Abstract
Neonatal dexamethasone (DEX) for chronic lung disease is associated with adverse outcome. We compared behavioral and motor development at school age of children who neonatally received DEX to children neonatally treated with hydrocortisone (HC) in a retrospective matched cohort study. DEX- and HC-treated groups matched for gestational age, birth weight and year, gender, and severity of respiratory distress syndrome were compared with a reference group (REF) and a group treated only antenatally with betamethasone (BMETH). REF and BMETH groups had a higher gestational age and less severe respiratory distress syndrome. From 192 children (DEX, n = 46; HC, n = 52; REF, n = 43; BMETH, n = 51), the Child Behavioral Checklists from parents and teachers (Teacher's Report Form) and the Movement Assessment Battery for Children to assess neuromotor function were analyzed. DEX girls had a poorer performance on nearly all behavioral scales of the Teacher's Report Form compared with HC girls. DEX boys did not differ from HC boys. The HC boys or girls did not differ from the REF or BMETH groups. Neuromotor development was poorer in DEX than the BMETH and REF groups. The HC group did not differ from REF and BMETH groups. We suggest that neonatal HC may be a “safer” alternative for DEX for the treatment of CLD.
Similar content being viewed by others
Main
Several studies have reported long-term adverse effects of neonatal DEX therapy for CLD on cognitive and motor development (1–3). A recent randomized double-blind trial of Yeh et al. (4) including 146 children revealed that early postnatal DEX treatment was associated with adverse effects on neuromotor and cognitive functions at school age. Because there is increasing evidence of long-term adverse side effects, clinicians have become more reluctant to use GC therapy in preterms at risk for CLD (5–7). However, because GC significantly decreases the incidence of CLD, it may be useful in some circumstances and further investigation of the use of GC in CLD seems mandatory to reduce severe CLD (8,9). Despite suggestions to use less potent GC such as HC (10,11), DEX is still the most frequently used GC in preterm CLD (2,12). Our neonatal intensive care unit (NICU) is one of the few NICU centers that uses HC for prevention of CLD. We recently reported the results of a small retrospective study in which we compared neonatally HC-treated children of our own NICU with DEX-treated children admitted to another Dutch NICU. We found no difference in clinical efficacy (reduction of extra oxygen need and weaning from the ventilator) between HC and DEX, but found that DEX-treated children had an inferior school performance at 5–7 y of age compared with HC-treated children (13).
We therefore hypothesize that neonatal GC treatment for prevention or reduction of CLD with HC is a safe alternative for DEX regarding behavioral performance and motor developmental outcome. We therefore investigated behavioral and motor development at school age (7–10 y of age) in a retrospective matched cohort of four groups: 1) a reference group not treated with GCs either prenatally or postnatally; 2) a group treated with prenatal BMETH only; 3) a study group treated with DEX; and 4) a study group treated with HC. Although we tried to match the REF and the BMETH groups with the HC and DEX groups, this was not possible for gestational age and severity of infant respiratory distress syndrome. The REF and BMETH groups were more mature and heavier at birth and had less severe respiratory distress syndrome. The BMETH group was included because most of the children who received neonatal GC treatment had also been exposed to BMETH antenatally. This allowed us to assess the separate effect of BMETH antenatally.
PATIENTS AND METHODS
The study population of this retrospective matched cohort study consisted of prematurely born infants admitted between December 1993 and July 1997 to the NICUs of the University Medical Centre/Wilhelmina Children's Hospital Utrecht, the Leiden University Medical Centre, the Free University Medical Centre Amsterdam, and the Isala Clinics Zwolle in the Netherlands. The study was approved by the Medical Ethics Committee of the University Medical Centre/Wilhelmina Children's Hospital Utrecht and the Scientific Boards of the four participating Hospitals. Written parental consent was always obtained. The NICU of the University Medical Centre/Wilhelmina Children's Hospital Utrecht exclusively used HC therapy to reduce CLD in a course starting with 5 mg/kg/d and tapering off to 1 mg/kg/d over a 22-d period, whereas the other NICUs used a course of DEX for this purpose, starting with 0.5 mg/kg/d and tapering off to 0.1 mg/kg/d over a 21-d period. In all centers, the course was sometimes extended or shortened, depending on the response and side-effects of therapy. Treatment indication in the respective hospitals was in all instances the impossibility to wean the infant from the ventilator together with prolonged dependency on extra continuous oxygen, based on the initial phase of CLD. In addition to these two neonatal GC groups, a group of antenatally BMETH-treated preterm born infants (12 mg intramuscularly, given to the mother twice, with an interval of 24 h, the last dose being administered at least 12 h antepartum) and a REF group of preterm infants who did not receive ante- or neonatal GC was added for comparison to fetuses and infants perinatally treated with GCs.
Study groups.
Eligibility for inclusion in one of the study groups was as follows: 1) surviving the neonatal period; 2) availability to participate in the study protocol as indicated below; 3) neonatal cerebral ultrasound showing maximal a grade II periventricular hemorrhage as classified according to Papile et al. (14); and 4) absence of major congenital anomalies. Infants with cystic periventricular leukomalacia diagnosed before the start of GC-treatment were also excluded. With 52 children in each group, it should be possible to detect a mean group difference of 45% in the total child behavioral checklist (see below), assuming an α (2-sided) of 0.05 and power of 0.80. The HC and DEX groups were composed as follows: The charts of all consecutively admitted preterm infants born after less than 32 completed weeks of pregnancy in the respective participating NICUs were systematically reviewed. From the NICU of the Wilhelmina Children's hospital, in which only hydrocortisone was used, 131 infants meeting the entry criteria were treated with HC during the defined period of time. The DEX group, recruited in a similar way as the other three NICUs, which used only DEX for reduction of CLD, consisted of 198 eligible infants. To better ensure that possible differences in outcome between HC- and DEX-treated babies were related to the different choice of GC and not to differences in clinical management between the hospitals, we looked for gestational age, inborn/outborn ratio, periventricular/intraventricular hemorrhage (grade I, II), postnatal age at the start of GC treatment, incidence of neonatal sepsis, and necrotizing enterocolitis between the selected HC and DEX children. No difference was found between the groups for any variable. Ultimately, we were able to reliably match 52 individuals from the HC group and 52 from the DEX group for gestational age, birth weight, gender, severity of infant respiratory distress syndrome [classified as no, moderate or severe RDS according to clinical symptoms and the Giedeon classification (15)], whether or not a minor periventricular/intraventricular hemorrhage (grade I and II) existed and the year of birth. The 52 selected HC children in this study did not significantly differ from the 79 nonselected HC children for gestational age, birth weight, gender, severity of infant respiratory distress syndrome, the incidence of periventricular/intraventricular hemorrhage (grade I and II), or postnatal age at the start of GC treatment. This was also true for the 52 children of the DEX cohort versus the 146 nonselected DEX children. Also, the incidence of prenatal GC did not differ between included and nonincluded HC or DEX children.
Fifty-two participants in the antenatally BMETH-treated group and the 52 in the REF group were also recruited from the four participating NICUs. The REF and BMETH groups consisted of prematurely born babies who were not treated postnatally with glucocorticoids, did not have periventricular leukomalacia or major peri-/intraventricular hemorrhage (grade III or more) and no other major complications during the neonatal period. Although we tried to match these latter two groups for gestational age and birth weight with a DEX-HC-couple, this was not always possible. Also, severity of respiratory distress syndrome was less in the REF and BMETH groups.
Study protocol.
To eliminate interobserver variability, one follow-up team evaluated all study patients. The team consisted of a neonatologist, a researcher, and a research nurse. The researcher was supervised by the neonatologist and educated before the start of the study to perform a medical evaluation including weight, length, blood pressure, a short orientating neurologic examination that was classified as either normal, minor abnormalities or abnormal (e.g., cerebral palsy), and to take the Movement Assessment Battery for Children to assess motor function (see also below). The follow-up team was unaware in which group the child was participating. For this occasion, the participating children were invited to visit the Wilhelmina Children's Hospital accompanied by at least one parent.
Behavioral performance at school age.
For this purpose, the Child Behavioral Checklist (CBCL) for ages 4–18 y was used (16) and should be completed by the mother and the father. The list consists of 118 items recalling behavioral problems that can be scored on a 3-point or a 2-point scale. Items include internalizing (somatic complaints, anxiety and depression) and externalizing [delinquent (i.e. rule-breaking) and aggressive] behavior, social problems, and thought and attention problems. There is a total score available in this test for behavioral problems. The teachers of the participants of the present study were asked to fill out the Teacher's Report Form (TRF), which consists, like the CBCL, of 120 items related to the above mentioned problems. The scales of the TRF items are similar to those of the CBCL, as is also the case with the total score. Additionally, data were gathered with respect to the educational status of mother and father.
Assessment of neurologic and motor functions.
The ABC Movement was used to assess functional motor skills. The ABC Movement consists of four scales, i.e. manual dexterity (function of one hand, coordination of two hands, hand-eye coordination), ball skills (one-hand bounce, ball in box), static (balance task) and dynamic balance (capacity to perform quick and brisk movements, slow movement, heel-to-toe walking), and the total motor impairment score (17). Manual dexterity measures subtle motor function; ball skills measure subtle and gross motor function; static and dynamic balance measures gross motor function. For each task, a score is given for performance, partly depending on age. The total impairment score is the sum of all scores; the lower the score, the better the performance.
Statistical analysis.
Data are summarized as mean ± SD or as median and ranges where appropriate. Differences in clinical data, important general follow-up data of the children and of the social economic status of mother and father were compared with one factorial ANOVA, followed by a posthoc Bonferroni test if a significant difference was detected, or χ2 test when categorical variables were compared.
To investigate the treatment effect on behavior at 7–10 y of age, an ANCOVA was done in which treatment and gender were included as independent factors and the different scores of the CBCL as dependent variables, followed by a posthoc Bonferroni test. Because gestational age and birth weight were different between DEX and HC groups on the one hand and antenatal BMETH and REF groups on the other (see Results), this procedure was corrected for gestational age. Age on the day of testing was also used as a covariate. For a more detailed assessment of possible differences between boys and girls, a separate ANCOVA was performed for boys and girls.
To investigate the difference in behavioral problems between the four groups, we applied a χ2 test to test the assumption of equality of percentages of children above or under the clinical cut-off score in the four groups in which the T-score was used (cut-off point: 67, and for internalizing, externalizing and total score: 60; see also Achenbach (16).
Special education between the treatment groups and/or between boys and girls was compared with a χ2 test for all studied children together and also separately for boys and girls.
To investigate possible differences between groups with respect to motor development, ANCOVA was used with group and gender as independent variable and the score on the different ABC Movement scales as dependent variable, with the posthoc Bonferroni test. Again, this analysis was corrected for gestational age and age on the day of testing.
All statistical analysis was performed using SPSS 12.0.1 (SPSS Inc., Chicago, IL). Statistical significance was assumed for p < 0.05.
RESULTS
Two hundred and eight children, born after a pregnancy of less than 32 wk, were initially recruited for the study. Eventually, 192 children (DEX, n = 46; HC, n = 52; BMETH, n = 51; REF, n = 43) participated in behavioral part of the study (CBCL/TRF questionnaires). The total number of children participating in the ABC Movement test was 191 (one child from the DEX group could not participate because he was wheelchair-bound). Figure 1 shows the flow from enrollment to follow-up at 7–10 y of age.
Clinical perinatal and follow-up data.
Perinatal and neonatal general characteristics are summarized in Table 1. The DEX and HC group were comparable for all measures, the REF and BMETH-groups were larger, more mature, and less ill.
The general characteristics of the children at follow-up age are provided in Table 2. When measurements were corrected for age at measurement, the neonatally DEX-treated children were comparable in body weight, head circumference, and height to the other three groups. No differences in blood pressure (measured at rest) were detected between groups.
Assessment of behavioral problems and school performance with the CBCL and TRF.
The CBCL scores were similar between groups, however, TRF scores were significantly higher in the DEX-treated girls compared with the girls in all other groups. For boys there were no group differences. Analysis of the TRF subscales showed that girls from the DEX-group had significantly more social problems, attention problems, internalizing behavior (withdrawn behavior) or externalizing (delinquent and aggressive) behavior and general behavioral problems compared with the other groups (Fig. 2). For internalizing behavior, DEX-girls only differed from REF-girls, but not from HC- or BMETH-girls (Fig. 1). The boys and girls in the HC group did not differ from the boys and girls in the BMETH or REF group for any of the TRF items. Due to the small number of children that did not receive BMETH prenatally in both the DEX and HC groups (see Table 1, >70% were BMETH-treated in each group), we could not reliably perform a subanalysis of the difference between children that were and were not prenatally treated with BMETH in these groups.
Scores (box and whisker plots) of CBCL (TRF) of (A) social problems, (B) attention problems and (C) internalizing, (D) externalizing behavior, and (E) total problem score as functions of neonatal DEX (n = 46) or HC (n = 52) treatment, antenatal BMETH (n = 51) treatment or no treatment at all (REF, n = 43). Results are given in box plots with median and interquartile ranges, separately for girls (shaded bars) and boys (open bars). Arrowheads indicate significant gender differences between the girls of the treatment groups; the boys do not significantly differ from each other. *p < 0.05; **p < 0.01.
As expected, the CBCL showed important differences between sexes in general. CBCL data from the mother showed more concentration problems (p < 0.05), externalizing behavior (p < 0.01 and p < 0.05) and sexual problems (p < 0.05) in boys compared with girls. Externalizing behavior was also significantly different between sexes in the CBCL data of the father: (aggressive and offensive behavior; p < 0.01 and p < 0.05). The TRF showed more concentration problems (p < 0.01), and externalizing behavior (p < 0.01) in boys compared with girls.
When examining differences between groups for behavioral problems according to clinical cut-off values used for the CBCL, no differences were found between groups when relying on the CBCL filled out by father and mother. However, the TRF showed a significantly higher percentage of children in the DEX group with internalizing behavioral problems according to clinical criteria compared with the other groups (p < 0.05).
With respect to the effect of medication on the type of school education we relied on the medical history taken by the researcher on the day of hospital visit, where questions about parental and child education were included. It appeared that children treated with DEX needed significantly more often a school for special education (p < 0.05). Also, the boys showed a clear tendency for the need of special education (Table 2). In this study, there seemed to be no clear relation between the education of the mother and marital status on the one hand and the need for special education on the other hand.
Neurologic examination and assessment of motor function.
As summarized in Table 3, no differences were detected between groups with respect to the results of the neurologic evaluation, although there is a clear trend for abnormal neurologic examination in the DEX group (p < 0.095).
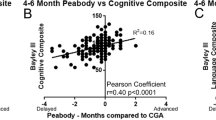
In contrast to the behavioral parameters, we did not observe a difference in motor performance between the sexes (p = 0.974) or an interaction between treatment and sex. Although there was no significant difference between the HC and DEX groups, the children of the DEX group had a higher total impairment score than the REF and BMETH groups (p < 0.01), indicating an overall poorer performance of the DEX group. No significant differences were detected between the HC group and the BMETH or REF group. When analyzing the subscales of the ABC Movement test, the DEX group scored worse on manual dexterity (versus BMETH group: p < 0.05), on ball skills (versus REF and BMETH groups: p < 0.001), and on static and dynamic balance (versus REF group: p < 0.01). The HC group scored significantly worse than the REF group only on the item ball skills: p < 0.05). The results of the total impairment score (TIS) derived from the ABC Movement test.
DISCUSSION
In this study, we found that infants treated postnatally with HC had a similar cognitive and motor neurodevelopmental outcome as a non-GC-treated REF group, whereas postnatally DEX-treated children did worse compared with the REF group, in particular the girls.
There is increasing evidence that the use of DEX in preterm infants has adverse effects on long-term somatic (18,19), cognitive (2,4), and neuromotor development (2,8). For this reason, the American Academy of Pediatrics and the Canadian Paediatric Society advised to limit neonatal GC therapy to exceptional situations (5). However, despite the potential dangers of neonatal DEX therapy, in some circumstances the use of GC is may be the lesser of two evils (9). One alternative may be HC, which has a shorter half life, thus reducing the possibility of drug accumulation. We previously documented that HC had a similar clinical effect as to DEX at a lower equivalent dose (13).
We observed group differences for the TRF but not for the parent ratings on the behavior of the children with the CBCL. Despite the fact that the naming of the subscales suggests that the same behavioral traits are assessed, this may not be entirely the case. An earlier review of the literature by Achenbach et al. (21) showed the correlations between TRF and CBCL to be low: 0.28. In our study we observed a higher correspondence, ranging between 0.33 and 0.42, between the questionnaires filled out by the mothers and the teachers. Another explanation of the low correspondence may be that the manifestation of the same behavioral trait of a child depends of specific environmental factors, i.e. a child being a bit shy at school may show this to a much lesser extent in the family situation.
Several authors have debated the predictive validity for long-term behavioral outcome of the child of the parents versus the teacher's reports. In the Dutch situation, Verhulst et al. (22) found the TRF to be more predictive for long-term outcome than the CBCL, which supports the reliability of our findings with respect to DEX effects in the long run.
One limitation of the study is its retrospective nature. However, the HC and DEX groups were matched for gestation and illness severity. Despite the fact that children in the REF and BMETH groups had a higher birth weight and were larger, more mature, and less ill, HC-treated children did not differ from these groups in neurodevelopment. DEX-treated children had a significantly worse neuromotor outcome. Additionally, our study suggests a better behavioral outcome in neonatally treated HC 7–10-y-old girls compared with their DEX-treated counterparts.
To our knowledge, no gender differences have been reported up to now in relation to outcome after neonatal DEX treatment. It has been reported that girls derive greater benefit than boys from antenatal GC treatment (23). The reason why the preterm girls in our study seem to be relatively more affected by treatment with dexamethasone than their male counterparts remains therefore to be elucidated.
Murphy et al. (24) demonstrated that DEX-treated infants showed a substantial loss of gray matter at 40 wk of age. No study is available as yet that describes volume magnetic resonance imaging (MRI) data for HC-treated children at 40 wk of age. Recently, however, Lodygensky et al. (25) described a cohort of HC-treated preterm infants from our NICU who had a volume MRI at 8 y of age. It appeared that prematurely born children treated with HC had similar gray and white matter volume in comparison to untreated prematurely born children (25). In a recent study in children at school age, who had neonatally been treated with HC, our group did not find changes in magnetic resonance spectroscopy–measured metabolism of the hippocampus in comparison to untreated children. Moreover, short-term memory and IQ were not different from a reference group of children of the same age (26). It is known that the hippocampus, which plays a critical role in memory (27), is an important target for glucocorticoids (28) and prolonged use of DEX impairs hippocampal synaptic plasticity and accelerates hippocampal neuronal loss (29,30). The lower affinity for GC receptors and a higher affinity for mineralocorticoid receptors in the brain than DEX (20) may be responsible for these observed differences and suggest that HC is a safe alternative for DEX when glucocorticoid treatment is unavoidable during early neonatal life in preterm infants with severe CLD.
It has already been established that administration of glucocorticoids via the mother to the fetus reduces risk for neonatal death, respiratory distress and periventricular/intraventricular hemorrhage (31). In the present study, we show that no differences could be detected between the antenatal BMETH group on the one hand, and the REF and HC group (except ball skills in the ABC Movement) on the other hand, suggesting that antenatal BMETH therapy alone is no risk factor with regard to behavioral and neuromotor dysfunction at school age. Because we did not observe adverse effects of BMETH, it is not plausible that the effect we observed in the DEX group is partly due to antenatal BMETH. Additionally, HC and DEX did not differ in antenatal BMETH percentage and we nevertheless observed differences between the HC and DEX group.
In summary, the results suggest that girls treated neonatally with DEX have a lower school performance and display more behavioral problems at 7–10 y of age than HC-treated children. In addition, in the present study motor impairment seem to be significantly higher in the DEX-treated group (boys and girls) than in the REF group. HC-treated children did not, however, differ from untreated children except for ball skills, despite the fact that children in the HC group were smaller and had a lower bodyweight at birth compared with the REF group. We therefore conclude that our present results suggest that HC is a safe alternative for neonatal DEX treatment, but this should be confirmed in a randomized controlled study set-up.
Abbreviations
- ABC Movement:
-
Movement Assessment Battery for Children
- BMETH:
-
betamethasone
- CBCL:
-
Child Behavioral Check List
- CLD:
-
chronic lung disease
- DEX:
-
dexamethasone
- GC:
-
glucocorticoid
- HC:
-
hydrocortisone
- REF:
-
reference
- TRF:
-
Teacher Report Form
References
Shinwell ES, Karplus M, Reich D, Weintraub Z, Blazer S, Bader D, Yurman S, Dolfin T, Kogan A, Dollberg S, Arbel E, Goldberg M, Gur I, Naor N, Sirota L, Mogilner S, Zaritsky A, Barak M, Gottfried E 2000 Early postnatal dexamethasone treatment and increased incidence of cerebral palsy. Arch Dis Child Fetal Neonatal Ed 83: F177–F181
Barrington KJ 2001 The adverse neuro-developmental effects of postnatal steroids in the preterm infant: a systematic review of RCTs. BMC Pediatr 1: 1
O'Shea TM, Kothadia JM, Klinepeter KL, Goldstein DJ, Jackson BG, Weaver RG 3rd, Dillard RG 1999 Randomized placebo-controlled trial of a 42-day tapering course of dexamethasone to reduce the duration of ventilator dependency in very low birth weight infants: outcome of study participants at 1-year adjusted age. Pediatrics 104: 15–21
Yeh TF, Lin YJ, Lin HC, Huang CC, Hsieh WS, Lin CH, Tsai CH 2004 Outcomes at school age after postnatal dexamethasone therapy for lung disease of prematurity. N Engl J Med 350: 1304–1313
Committee on Fetus and Newborn 2002 Postnatal corticosteroids to treat or prevent chronic lung disease in preterm infants. Pediatrics 109: 330–338
Shinwell ES, Karplus M, Bader D, Dollberg S, Gur I, Weintraub Z, Arnon S, Gottfreid E, Zaritsky A, Makhoul IR, Reich D, Sirota L, Berger I, Kogan A, Yurman S, Goldberg M, Kohelet D 2003 Neonatologists are using much less dexamethasone. Arch Dis Child Fetal Neonatal Ed 88: F432–F433
Kaempf JW, Campbell B, Sklar RS, Arduza C, Gallegos R, Zabari M, Brown A, McDonald JV 2003 Implementing potentially better practices to improve neonatal outcomes after reducing postnatal dexamethasone use in infants born between 501 and 1250 grams. Pediatrics 111: e534–e541
Halliday HL, Ehrenkranz RA, Doyle LW 2003 Moderately early (7–14 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Database Syst Rev CD001144.
Doyle LW, Halliday HL, Ehrenkranz RA, Davis PG, Sinclair JC 2005 Impact of postnatal systemic corticosteroids on mortality and cerebral palsy in preterm infants: effect modification by risk for chronic lung disease. Pediatrics 115: 655–661
Watterberg KL, Demers LM, Scott SM, Murphy S 1996 Chorioamnionitis and early lung inflammation in infants in whom bronchopulmonary dysplasia develops. Pediatrics 97: 210–215
Watterberg KL, Gerdes JS, Gifford KL, Lin HM 1999 Prophylaxis against early adrenal insufficiency to prevent chronic lung disease in premature infants. Pediatrics 104: 1258–1263
Thebaud B, Lacaze-Masmonteil T, Watterberg K 2001 Postnatal glucocorticoids in very preterm infants: “the good, the bad, and the ugly”?. Pediatrics 107: 413–415
van der Heide-Jalving M, Kamphuis PJ, van der Laan MJ, Bakker JM, Wiegant VM, Heijnen CJ, Veen S, van Bel F 2003 Short- and long-term effects of neonatal glucocorticoid therapy: is hydrocortisone an alternative to dexamethasone?. Acta Paediatr 92: 827–835
Papile LA, Burstein J, Burstein R, Koffler H 1978 Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr 92: 529–534
Giedion A, Haefliger H, Dangel P 1973 Acute pulmonary X-ray changes in hyaline membrane disease treated with artificial ventilation and positive end-expiratory pressure (PEP). Pediatr Radiol 1: 145–152
Achenbach TM 1992 Manual for the Child Behavioral Checklist/4-18 and 1991 Profile. University Associates in Psychiatry, Burlington, VT
Van Waelvelde H, De Weerdt W, De Cock P, Smits-Engelsman BC 2004 Aspects of the validity of the Movement Assessment Battery for Children. Hum Mov Sci 23: 49–60
Bakker JM, van Bel F, Heijnen CJ 2001 Neonatal glucocorticoids and the developing brain: short-term treatment with life-long consequences?. Trends Neurosci 24: 649–653
Stark AR, Carlo WA, Tyson JE, Papile LA, Wright LL, Shankaran S, Donovan EF, Oh W, Bauer CR, Saha S, Poole WK, Stoll BJ 2001 Adverse effects of early dexamethasone in extremely-low-birth-weight infants. National Institute of Child Health and Human Development Neonatal Research Network. N Engl J Med 344: 95–101
Haynes RC 1990 Adrenocorticotroph hormone: adrenocortical steroids and their synthetic analogs: inhibitors of the synthesis and actions of adrenocortical hormones. In: Goodman LS, Gilman A, Rall TW (eds) The Pharmacological Basics of Therapeutics. Pergamon Press, New York, pp 1431–1459
Achenbach TM, McConaughy SH, Howell CT 1987 Child/adolescent behavioral and emotional problems: implications of cross-informant correlations for situational specificity. Psychol Bull 101: 213–232
Verhulst FC, Koot HM, van der Ende J 1994 Differential predictive value of parents' and teachers' reports of children's behaviors: a longitudinal study. J Abnorm Child Psychol 22: 531–546
Weitzel HK, Lorenz U, Kipper B 1987 Clinical aspects of antenatal glucocorticoid treatment for prevention of neonatal respiratory distress syndrome. J Perinat Med 15: 441–446
Murphy BP, Inder TE, Huppi PS, Warfield S, Zientara GP, Kikinis R, Jolesz FA, Volpe JJ 2001 Impaired cerebral cortical gray matter growth after treatment with dexamethasone for neonatal chronic lung disease. Pediatrics 107: 217–221
Lodygensky GA, Rademaker K, Zimine S, Gex-Fabry M, Lieftink AF, Lazeyras F, Groenendaal F, de Vries LS, Huppi PS 2005 Structural and functional brain development after hydrocortisone treatment for neonatal chronic lung disease. Pediatrics 116: 1–7
Rademaker KJ, Rijpert M, Uiterwaal CS, Lieftink AF, van Bel F, Grobbee DE, de Vries LS, Groenendaal F 2006 Neonatal hydrocortisone treatment related to 1H-MRS of the hippocampus and short-term memory at school age in preterm born children. Pediatr Res 59: 309–313
Isaacs EB, Lucas A, Chong WK, Wood SJ, Johnson CL, Marshall C, Vargha-Khadem F, Gadian DG 2000 Hippocampal volume and everyday memory in children of very low birth weight. Pediatr Res 47: 713–720
De Kloet ER, Vreugdenhil E, Oitzl MS, Joels M 1998 Brain corticosteroid receptor balance in health and disease. Endocr Rev 19: 269–301
Kamphuis PJ, Gardoni F, Kamal A, Croiset G, Bakker JM, Cattabeni F, Gispen WH, van Bel F, Di Luca M, Wiegant VM 2003 Long-lasting effects of neonatal dexamethasone treatment on spatial learning and hippocampal synaptic plasticity: involvement of the NMDA receptor complex. FASEB J 17: 911–913
Sapolsky RM, Uno H, Rebert CS, Finch CE 1990 Hippocampal damage associated with prolonged glucocorticoid exposure in primates. J Neurosci 10: 2897–2902
National Institutes of Health 1994 Report on the Consensus Development Conference on the Effect of Corticosteroids for Fetal Maturation on Perinatal Outcome. NIH publication no. 95–3784.
Acknowledgements
The authors thank Mrs. Marijke Tersteeg-Kamperman for her invaluable technical assistance and Maike Eussen and Jolanda Hoogeboom for their help with the analysis of the data.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by a grant of the Catherijne Stichting, UMC Utrecht, The Netherlands.
Rights and permissions
About this article
Cite this article
Karemaker, R., Heijnen, C., Veen, S. et al. Differences in Behavioral Outcome and Motor Development at School Age After Neonatal Treatment for Chronic Lung Disease with Dexamethasone versus Hydrocortisone. Pediatr Res 60, 745–750 (2006). https://doi.org/10.1203/01.pdr.0000246200.76860.de
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.pdr.0000246200.76860.de
This article is cited by
-
Duration of mechanical ventilation is more critical for brain growth than postnatal hydrocortisone in extremely preterm infants
European Journal of Pediatrics (2021)
-
Hydrocortisone and bronchopulmonary dysplasia: variables associated with response in premature infants
Journal of Perinatology (2020)
-
Let’s call the whole thing off: evaluating gender and sex differences in executive function
Neuropsychopharmacology (2019)
-
Safety, Efficacy and Response to a Hydrocortisone Rescue Therapy Protocol in Children with Refractory Hypotension After Cardiopulmonal Bypass
Pediatric Cardiology (2015)
-
Hydrocortisone vs. dexamethasone treatment for bronchopulmonary dysplasia and their effects on general movements in preterm infants
Pediatric Research (2012)