Abstract
3,3′-diiodothyronine sulfate (T2S) derived from T3 of fetal origin is transferred to the maternal circulation and contributes significantly to the maternal urinary pool. The present study quantitatively assesses the fetal to maternal transfer of T4 metabolites compared with those of T3. Labeled T4 or T3 was infused intravenously to four singleton fetuses in utero in each group at gestational age 138 ± 3 d. Maternal and fetal serum and maternal urine samples were collected hourly for 4 h and at 24 h (serum) or in pooled 4–24 h samples (urine). Radioactive metabolites were identified by HPLC and by specific antibody in serum and urine extracts and expressed as percentage infusion dose per liter. The results demonstrate a rapid clearance of labeled T3 from fetal serum (disappearance T1/2 of 0.7 h versus 2.4 h for T4 in the first 4 h). The metabolites found in fetal serum after labeled T3 infusion were T2S > T3 > T3S; in maternal urine, T2S > unconjugated iodothyronines (UI) > T3S > unknown metabolite (UM). After labeled T4 infusion, the metabolites in fetal serum were rT3 > T3 > T2S > T4S in the first 4 h, and rT3 = T3 = T4S = T2S > T3S at 24 h; in maternal urine we found T2S > UM > UI > T4S > T3S in the first 4 h and UM > T2S > UI in 4–24 h pooled sample. In conclusion, the conversion of T3 to T2S followed by fetal to maternal transfer of T2S and other iodothyronines appears to contribute importantly to maintaining low fetal T3 levels in late gestation.
Similar content being viewed by others
Main
Kinetic studies in fetal sheep in late gestation (>135 d of gestational age; term, 150 d) showed that mean fetal T4 CR and PR are significantly higher than the corresponding values in adult sheep (1). The ratio of mean PR of rT3 to T4 is similar in fetal and adult sheep, whereas the PR ratio of T3 to T4 in fetal sheep is much lower than that in adult sheep. These data in the ovine fetus indicate that the prevailing low serum T3 concentration is due both to increased CR and decreased PR, whereas the elevated serum rT3 levels are due to decreased CR and increased PR. We and others showed that sulfated iodothyronines, including T4S, T3S, rT3S, and 3,3′-T2S are major T4 metabolites in ovine fetuses (2,3). The PR of T4S, T3S, rT3S, and rT3 significantly exceed the PR of T3. Thus, peripheral thyroid hormone metabolism in the ovine fetus, in contrast to the adult, is shunted to inactivation rather than production of active hormone.
In a recent study, we showed that a significant amount of 3,3′-diiodothyronine (T2), the inner-ring deiodinated metabolite of fetal T3, is found in maternal urine as sulfated T2 when 125I-T3 is infused in venously catheterized fetuses (4,5). In contrast, when a supraphysiological dose of T3, about 200-fold the fetal T3 PR, was infused into fetuses, both T2S and T3S were found in maternal urine (6). To exclude the possibility that the observed fetal-to-maternal transfer of metabolites could be a pharmacological dose effect, the present study was conducted to quantify the radioactivities and identify the metabolites in fetal serum and maternal serum and urine following fetal infusion of 125I-T4 contrasted with results after infusion of 125I-T3.
MATERIALS AND METHODS
Animal preparation.
Western mixed-breed, time-dated pregnant ewes with singleton pregnancies were obtained from the Nebeker Ranch (Lancaster, CA) and acclimated to laboratory conditions and food. Animals were studied in two groups, four in each group.
The ewes (131 ± 2 d) were sedated (1.2 mg atropine and 700 mg ketamine i.m.), and a continuous infusion of ketamine (100 mg/h) begun via a jugular venous catheter. After local anesthesia of the abdominal wall (2% lidocaine), a midline incision was followed by palpation of the uterus and fetal parts and identification of the fetal abdomen. A hysterotomy was performed over the fetal lower abdomen and fetal membranes were marsupialized to the skin of the fetal abdomen, avoiding loss of amniotic fluid. The groin area of the singleton fetus was infiltrated with 1% lidocaine, followed by the incision and insertion of catheters in both the femoral vein and artery. The incisions were closed. In each group, the ewes were treated for 3 d postoperatively with oxacillin (2 g) and gentamicin (80 mg) daily given intramuscularly in divided doses. The fetal arterial blood gas and pH were monitored at the beginning and at the end of the infusion study to ascertain normalcy of arterial Po2 and pH values.
Seven to 10 d later, outer-ring labeled 125I-T3 (250 μCi, sp. act. 1300 μCi/μg) or 125I-T4 (250 μCi, sp. act. 5700 μCi/μg) diluted in saline was given in a single bolus via the fetal femoral venous catheter. Maternal and fetal serum samples were collected hourly for 4 h and at 24 h. Maternal urinary samples were collected hourly for the first 4 h and then were pooled from 4 to 24 h. All experiments were approved by the Harbor-UCLA Medical Center Animal Use Committee.
In a separate experiment, involving three pregnant sheep with singleton fetuses, the fetuses and ewes were similarly treated. 125I-T4 was infused into the maternal femoral vein; serum and urine samples were similarly collected from both mother and fetus.
Identification of labeled metabolites in fetal serum and maternal sheep urine and serum.
After fetuses were infused with 125I-T3 or 125I-T4, radioactive metabolites were identified in fetal serum in hourly samples (in one and four lambs after 125I-T3 and 125I-T4 infusion, respectively) and maternal urine extracts (hourly samples from all four sheep of each group). Urine and serum samples were extracted with two volumes of 95% ethanol and subsequently lyophilized. The dried extracts were dissolved in 1 mL of H2O and purified using an LH-20 column as previously described (6). After application to an HPLC μ-Bondapak C18 column (Waters, Milford, MA), the extracts were eluted isocratically with a mixture of acetonitrile and 0.02M ammonium acetate, pH 4.0 (22:78 vol/vol) at a flow rate of 2 mL/min. Aliquots of eluent in 1-mL fractions were collected and 100 μL of these aliquots with significant radioactivities (found only in maternal urine samples following 125I-T3 infusion) were subjected to immunoprecipitation with specific antibodies to T2S, as a major peak. Minor peaks were identified by comparing their retention times to those of known synthetic iodothyronines eluted on HPLC under the same conditions. Hourly urine samples (n = 7) of the identified T2S peaks from two 125I-T3 infusion studies in duplicate were subjected to polyclonal rabbit T2S antibody precipitation; T2S-specific activities were varied from 93.6% to 99.9% (mean 97.6%). Radioactivities in urine or serum extracts were expressed as percentage of injected total dose. Duplicate 0.1% aliquots of the total infused dose were used in each infusion study as counting standards.
T2S RIA.
T2S levels in serum and urine were measured by specific and sensitive RIA methods as described previously (5). Serum and urine samples were extracted with two volumes of 95% ethanol (final ethanol concentration 63%). T2S RIA has a lower limit of detection of 2 ng/dL (33 pmol/L). Among various thyroid hormone analogs studied and known to exist in sheep serum or urine, only T3S, rT3S, and T4S cross-react significantly (3.2, 1.4, and 0.02%, respectively) in the T2S RIA; T4, T3, rT3, and T2 cross-reacted <0.0001%. The T2S concentrations in serum and urine were not corrected for the cross-reactivity of T3S.
Source of materials.
3,3′-T2, T3, and T4 were purchased from Henning-Berlin Co. (Berlin, Germany). 125I-3,3′-T2 was prepared by radioiodination using the method described previously (7). T3S and T2S were synthesized as described by Mol and Visser et al. (8,9). Chlorosulfonic acid, 99%, was purchased from Aldrich Chemical Co. (Milwaukee, WI). Outer-ring labeled 125I-T4 and 125I-T3 were purchased from PerkinElmer NEN (Boston, MA).
RESULTS
Characterization of fetal serum metabolites after fetal infusion of labeled T3 or T4.
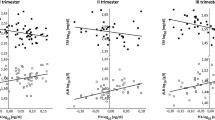
Figure 1 shows radioactivities expressed as percentage of infused dose of radioactive T3 or T4 per liter of serum (% dose/L) in fetuses following the bolus infusion of 125I-T3 or 125I-T4, respectively. There was a rapid decrease in serum 125I-T3, which dropped about 75% in the first hour and 96% by the end of 4 h, then transited to a slow phase from 4 to 24 hour. Similarly, serum 125I-T4 showed a rapid clearance phase during the first 2 h followed by a slow phase. Fetal serum samples analyzed by HPLC at each time period from one fetal sheep showed that T3 decreased rapidly after 125I-T3 infusion; levels dropped to 4.3% dose/L at the end of h 4 from 94.2% dose/L at the end of h 1, with a disappearance T1/2 of approximately 0.7 h. T2S, the major metabolite, on the other hand, increased to 15.4% dose/L from 7.2% dose/L over the same period of time (Table 1). By contrast, there was a slower decrease in T4 following 125I-T4 infusion, from 215% dose/L in the first hour to 125% dose/L at the end of 4 h. RT3 and T3 were the major metabolites after 125I-T4 infusion; respective levels increased from 1.8 and 2.2% dose/L at 1 h to 2.6% and 2.9% dose/L at the end of 24 h. T2S and T4S, the less abundant metabolites, rose from 0.3 and 0.5% dose/L to 1.9 and 2.3% dose/L at 24 h. Negligible amount of rT3S were observed after 125I-T4 infusion.
Metabolites found in maternal serum and urine after fetuses received 125I-T3 or -T4 intravenously.
A total of 15.9% radioactivity was recovered in maternal urine in the first 4 h following fetal infusion of 125I-T3 whereas only 1.0% was recovered following 125I-T4 infusion (Table 2). In contrast, little radioactivity was found in maternal serum after fetal infusion of 125I-T3, an average of 2.2% of the infused dose/L during the first 4 h and 1.0% dose/L at 24 h (Table 3). Even less radioactivity was found in maternal sera after fetal infusion of 125I-T4, 0.22% dose/L at the first hour increasing to 1.4% dose/L at the end of 24 h (Table 3). Because of the low levels of radioactivity, the metabolites were not characterized by HPLC following 125I-T4 infusion. In one maternal serum sample characterized by HPLC 2 h after 125I-T3 infusion, the major metabolites were free iodide and T2S (44.6 and 43.7% of radioactivity distribution, respectively). Minor peaks included T2 and T3 (3.9 and 4.1%, respectively).
The major metabolites found in maternal urine were similar after fetal infusion of either 125I-T3 or 125I-T4, but significantly higher amounts were recovered after T3 infusion than after T4 infusion. Following 125I-T3 infusion, 46.4% of radioactivity was found in the T2S peak in the 1-h maternal urine; the identity of T2S was confirmed by precipitation with a T2S-specific antibody. The percentage of T2S gradually decreased to 22.8% in h 4 and to 6.1% in the 4–24 h pooled urine sample. The iodide fraction increased from 42.4% in the h 1 urine sample to 84.9% in the 4–24 h pooled urine. Expressed as percentage dose, 43.7% of the 125I-T3 radioactivity was recovered in maternal urine in 24 h and 6.4% dose was recovered as T2S. After fetal infusion of 125I-T4, 6.1% of the radioactivity in maternal urine was identified as T2S, whereas 89.4% was iodide at 1 h, and at 4 h, 5.6% of urinary radioactivity is still present in the T2S peak. A peak of an unknown compound appeared after infusion of labeled T3 or T4, amounting to about 8% in the 4–24 h samples in each case (Table 2).
Specific activity of T2S in fetal sera and maternal urine after fetal infusion of 125I-T3 or 125I-T4.
T2S levels were measured in selected fetal serum and maternal urine samples and their specific activities were calculated and expressed as percentage dose per microgram T2S (Table 4). Significantly higher specific activities were found in fetal serum compared with maternal urine after either labeled T3 or T4 infusion in the fetuses. After T3 infusion, however, T2S specific activity in both serum and urine reached a peak early, around h 2, whereas the specific T2S activity continued to increase up to 24 h after T4 infusion, even though activity was much lower than that after T3 infusion. These data suggest that T2S is formed mainly in the fetal compartment and then transferred to the maternal side and finally excreted into maternal urine (4,6). The rate of T2S formed from T3 is significantly higher than that from T4 (Table 4).
Distribution of radioactivity in maternal and fetal sera after the intravenous infusion of 125I-T4 in maternal ewes.
As shown in Table 5, after labeled T4 infusion to maternal ewes (n = 3), the ratios of fetal to maternal serum radioactivities (F/M) were 0.006–0.014 in the first 4 h, increasing to 0.105 at 24 h. The radioactivities were not further characterized by HPLC.
DISCUSSION
The present study demonstrates a rapid clearance of labeled T3 from fetal serum following its infusion; the T1/2 is 0.7 h (Fig. 1). The initial rapid decline in T3 radioactivity may also involve distribution. However, the fact that large amounts of iodide and T2S accrue after 1 h suggests that metabolism plays an important role. Fetal T3 undergoes rapid inner-ring monodeiodination to 3,3′-T2, which is an excellent substrate for all known mammalian iodothyronine sulfotransferases (10–16). The rapid sulfoconjugation of the hydroxyl group in the outer-ring of 3,3′-T2 forms a hydrophilic sulfated T2 (T2S) with enhanced permeability through placental membranes, facilitating transfer to maternal compartments. The T2S of fetal origin appears to be rapidly cleared from the maternal circulation via excretion in urine, as shown in Table 2.
Fetal T4, on the other hand, disappears from the fetal circulation at a slower rate; a fast phase (T1/2 2.4 h) in the first 3 h is followed by a slow phase (T1/2 17.5 h). The major metabolites in fetal circulation after infusion of 125I-T4 were rT3 and T3 as well as their sulfates, T4S, rT3S, and 3,3′-T2S. Negligible amounts of T3S, 0.7–1.2%, were detected (Table 1). Similarly to fetal T3 infusion, the most abundant metabolite found in maternal urine following radioactive T4 infusion is T2S (Table 2). The T4 infusion study confirms previous data in ovine fetuses (2,4,6) indicating that the production of active thyroid hormone (T3) is less than production of inactive products (1.8 versus 3.1% dose/L, respectively in h 1 and 1.9 versus 8.9% dose/L, respectively in h 4, Table 1). It is also interesting that free iodide comprises 14.5–16.8% dose/L generated in the first 3 h and this far exceeds the identified metabolites (4.9–6.5% dose/L in total). This suggests that the lower serum levels of radioactive metabolites are due to rapid distribution and/or production of deiodinated metabolites that are not identified by HPLC. The former is a more likely possibility inasmuch as, by h 4, the percentage dose of metabolites becomes equal to that of free iodine (10.6 versus.= 10.8% dose/L, Table 1), indicating that little, if any, deiodinated metabolites were unaccounted for by HPLC.
It appears that a significant amount of T3 formed in the fetal circulation is converted to T2S and transferred to the maternal compartment for deiodination/excretion. This process would contribute to the low circulating T3 levels in the fetus. Because T2S appears to be quantitatively derived from circulating T3 in the fetus, a significant increase or decrease in T2S in the maternal circulation would suggest hyper- or hypothyroidism in the fetus. We have shown that the amount of T2S excretion in maternal urine reflects fetal thyroid function in sheep (5). Further, recent studies in rats have shown that 3,3′-T2 stimulates mitochondrial respiration in various tissues (17). It is possible that a tight regulation of T2 concentration by sulfation and fetal-to-maternal transfer would have physiologic value. Enhancing fetal-to-maternal transfer may protect the fetus from excessive mitochondrial thermogenesis stimulated by high fetal concentrations of T2. Another T2, i.e. 3,5-T2, was also shown to stimulate mitochondrial thermogenesis (17). 3,5-T2 was not evaluated in the present study but it is likely that the active inner-ring (type 3) deiodinase in fetal mammals rapidly deiodinates 3,5-T2 to T1 (18).
The present study also demonstrated fetal-to-maternal transfer of sulfated iodothyronine metabolites, particularly T2S, but to a lesser degree T3S, rT3S, and T4S. We also demonstrated unconjugated iodothyronines as well as an uncharacterized derivative in maternal urine (Table 2). The site of sulfoconjugation of iodothyronines is likely fetal tissues since there is a much higher specific activity of the T2S in fetal sera relative to maternal urine (Table 4). The lower specific activities of T2S in maternal urine than in fetal serum imply that T2S is formed in pools that do not equilibrate with fetal serum T2S. Whether these pools are in the fetus (possibly derived from the unlabeled iodothyronine in placental tissues) or are of maternal origin is not clear from the present data.
Fetal-to-maternal transfer would involve the placental circulation which comprises 40–50% of fetal cardiac output (19). The placental transfer of T2S and other T3 metabolites to the maternal circulation appears to be an active process helping maintain serum T3 in fetuses at very low levels. This is consistent with the previous findings of Sack and co-workers (20), who showed that umbilical cord cutting triggers hypertriiodothyroninemia in the newborn lamb, and that the postnatal T3 surge can be delayed until well after the TSH peak by delaying umbilical cord cutting. Santini et al. (21) also have shown that the placenta plays an important role in maintaining the low serum T3 in fetuses late in gestation. The present study and the aforementioned studies of Sack et al. and Santini et al. point out the importance of the intact umbilico-placental unit and the continuing fetal-maternal exchange for maintaining the low fetal T3 levels assuring normal growth and development.
Abbreviations
- CR:
-
clearance rate
- PR:
-
production rate
- T2:
-
3,3′-diiodothyronine
- T2S:
-
3,3′-diiodothyronine sulfate
- T3S:
-
T3 sulfate
- T4S:
-
T4 sulfate
References
Wu SY, Fisher DA, Polk DH, Chopra IJ 1991 Maturation of thyroid hormone metabolism. In: Wu SY (ed) Thyroid Hormone Metabolism: Regulation and Clinical Implications. Blackwell Scientific Publications, Boston, 293–320
Polk DH, Fisher DA, Wu SY 1994 Alternate pathways of thyroid hormone metabolism in developing mammals. In: Wu SY, Visser TJ (eds) Thyroid Hormone Metabolism: Molecular Biology and Alternate Pathways. CRC Press: Boca Raton, pp 223–243
Polk DH, Reviczky A, Wu SY, Huang WS, Fisher DA 1994 Metabolism of sulfoconjugated thyroid hormone derivatives in developing sheep. Am J Physiol 266: E892–E896
Wu SY, Polk DH, Huang WS, Fisher DA 1999 Fetal-to-maternal transfer of 3,3′,5-triiodothyronine sulfate and its metabolite in sheep. Am J Physiol 277: E915–E919
Wu SY, Huang WS, Fisher DA, Florsheim WH, Kashiwai K, Polk DH 2001 3,3′-Diiodothyronine sulfate excretion in maternal urine reflects fetal thyroid function in sheep. Pediatr Res 50: 358–364
Wu SY, Polk D, Fisher DA, Huang WS, Reviczky AL, Chen WL 1995 Identification of 3,3′-T2S as a fetal thyroid hormone derivative in maternal urine in sheep. Am J Physiol 268: E33–E39
Nakamura Y, Chopra IJ, Solomon DH 1977 Preparation of high-specific- activity radioactive iodothyronines and their analogues. J Nucl Med 18: 1112–1115
Eelkman Rooda SJ, Kaptein E, van Loon MA, Visser TJ 1988 Development of a radioimmunoassay for triiodothyronine sulfate. J Immunoassay 9: 125–134
Mol JA, Visser TJ 1985 Synthesis and some properties of sulfate esters and sulfamates of iodothyronines. Endocrinology 117: 1–7
Visser TJ 1994 Sulfation and glucuronidation pathways of thyroid hormone metabolism. In: Wu SY, Visser TJ (eds) Thyroid Hormone Metabolism: Molecular Biology and Alternate Pathways. CRC Press, Boca Raton, pp 85–117
Kester MH, Kaptein E, Roest TJ, van Dijk CH, Tibboel D, Meinl W, Glatt H, Coughtrie MW, Visser TJ 2003 Characterization of rat iodothyronine sulfotransferases. Am J Physiol Endocrinol Metab 285: E592–E598
Fujita K, Nagata K, Ozawa S, Sasano H, Yamazoe Y 1997 Molecular cloning and characterization of rat STIBI and human ST1B2 cDNAs, encoding thyroid hormone sulfotransferases. J Biochem 122: 1052–1061
Wu SY, Huang WS, Fisher DA, Florsheim WH, St Germain DL, Galton VA 2000 Iodothyronine sulfotransferase activity in rat uterus during gestation. Pediatr Res 48: 847–851
Li X, Clemens DL, Anderson RJ 2000 Sulfation of iodothyronines by human sulfotransferase 1C1 (SULT1C1)*. Biochem Pharmacol 60: 1713–1716
Stanley EL, Hume R, Visser TJ, Coughtrie MW 2001 Differential expression of sulfotransferase enzymes involved in thyroid hormone metabolism during human placental development. J Clin Endocrinol Metab 86: 5944–5955
Wu SY, Green WL, Huang WS, Hays MT, Chopra IJ 2005 Alternate pathways of thyroid hormone metabolism. Thyroid 15: 943–958
Moreno M, Lanni A, Lombardi A, Goglia F 1997 How the thyroid controls metabolism in the rat: different roles for triiodothyronine and diiodothyronines. J Physiol 505: 529–538
Bates JM, St Germain DL, Galton VA 1999 Expression profiles of the three iodothyronine deiodinases, D1, D2, and D3, in the developing rat. Endocrinology 140: 844–851
Rudolph AM, Heymann MA 1970 Circulatory changes during growth in the fetal lamb. Circ Res 26: 289–296
Sack J, Beaudry M, DeLamater PV, Oh W, Fisher DA 1976 Umbilical cord cutting triggers hypertriiodothyroninemia and nonshivering thermogenesis in the newborn lamb. Pediatr Res 10: 169
Santini F, Chiovato L, Ghirri P, Lapi P, Mammoli C, Montanelli L, Scartabelli G, Ceccarini G, Coccoli L, Chopra IJ, Boldrini A, Pinchera A 1999 Serum iodothyronine in the human fetus and the newborn: evidence for an important role of placenta in fetal thyroid hormone homeostasis. J Clin Endocrinol Metab 84: 493–498
Author information
Authors and Affiliations
Corresponding author
Additional information
This work has been supported by the Department of Veterans' Affairs and the National Science Council (ROC), NSC 82-0412-B-016-085.
Rights and permissions
About this article
Cite this article
Wu, SY., Polk, D., Huang, WS. et al. Fetal-to-Maternal Transfer of Thyroid Hormone Metabolites in Late Gestation in Sheep. Pediatr Res 59, 102–106 (2006). https://doi.org/10.1203/01.pdr.0000191142.56073.f8
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.pdr.0000191142.56073.f8