH treatment than GHD patients without that allele. However, Blum et al. (15), Hujeirat et al. (16) and Pilotta et al. (17) demonstrated that the presence of d3-GHR did not correlate with first-year growth velocity in GHD patients treated with GH. The reason for the discrepancy is unknown; however, it indicates that there may be other genetic factors that influence growth velocity in GHD patients after GH therapy.
Most of the children in our study group (70.8%) were homozygous for the GG genotype of the GHR c.1319 G>T polymorphism. Individuals with the T-related genotype (29.2%) obtained better growth velocity post–GH replacement than children who were homozygous for GG. The highest growth velocity was among the three individuals (1.9%) who carried the TT genotype. These children ranged in age from 7.5 to 8.8 y and comprised one girl and two boys. The three patients had growth velocities ranging from 9.8 cm to 13.5 cm, which is above the average gain in height of children with the GG and GT genotypes.
To elucidate the mechanism by which the GHR c.1319 T confers height gain, we conducted an assay of the reporter gene. The results showed that the homozygous TT genotype of the GHR c.1319 G>T polymorphism had higher transcriptional activity and stronger STAT-5 Tyr694 phosphorylation. It has been reported that phosphorylated JAK2 activates the STAT-1, -3, and -5 and the mitogen-activated protein kinase (MAPK) pathways, including Erk1/2, p38, and Jnk after GH stimulation (1–3). Therefore, we performed a Western blot analysis to analyze the tyrosine phosphorylation of JAK2; STAT-1, -3, and -5; Erk1/2; p38; and Jnk. There were no differences (data not shown) in tyrosine phosphorylation among these proteins, except for STAT-5.
The human GHR gene contains 10 exons. Exon 2 codes for a signal peptide and exons 3–7 code for the 246 amino acid extracellular domain. Exon 8 codes for the transmembrane domain, which contains a 24-amino-acid peptide, and exons 9 and 10 code for the 350-amino-acid cytoplasmic domain. The Cys440 residue located in exon 10 of the GHR gene, near Tyr469, a JAK2 kinase phosphorylation site, serves as docking site for STAT-5 (18,19). The nonsynonymous change of a cysteine to phenylalanine residue might interfere with the binding affinity of STAT-5 and further interfere with its phosphorylation. There are a total of nine Cys residues in the cytoplasmic domain of GHR. No reports have been published regarding the intramolecular bonds in the GHR c.1319 G>T polymorphism; therefore, we used two different programs [DISULFIND (20) and DiANNA 1.1(21)] to predict the disulfide bonding state. There are some differences in results generated between the two programs; however, they all showed that there is a disulfide bond between Cys425 and Cys440. The disrupted disulfide bond in c.1319 G may alter the binding affinity of SOCS-2 and result in a higher rate of STAT-5 phosphorylation.
Genetic studies have shown that SOCS proteins play important roles in growth and development. SOCS proteins are a family of negative regulatory proteins that are expressed in response to the activation of GH signal cascades, particularly the JAK/STAT signaling system (22). There are eight SOCS proteins (SOCS-1–SOCS-7 and a cytokine-inducible SH2 domain-containing protein), and some of these molecules have been shown to bind to and inhibit a number of cytokine/growth factor signaling molecules, including GH. For example, SOCS-2 was reported to interact with GHRs and act as a negative regulator of GH action. Furthermore, SOCS-2 knockout mice were shown to exhibit gigantism. SOCS-2 was reported to bind to phosphorylated Tyr487 and Tyr595 of the GHR; previously, it was shown that mutation of these two sites results in the prolongation of the GH-activated JAK/STAT-5 pathway (4). We found that there were no differences in protein expression levels of SOCS-2 between GHR c.1319 T and GHR c.1319 G in CHO-K1 cells (data not shown).
In conclusion, the heterozygous GT and the homozygous TT genotypes of the GHR c.1319 G>T polymorphism are associated with better first-year growth response to GH therapy. The homozygous TT genotype induced the highest transcriptional activity and strongest activation of STAT-5. This finding indicates that the GHR c.1319 G>T polymorphism might be a useful marker in pretreatment evaluation of GHD children. Once its role in growth velocity has been clarified, GHR c.1319 G>T polymorphism might prove to be a useful marker for predicting the future development of GH replacement therapy, thus permitting early therapeutic intervention in individuals with GHD.
Abbreviations
- ALS:
-
acid-labile subunit
- d3:
-
exon 3 retention or deletion
- FSS:
-
familial short stature
- GHD:
-
growth hormone deficiency
- GHR:
-
growth hormone receptor
- IGFBP:
-
insulinlike growth factor binding protein-3
- JAK:
-
Janus-activated kinase
- Jnk:
-
c-Jun N-terminal kinase
- LHRE:
-
lactogenic hormone response element
- SGA:
-
small for gestational age
- SNP:
-
single nucleotide polymorphism
- SOCS:
-
suppressor of cytokine signaling
- STAT:
-
signal transducers and activators of transcription
References
Thomas MJ 1998 The molecular basis of growth hormone action. Growth Horm IGF Res 8: 3–11
Herrington J, Carter-Su C 2001 Signaling pathways activated by the growth hormone receptor. Trends Endocrinol Metab 12: 252–257
Zhu T, Goh EL, Graichen R, Ling L, Lobie PE 2001 Signal transduction via the growth hormone receptor. Cell Signal 13: 599–616
Greenhalgh CJ, Rico-Bautista E, Lorentzon M, Thaus AL, Morgan PO, Willson TA, Zervoudakis P, Metcalf D, Street I, Nicola NA, Nash AD, Fabri LJ, Norstedt G, Ohlsson C, Flores-Morales A, Alexander WS, Hilton DJ 2005 SOCS2 negatively regulates growth hormone action in vitro and in vivo. J Clin Invest 115: 397–406
van der Lely AJ, Janssen JM, Lamberts SW 1998 Adult vs childhood onset GHD: is there a real clinical difference?. Growth Horm IGF Res 8:( Suppl A) 21–23
Dos Santos C, Essioux L, Teinturier C, Tauber M, Goffin V, Bougneres P 2004 A common polymorphism of the growth hormone receptor is associated with increased responsiveness to growth hormone. Nat Genet 36: 720–724
Jorge AA, Marchisotti FG, Montenegro LR, Carvalho LR, Mendonca BB, Arnhold IJ 2006 Growth hormone (GH) pharmacogenetics: influence of GH receptor exon 3 retention or deletion on first-year growth response and final height in patients with severe GH deficiency. J Clin Endocrinol Metab 91: 1076–1080
Gau SF, Soong WT, Tsai WY, Chiu YN 1997 A Chinese version of a self-administered ratings scale for pubertal development. Taiwanese J Psychiatry 11: 129–140
Chen W, Tsai C, Chen A, Wu S, Lin T, Lin H 2003 Growth charts of Taiwanese youth: norms based on health-related physical fitness. Mid Taiwan J Med 8: S85–S93
Greulich W, Pyle S 1959 Radiographic Atlas of Skeletal Development of the Hand and Wrist. Stanford University Press, Stanford, CA,
Pantel J, Machinis K, Sobrier ML, Duquesnoy P, Goossens M, Amselem S 2000 Species-specific alternative splice mimicry at the growth hormone receptor locus revealed by the lineage of retroelements during primate evolution. J Biol Chem 275: 18664–18669
Horan M, Newsway V, Yasmin Lewis MD, Easter TE, Rees DA, Mahto A, Millar DS, Procter AM, Scanlon MF, Wilkinson IB, Hall IP, Wheatley A, Blakey J, Bath PM, Cockcroft JR, Krawczak M, Cooper DN 2006 Genetic variation at the growth hormone (GH1) and growth hormone receptor (GHR) loci as a risk factor for hypertension and stroke. Hum Genet 119: 527–540
Audi L, Esteban C, Carrascosa A, Espadero R, Perez-Arroyo A, Arjona R, Clemente M, Wollmann H, Fryklund L, Parodi LA, Spanish SGA Study Group 2006 Exon 3-deleted/full-length growth hormone receptor polymorphism genotype frequencies in Spanish short small-for-gestational-age (SGA) children and adolescents (n = 247) and in an adult control population (n = 289) show increased fl/fl in short SGA. J Clin Endocrinol Metab 91: 5038–5043
Duquesnoy P, Sobrier ML, Amselem S, Goossens M 1991 Defective membrane expression of human growth hormone (GH) receptor causes Laron-type GH insensitivity syndrome. Proc Natl Acad Sci U S A 88: 10272–10276
Blum WF, Machinis K, Shavrikova EP, Keller A, Stobbe H, Pfaeffle RW, Amselem S 2006 The growth response to growth hormone (GH) treatment in children with isolated GH deficiency is independent of the presence of the exon 3-minus isoform of the GH receptor. J Clin Endocrinol Metab 91: 4171–4174
Hujeirat Y, Hess O, Shalev S, Tenenbaum-Rakover Y 2006 Growth hormone receptor sequence changes do not play a role in determining height in children with idiopathic short stature. Horm Res 65: 210–216
Pilotta A, Mella P, Filisetti M, Felappi B, Prandi E, Parrinello G, Notarangelo LD, Buzi F 2006 Common polymorphisms of the growth hormone (GH) receptor do not correlate with the growth response to exogenous recombinant human GH in GH-deficient children. J Clin Endocrinol Metab 91: 1178–1180
Waters MJ, Hoang HN, Fairlie DP, Pelekanos RA, Brown RJ 2006 New insights into growth hormone action. J Mol Endocrinol 36: 1–7
Wang X, Darus CJ, Xu BC, Kopchick JJ 1996 Identification of growth hormone receptor (GHR) tyrosine residues required for GHR phosphorylation and JAK2 and STAT5 activation. Mol Endocrinol 10: 1249–1260
Ceroni A, Passerini A, Vullo A, Frasconi P 2006 DISULFIND: a disulfide bonding state and cysteine connectivity prediction server. Nucleic Acids Res 34: W177–W181
Ferre F, Clote P 2005 DiANNA: a web server for disulfide connectivity prediction. Nucleic Acids Res 33: W230–W232
Rowland JE, Lichanska AM, Kerr LM, White M, d'Aniello EM, Maher SL, Brown R, Teasdale RD, Noakes PG, Waters MJ 2005 In vivo analysis of growth hormone receptor signaling domains and their associated transcripts. Mol Cell Biol 25: 66–77
Author information
Authors and Affiliations
Additional information
This work was supported by grants from the National Science Council (91-3112-B-039-001- and 92-3112-B-039-001-), Taipei, Taiwan, and a grant from China Medical University Hospital (DMR-96-111), Taichung, Taiwan.
Rights and permissions
About this article
Cite this article
Wan, L., Chen, WC., Tsai, Y. et al. Growth Hormone (GH) Receptor C.1319 G>T Polymorphism, But Not Exon 3 Retention or Deletion Is Associated With Better First-Year Growth Response to GH Therapy in Patients With GH Deficiency. Pediatr Res 62, 735–740 (2007). https://doi.org/10.1203/01.pdr.0000290803.86985.61
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.pdr.0000290803.86985.61
This article is cited by
-
Predicting Response to Growth Hormone Treatment
The Indian Journal of Pediatrics (2012)
-
Genetic causes and treatment of isolated growth hormone deficiency—an update
Nature Reviews Endocrinology (2010)