Abstract
Recent studies have identified abnormalities in the development and function of medullary serotonin (5-HT) pathways in postmortem brain from sudden infant death syndrome (SIDS) cases, suggesting 5-HT–mediated dysregulation of the autonomic nervous system (ANS) in SIDS. The human fifth Ewing variant (FEV) gene is specifically expressed in central 5-HT neurons in the brain, with a predicted role in specification and maintenance of serotonergic neuronal phenotype. We hypothesized that variations of FEV may underlie abnormalities of the 5-HT system in SIDS cases and thus may be associated with SIDS risk. To elucidate the relationship between variation in FEV and SIDS, DNA was prepared from 96 African American and Caucasian SIDS cases and 96 gender- and ethnicity-matched controls. Standard sequencing and analysis of FEV revealed a heterozygous insertion mutation (IVS-191_190insA) upstream of the 5′ exon 3 splice site occurring more frequently in SIDS cases (6/96) compared with controls (0/96; p = 0.01) and in the overall African American group (6/98) compared with the Caucasian group (0/94; p = 0.03). Identification of a variation in a gene responsible for 5-HT neuronal development, exclusively in a subset of African American SIDS cases in this cohort, may help explain both the observed abnormalities of this system in some SIDS cases and the ethnic disparity observed in SIDS.
Similar content being viewed by others
Main
The 5-HT system appears to be a key regulator of the ANS with important roles in cardiorespiratory control, thermoregulation, arousal, and sleep-wake cycling (1). Recent studies have identified abnormalities in the development and function of medullary 5-HT pathways in postmortem SIDS brains (2–5). These results indicate possible dysfunction in the differentiation and development of 5-HT neuronal networks in the medulla leading to disruption of the ANS and increased risk of SIDS.
Two functional polymorphisms associated with SIDS risk have been identified in the 5-HT transporter gene (SLC6A4, 5-HTT), known to regulate the duration and strength of interactions between 5-HT and its receptors. Narita et al. (6) initially demonstrated an association of a promoter polymorphism of SLC6A4 with risk of SIDS in the Japanese population. These results were subsequently confirmed in African American and Caucasian SIDS cases (7). Further, an intron 2 polymorphism of the SLC6A4 gene has been shown to increase SIDS risk in the African American population (8). Although these results begin to delineate the genetic mechanisms responsible for 5-HT–mediated dysregulation of the ANS in SIDS, the finding of diffuse differentiation and developmental abnormalities of the medullary 5-HT system suggests a genetic mechanism acting in the cascade of genes controlling 5-HT system development.
The transcriptional mechanisms leading to differentiation and development of the neuronal 5-HT system have been deciphered in recent studies (9–14). These studies identified a Sonic hedgehog (Shh)–regulated series of transcription factors working in concert to specify 5-HT neurotransmitter phenotype in a subset of neurons, specifically identifying the mouse ETS family transcription factor Pet1 (15–20) as necessary for terminal induction of 5-HT neurons. Pet1 is expressed in the central 5-HT system, and the onset of Pet1 expression consistently precedes the appearance of 5-HT by 0.5 d (15). It seems that Pet1 not only establishes and maintains the serotonergic phenotype, it also interacts with the regulatory regions of genes whose expression is characteristic of the serotonergic phenotype including the SLC6A4, 5-HT1a receptor, tryptophan hydroxylase, and aromatic l-amino acid decarboxylase genes (15). Nearly all 5-HT neurons fail to differentiate in mice lacking Pet1, and the remaining neurons exhibit deficient expression of genes required for 5-HT synthesis, uptake, and vesicular storage (16). The FEV gene, located on chromosome 2, is the human homologue of Pet1. Based on its high (96%) sequence similarity to the predicted mouse Pet1 gene (19,20) and its similar restricted expression pattern in the 5-HT system (17,18), a similar function for FEV in the differentiation and development of the human 5-HT neuronal phenotype is predicted.
The Pet1 gene is the only known transcription factor whose brain expression is limited to developing and adult 5-HT neurons. Recently, a 1.8-kb 5′ region immediately upstream of the Pet1 coding region was demonstrated to be necessary and sufficient to cause 5-HT neuron–specific expression of Pet1 (21). This region shows 70%–90% sequence identity with the human FEV gene and is therefore expected to play a similar role of specifying FEV expression to 5-HT neurons in the human brain.
Extensive abnormalities of the medullary 5-HT system have been identified in SIDS cases, suggesting a failure of transcriptional mechanisms that control differentiation and development of this system. Thus, genes involved in the transcriptional cascade that defines serotonergic system differentiation and development can be viewed as candidate genes for contribution to SIDS risk. Because FEV specifically interacts with the SLC6A4 promoter, already implicated in SIDS risk, and has been predicted to play an integral role in 5-HT neuronal differentiation, FEV was hypothesized to be a likely candidate gene for contribution to SIDS etiology. This study examined the coding regions, intron-exon boundaries, and 2-kb 5′ upstream region of the FEV gene in a cohort of SIDS cases and matched controls.
METHODS
Study population.
Two distinct groups were investigated in this study: 96 SIDS cases and 96 control subjects matched for gender and ethnicity, a subset of which (91/96) was included in previous publications (7,8,22–24). SIDS cases (mean age at death, 95 ± 52 d; median age, 85 d; 25th and 75th percentiles: 56 and 111 d, respectively) were collected in the University of Maryland Brain and Tissue Bank (23 African American females, 26 African American males, 17 Caucasian females, and 30 Caucasian males). The diagnosis of SIDS was based on the accepted definition (25). With informed consent, unrelated control subjects were matched for ethnicity and gender to SIDS cases with a 1:1 match ratio. A three-generation family history was taken for each control to ensure that no family member had a diagnosis of SIDS, Hirschsprung disease, congenital central hypoventilation syndrome, apparent life-threatening event, primary (nonacquired) ANS dysregulation, or tumor of neural crest origin. This study was approved by the Rush University Institutional Review Board.
DNA preparation and sequence analysis.
Genomic DNA was isolated from frozen frontal cortex (SIDS cases) or blood samples (controls) using standard methods (7). All coding regions, intron-exon boundaries, and the 2-kb 5′ region immediately upstream of the FEV gene were amplified by polymerase chain reaction (PCR) using primer pairs 5′-AAGATGCAGATA ACGCAGCCTGGA-3′ (forward) and 5′-CATTACAATCGGCCCTCC ATGCAA-3′ (reverse) for exon 1; 5′-TCCTGACTTGGGCTCTATGG-3′ (forward) and 5′-CTTGGCCTGCAACTCTTTTC-3′ (reverse) for exon 2; 5′-AGTGGAAGCCGCATTTCCATTGTG-3′ (forward) and 5′- ACCAG ACAAGGATTGAGGGAGCTT-3′ (reverse) for exon 3; and 5′-AAC TAGAACCCAGGCAAACTGGCT-3′ (forward) and 5′-CGTCCCATCG CAATAAAGTCTCCA-3′ (reverse) for the upstream region. Exons 1 and 3, and the 5′ upstream region were amplified using the GC-RICH system (Roche Molecular Biochemicals, Indianapolis, IN) in 50 μL containing 50 ng genomic DNA, 0.5 μM primers, 5 μL of 5M GC-RICH resolution solution, 10 μL of 5× GC-RICH reaction buffer, 0.2 μM deoxyribonucleoside triphosphate (dNTPs), and 2 U of Taq. Amplification was performed with an initial denaturation at 95°C for 8 min, 35 cycles at 95°C for 1 min, 60°C for 1 min, and 72°C for 1 min (1 min 30 s for the upstream region) with a final extension at 72°C for 10 min. Samples identified as containing an insertion in intron 2 using the primers above, as well as the matched controls of these samples, were amplified again using primer pair 5′-TATCTGTCCTTGCTCGCCTTGGAA-3′ (forward) and 5′-ACCAGA CAAGGATTGAGGGAGCTT-3′ (reverse) following the above protocol. Exon 2 was amplified in 50 μL containing 50 ng genomic DNA, 5 μL 10× buffer, 1.5 μM MgCl2, 0.2 μM dNTPs, 0.5 μM primers, and 1.5U Taq (Invitrogen Corporation, Carlsbad, CA). Amplification was carried out using an initial denaturation of 94°C for 5 min, 35 cycles at 94°C for 1 min, 55°C for 1 min, and 72°C for 1 min, and a final elongation of 72°C for 10 min. All products were purified using the Millipore Montage Cleanup Kit (Millipore, Billerica, MA) according to the manufacturer's instructions and visualized by running 5 μL of product on 1% agarose gels. Purified products were sequenced directly on an ABI PRISM 3100 Genetic Analyzer (Applied Biosystems, Foster City, CA). PCR and sequencing of all samples with sequence variations were repeated, using both forward and reverse primers, and were manually reviewed by multiple experienced individuals to ensure accuracy of variant identification.
Statistical analysis.
Allele frequencies were compared using χ2 tests. The number of index alleles in each case was compared with the number in the matching control by Wilcoxon signed-rank tests. The genotype frequencies were compared using the Cochran-Mantel-Haenszel test applied to paired data. Statistical significance was set at α = 0.05.
RESULTS
FEV sequence analysis in SIDS cases and control subjects.
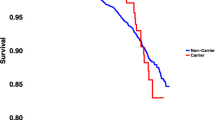
A previously unidentified heterozygous insertion mutation (IVS2-191_190insA) was observed in intron 2 of the FEV gene (Fig. 1) 190 base pairs upstream of the 5′ exon 3 splice site. The genotype distribution of this mutation differed significantly between SIDS cases and control subjects (p = 0.01) with the IVS2-191_190insA genotype being identified in six of 96 SIDS cases compared with zero of 96 control samples. Ethnic distribution variation was apparent as this mutation was identified significantly more frequently in the African American population (6/98) than the Caucasian population (0/94; p = 0.03).
Variations identified in the FEV gene in 96 SIDS cases and 96 matched controls. Schematic illustration of variations identified in the FEV gene in this cohort of 96 SIDS cases and 96 matched controls. Location of the three polymorphisms (IVS2-37C>G, c357C>T, and c*61G>T) identified in or near exon 3 of FEV in both SIDS cases and matched controls is indicated. The location of the IVS-191_190insA variation, found exclusively in African American SIDS cases in this cohort, is shown. Representation of the variant DNA sequence compared with the wild-type DNA sequence is also provided.
Three polymorphisms were identified in or near exon 3 of FEV in both SIDS cases and matched controls: IVS2-37C>G (rs452985), c357C>T (rs860573), and c*61G>T (rs2301296) (9/96 versus 5/96, 10/96 versus 11/96, 5/96 versus 10/96; SIDS variant genotypes versus control variant genotypes, respectively; Fig. 1). No association between these variations, either alone or when considered in combination, and SIDS was identified. However, there were significantly more African American cases and controls (21/98) presenting with one or more of these FEV polymorphisms compared with the Caucasian subjects (6/94; p = 0.003). No variations were identified in FEV upstream of intron 2 in either SIDS cases or controls.
DISCUSSION
Evidence is growing indicating dysfunction of the serotonergic system in the pathway leading to autonomic dysregulation and vulnerability to SIDS (2–8,26,27). The focus of this study, the ETS domain transcription factor FEV, has been predicted to play a role in the development and maintenance of the serotonergic system as a regulator of 5-HT neuronal differentiation (15–18) based on its high sequence similarity to the mouse Pet1 gene (19,20) and its restricted expression pattern in the 5-HT system of the human brain (17,18). Analysis of the FEV gene in SIDS cases and matched controls revealed an intronic insertion mutation, IVS2-191_190insA, upstream of the third FEV exon found exclusively in SIDS cases in the cohort presented here. The SIDS-specific mutation identified in this study is located outside the amino acid coding region and does not appear, through branch point analysis, to be involved in splicing. However, it is possible that this variation may exert its effects through additional regulatory means. Although the limited sample size of cases presenting with the IVS2-191_190insA genotype in this study precludes gene-interaction studies, it is possible that this mutation may be acting in combination with variations identified in SLC6A4 or other, yet unidentified, variations in genes involved in 5-HT system development. In this cohort, the IVS2-191_190insA mutation was specific to the African American population, whereas other polymorphisms in the FEV gene were increased in the African American group, likely reflective of the increased genetic variability expected in populations of African descent. Nonetheless, the prevalence of this mutation in the African American population may relate to the increased risk of SIDS in this population.
Identification of a mutation expressed exclusively in SIDS cases in a transcriptional regulator thought to be responsible for terminal 5-HT differentiation may relate to abnormalities observed in the 5-HT system in some SIDS cases. Although this study represents the first report of a mutation in the 5-HT neuronal differentiation cascade associated with SIDS risk, it does not uncover a specific pathogenetic mechanism associated with the mutation. Functional studies examining the effects of this mutation on FEV transcriptional activity and on 5-HT neuronal development were unavailable in this study due to lack of SIDS tissue from which quality RNA samples could be obtained. In vitro analysis of the role of this mutation will be required to establish molecular pathogenesis and determine how this mutation relates to disease risk.
CONCLUSIONS
In summary, the present study identifies an intronic insertion mutation in the FEV gene, which is found more commonly in SIDS cases, specifically African American SIDS cases, than controls and may be present exclusively in SIDS cases. Studies of this mutation in a larger cohort of SIDS cases and matched controls to assess the effect of interaction between variants in the 5-HT system genes on SIDS risk are indicated, as are functional analyses to ascertain the possible pathogenetic mechanism associated with the mutation.
Abbreviations
- 5-HT:
-
serotonin
- ANS:
-
autonomic nervous system
- FEV:
-
fifth Ewing variant
- SLC6A4:
-
serotonin transporter gene
References
Jacobs BL, Azmitia EC 1992 Structure and function of the brain serotonin system. Physiol Rev 72: 165–229
Kinney HC, Randall LL, Sleeper LA, Willinger M, Belliveau RA, Zec N, Rava LA, Dominici L, Iyasu S, Randall B, Habbe D, Wilson H, Mandell F, McClain M, Welty TK 2003 Serotonergic brainstem abnormalities in Northern Plains Indians with the sudden infant death syndrome. J Neuropathol Exp Neurol 62: 1178–1191
Ozawa Y, Okado N 2002 Alteration of serotonergic receptors in the brain stems of human patients with respiratory disorders. Neuropediatrics 33: 142–149
Panigrahy A, Filiano J, Sleeper LA, Mandell F, Valdes-Dapena M, Krous HF, Rava LA, Foley E, White WF, Kinney HC 2000 Decreased serotonergic receptor binding in rhombic lip-derived regions of the medulla oblongata in the sudden infant death syndrome. J Neuropathol Exp Neurol 59: 377–384
Paterson DS, Trachtenberg FL, Thompson EG, Belliveau RA, Beggs AH, Darnall R, Chadwick AE, Krous HF, Kinney HC 2006 Multiple serotonergic brainstem abnormalities in sudden infant death syndrome. JAMA 296: 2124–2132
Narita N, Narita M, Takashima S, Nakayama M, Nagai T, Okado N 2001 Serotonin transporter gene variation is a risk factor for sudden infant death syndrome in the Japanese population. Pediatrics 107: 690–692
Weese-Mayer DE, Berry-Kravis EM, Maher BS, Silvestri JM, Curran ME, Marazita ML 2003 Sudden infant death syndrome: association with a promoter polymorphism of the serotonin transporter gene. Am J Med Genet A 117: 268–274
Weese-Mayer DE, Zhou L, Berry-Kravis EM, Maher BS, Silvestri JM, Marazita ML 2003 Association of the serotonin transporter gene with sudden infant death syndrome: a haplotype analysis. Am J Med Genet A 122: 238–245
Cheng L, Chen CL, Luo P, Tan M, Qiu M, Johnson R, Ma Q 2003 Lmx1b, Pet-1, and Nkx2.2 coordinately specify serotonergic neurotransmitter phenotype. J Neurosci 23: 9961–9967
Craven SE, Lim KC, Ye W, Engel JD, de Sauvage F, Rosenthal A 2004 Gata2 specifies serotonergic neurons downstream of sonic hedgehog. Development 131: 1165–1173
Ding YQ, Marklund U, Yuan W, Yin J, Wegman L, Ericson J, Deneris E, Johnson RL, Chen ZF 2003 Lmx1b is essential for the development of serotonergic neurons. Nat Neurosci 6: 933–938
Pattyn A, Simplicio N, van Doorninck JH, Goridis C, Guillemot F, Brunet JF 2004 Ascl1/Mash1 is required for the development of central serotonergic neurons. Nat Neurosci 7: 589–595
Zhao ZQ, Scott M, Chiechio S, Wang JS, Renner KJ, Gereau RW 4th, Johnson RL, Deneris ES, Chen ZF 2006 Lmx1b is required for maintenance of central serotonergic neurons and mice lacking central serotonergic system exhibit normal locomotor activity. J Neurosci 26: 12781–12788
van Doorninck JH, van Der Wees J, Karis A, Goedknegt E, Engel JD, Coesmans M, Rutteman M, Grosveld F, De Zeeuw CI 1999 GATA-3 is involved in the development of serotonergic neurons in the caudal raphe nuclei. J Neurosci 19: RC12
Hendricks T, Francis N, Fyodorov D, Deneris ES 1999 The ETS domain factor Pet-1 is an early and precise marker of central serotonin neurons and interacts with a conserved element in serotonergic genes. J Neurosci 19: 10348–10356
Hendricks TJ, Fyodorov DV, Wegman LJ, Lelutiu NB, Pehek EA, Yamamoto B, Silver J, Weeber EJ, Sweatt JD, Deneris ES 2003 Pet-1 ETS gene plays a critical role in 5-HT neuron development and is required for normal anxiety-like and aggressive behavior. Neuron 37: 233–247
Iyo AH, Porter B, Deneris ES, Austin MC 2005 Regional distribution and cellular localization of the ETS-domain transcription factor, FEV, mRNA in the human postmortem brain. Synapse 57: 223–228
Maurer P, Rorive S, de Kerchove d'Exaerde A, Schiffmann SN, Salmon I, de Launoit Y 2004 The Ets transcription factor Fev is specifically expressed in the human central serotonergic neurons. Neurosci Lett 357: 215–218
Peter M, Couturier J, Pacquement H, Michon J, Thomas G, Magdelenat H, Delattre O 1997 A new member of the ETS family fused to EWS in Ewing tumors. Oncogene 14: 1159–1164
Pfaar H, von Holst A, Vogt Weisenhorn DM, Brodski C, Guimera J, Wurst W 2002 mPet-1, a mouse ETS-domain transcription factor, is expressed in central serotonergic neurons. Dev Genes Evol 212: 43–46
Scott MM, Krueger KC, Deneris ES 2005 A differentially autoregulated Pet-1 enhancer region is a critical target of the transcriptional cascade that governs serotonin neuron development. J Neurosci 25: 2628–2636
Weese-Mayer DE, Berry-Kravis EM, Zhou L, Maher BS, Curran ME, Silvestri JM, Marazita ML 2004 Sudden infant death syndrome: case-control frequency differences at genes pertinent to early autonomic nervous system embryologic development. Pediatr Res 56: 391–395
Maher BS, Marazita ML, Rand C, Zhou L, Berry-Kravis EM, Weese-Mayer DE 2006 3′ UTR polymorphism of the serotonin transporter gene and sudden infant death syndrome: haplotype analysis. Am J Med Genet A 140: 1453–1457
Rand CM, Weese-Mayer DE, Zhou L, Maher BS, Cooper ME, Marazita ML, Berry-Kravis EM 2006 Sudden infant death syndrome: case-control frequency differences in paired like homeobox (PHOX) 2B gene. Am J Med Genet A 140: 1687–1691
Willinger M, James LS, Catz C 1991 Defining the sudden infant death syndrome (SIDS): deliberations of an expert panel convened by the National Institute of Child Health and Human Development. Pediatr Pathol 11: 677–684
Kinney HC, Filiano JJ, White WF 2001 Medullary serotonergic network deficiency in the sudden infant death syndrome: review of a 15-year study of a single dataset. J Neuropathol Exp Neurol 60: 228–247
Kinney HC, Myers MM, Belliveau RA, Randall LL, Trachtenberg FL, Fingers ST, Youngman M, Habbe D, Fifer WP 2005 Subtle autonomic and respiratory dysfunction in sudden infant death syndrome associated with serotonergic brainstem abnormalities: a case report. J Neuropathol Exp Neurol 64: 689–694
Acknowledgements
The authors thank the parents of the SIDS cases for their gracious tissue donations, as well as the control subjects who shared their DNA. Sue E. Leurgans Ph.D., is gratefully acknowledged for her help in statistical design and analysis and in revision of the article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Extramural support: Spastic Paralysis and Allied Diseases of the Central Nervous System Research Foundation of the Illinois-Eastern Iowa District Kiwanis International (E.M.B.-K.). CJ Foundation for SIDS, Justin Carl Suth SIDS Research Fund, Joseph Tyler Gertler SIDS Research Fund, the NICHD-Funded University of Maryland Brain & Tissue Bank, and the Scottish Cot Death Trust (D.E.W.-M.).
Rights and permissions
About this article
Cite this article
Rand, C., Berry-Kravis, E., Zhou, L. et al. Sudden Infant Death Syndrome: Rare Mutation in the Serotonin System FEV Gene. Pediatr Res 62, 180–182 (2007). https://doi.org/10.1203/PDR.0b013e3180a725a0
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3180a725a0
This article is cited by
-
Sudden and unexpected death in early life: proceedings of a symposium in honor of Dr. Henry F. Krous
Forensic Science, Medicine, and Pathology (2012)
-
Gene variants predisposing to SIDS: current knowledge
Forensic Science, Medicine, and Pathology (2011)
-
“Smothered” Infants—Neglect, Infanticide or SIDS? A Fresh Look at the 19th Century Mortality Schedules
Human Ecology (2009)
-
Transcriptional repression coordinates the temporal switch from motor to serotonergic neurogenesis
Nature Neuroscience (2007)