Abstract
Mitochondrial fatty acid oxidation disorders (FAOD) are recessively inherited errors of metabolism. Newborns with FAOD typically present with hypoketotic hypoglycemia, metabolic acidosis, hepatic failure, and cardiomyopathy. Late presentations include episodic myopathy, neuropathy, retinopathy, and arrhythmias. Sudden unexpected death can occur at any age and can be confused with sudden infant death syndrome. Some FAOD are associated with intrauterine growth restriction, prematurity, and pregnancy complications in the heterozygous mother, such as severe preeclampsia, acute fatty liver of pregnancy (AFLP), or hemolysis, elevated liver enzymes, and low platelets (HELLP) syndrome. Maternal pregnancy complications occur primarily in mothers carrying a fetus with long-chain l-3-hydroxyacyl CoA dehydrogenase deficiency or general trifunctional protein deficiencies. FAOD as a group represent the most common inborn errors of metabolism, and presymptomatic diagnosis of FAOD is the key to reduce morbidity and avoid mortality. The application of tandem mass spectrometry to newborn screening provides an effective means to identify most FAOD patients presymptomatically. At the beginning of 2005, 36 state newborn screening programs have mandated or adopted this technology resulting in a marked increase in the number of asymptomatic neonates with FAOD diagnosed. To ensure the long-term benefits of such screening programs, pediatricians and other health care providers must be educated about these disorders and their treatment.
Similar content being viewed by others
Main
Fatty acids constitute the largest energy reserve in the body and play a crucial role in supplying energy-yielding substrates during periods of fasting and stress through the β-oxidation pathway (1). FAO provides nearly 80% of energy to organs like heart, liver, and skeletal muscles, especially during fasting when tissue glycogen stores become depleted. The β-oxidation pathway also generates ketone bodies, which are used by peripheral tissues and brain (2). This metabolic pathway is critical for the neonate who has limited glycogen reserve and a high metabolic rate leading to rapid metabolic decompensation if there is any perturbation of individual enzymes (3). FAOD are potentially fatal autosomal recessive disorders and are now diagnosed frequently in the perinatal and infantile periods. Mothers heterozygous for a FAOD and pregnant with an affected fetus may develop severe preeclampsia, AFLP, and the HELLP syndrome, and may deliver a premature, intrauterine growth-restricted (IUGR) infant (4).
The first genetic defect in fat oxidation was described in 1973, involving a patient with what is now known as carnitine palmitoyltransferase II (CPT II) deficiency (5,6). Since that time, there has been a steady increase in discovery of newer FAOD and an exponential rise in patients diagnosed with these disorders (6). Advances in this field have recently been facilitated by the availability of MS/MS technology with which a single analysis provides a clue as to the type of FAOD the patient may have. Here we review this seemingly complex subject, and discuss its likely impact on health care of newborn infants and their mothers in the near future.
THE MITOCHONDRIAL β-OXIDATION PATHWAY
Figure 1 represents a schematic of the mitochondrial β-oxidation pathway starting with uptake of fatty acids and carnitine into the cell, transfer of fatty acid from the cytosol into mitochondria, and entry into the β-oxidation spiral. Medium- and short-chain fatty acids are transported directly into the cytosol and mitochondria, but long-chain fatty acids and carnitine are transported by specific plasma membrane transporters like fatty acid transporter (FAT), and fatty acid-binding protein (FABP) (7–9). Carnitine a key factor in facilitating entry of long-chain fatty acids into the mitochondria is transported into the cell through its transporter OCTN2 (10). Activated fatty acyl-CoA are converted to carnitine esters by carnitine palmitoyltransferase I (CPT I), transferred across the mitochondrial membranes by carnitine-acylcarnitine translocase (CACT), and fatty acyl-CoA reconstituted by CPT II (11).
The mitochondrial fatty acid β-oxidation pathway. This schematic shows the various enzymes involved in cellular uptake of fatty acids and carnitine, followed by their transport into the mitochondria and subsequent β-oxidation. Reproduced with permission from Am J Physiol Endocrinol Metab 284:E1098–E1105. Copyright © 2003 the American Physiological Society.
The initial step in the FAO spiral is the acyl-CoA dehydrogenase reaction catalyzed by the homologous flavoprotein-linked (FAD) enzymes MCAD, LCAD, and VLCAD and leads to formation of a 2,3-enoyl-acyl-CoA (12). The second step is the conversion of a 2,3-enoyl-acyl-CoA to a 3-hydroxyacyl-CoA catalyzed by 2,3-enoyl-CoA hydratase. The third step of the spiral is the conversion of 3-hydroxyacyl-CoA to 3-ketoacyl-CoA catalyzed by the two homologous enzymes SCHAD and LCHAD, and, in the final step, one acetyl-CoA molecule is removed from the 3-ketoacyl-CoA by the two homologous enzymes, short-chain 3-keto-acyl-CoA thiolase (SKAT) and long-chain 3-keto-acyl-CoA thiolase (LKAT), respectively. For longer chain fatty acids, the latter three steps of this pathway are catalyzed by the membrane-bound MTP, a hetero-octameric complex in which the α-subunit contains the LCHAD and hydratase activities and the β-subunit contains the long-chain 3-ketoacyl-CoA thiolase activity. The end result of each cycle of β-oxidation is production of a shortened acyl-CoA that reenters the β-oxidation spiral within the mitochondrial matrix and one molecule of acetyl-CoA. Acetyl-CoA may be used for steroidogenesis, enter the TCA cycle, or become transformed into ketone bodies in the liver by the action of 3-hydroxy-3-methylglutaryl-CoA synthetase (HMGCS2) and 3-hydroxy-3-methylglutaryl-CoA lyase (HMGCL) (13). The FAD-linked dehydrogenases (MCAD, LCAD, and VLCAD) generate electrons which are transferred to ubiquinone via the electron transfer flavoproteins (ETF) and ETF dehydrogenase (ETFDH). Electrons from NADH-linked dehydrogenation (SCHAD and LCHAD) are shifted to complex 1 in the respiratory chain eventually leading to production of energy as ATP.
Unsaturated fatty acids with cis double bonds are also degraded by mitochondrial β-oxidation and require two auxiliary enzymes such as enoyl-CoA isomerase and dienoyl-CoA reductase (13). Our current knowledge of cellular uptake mechanisms, intracellular trafficking, degradation, and utilization of long-chain fatty acids is incomplete. The fact that there are many patients with clinical presentations indicative of a FAOD in whom FAO enzymatic activity analyses and molecular studies of all known enzymes fail to reveal any abnormalities, suggests that additional enzymes remain undiscovered. The opposite situation of known or newly detected fatty acyl-CoA dehydrogenases with yet-to-be-defined clinical deficiency states further underscores the current lack of understanding of this complex metabolic pathway (14,15).
THE MITOCHONDRIAL FATTY ACID β-OXIDATION DISORDERS
More than 20 defects in fatty acid transport and mitochondrial β-oxidation are known and all are inherited as autosomal recessive disorders (1). The genes encoding most of the known enzymes are known and mutations have been discovered in affected patients. The clinical presentations of FAOD vary from a neonatal onset with severe metabolic acidosis, hypoglycemia associated with absent or inadequate ketone production, hyperammonemia, cardiomyopathy, liver failure, and sudden death, to a late onset with episodic myopathy, neuropathy, and retinopathy. FAOD become apparent during periods of increased energy demands, such as prolonged fasting, febrile illness, or any other stressful situation during which the inability to use fatty acids causes metabolic decompensation. FAOD have been implicated as the cause of death in 5–8% cases of sudden unexpected death in infancy based on metabolic studies of surviving siblings, “near-miss” SIDS cases, and postmortem studies (16).
The genetic defects and clinical and biochemical features of major FAOD are summarized in Table 1. Incidences of individual FAOD may vary from 1:8000 to 1:100,000; but, as a group, FAOD represent the most common metabolic disorder with severe consequences for affected individuals. More detailed descriptions of individual FAOD are available in recently published reviews and book chapters (1–3,17,18).
PREECLAMPSIA, AFLP, AND HELLP SYNDROME
Preeclampsia is characterized by pregnancy-induced hypertension, edema, and proteinuria and occurs in up to 5–8% of all pregnancies (19). In a small percentage of cases, preeclampsia progresses to severe eclampsia with marked hypertension, encephalopathy, and seizures. Severe preeclampsia in some cases is associated with HELLP syndrome, with an incidence of 1–6 cases per 1000 deliveries (20,21). AFLP is another severe condition of pregnancy with a prevalence ranging from 1 in 10,000 to 1 in 15,000 pregnancies and carries a high mortality (21). Preeclampsia, HELLP syndrome, and AFLP have been suggested to represent a spectrum of the same pathologic process (21–24).
HELLP syndrome is characterized by microangiopathic hemolytic anemia, elevated liver enzymes, and thrombocytopenia. Typically, patients with HELLP syndrome present in their third trimester (28–34 wk gestation) with nausea, vomiting, headache, hypertension, proteinuria, and right upper quadrant pain, and disseminated intravascular coagulation in advanced cases (22). Women with HELLP syndrome have a higher incidence of fetal distress and cesarean section and often give birth to a preterm, IUGR infant with lower Apgar scores in about a third of cases (25). AFLP is the rarest of the three maternal pregnancy complications. The potentially fatal clinical presentation of AFLP is similar to HELLP syndrome but jaundice is frequently seen in these patients. Fatty liver has been demonstrated in some cases where a biopsy was performed. In one recent analysis of multiple studies, AFLP was associated with maternal hypoglycemia in nearly 50% of patients, disseminated intravascular coagulopathy (DIC) in 88%, encephalopathy in 38%, and death in 6% (21). AFLP led to a high perinatal mortality (15%) and 70% of infants were born preterm (26,27). AFLP and HELLP have a similar clinical presentation with elevated liver enzymes and ultrasound findings of increased echogenicity, and only histologic investigation of a liver biopsy allows an unequivocal diagnosis.
ASSOCIATION OF FETAL FAOD AND MATERNAL PREECLAMPSIA, AFLP AND HELLP SYNDROME
During pregnancy, increased activity of hormone-sensitive lipase in combination with gestational insulin resistance causes an increase in the levels of FFA in maternal blood. The maternal liver responds to these metabolic changes by synthesizing triglycerides, which are secreted as VLDL and LDL that are taken up by placenta. In the last trimester, greater metabolic demands of the fetus shift maternal metabolism toward ketogenesis and the fetus uses maternal ketone bodies for lipogenesis as well as for energy production. Therefore, defects in FAO in the fetoplacental unit become clinically evident at this stage of gestation (28). These associations of placental complications and poor fetal and neonatal outcomes have been described with defects in fatty acid transport across mitochondrial membranes and in enzymes involved in mitochondrial FAO (Fig. 2).
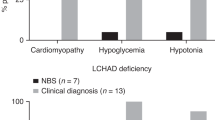
Genetic defects in FAO within the mitochondria have been shown to be associated with maternal, placental and fetal complications. The first report of this association was published by Wilcken et al. (29) in 1993, in which 11 pregnancies in five mothers resulted in six babies with LCHAD deficiency. Each of these pregnancies was complicated by maternal fatty liver, HELLP syndrome, and preterm delivery. Wilcken and colleagues based their diagnosis of LCHAD deficiency on 3-hydroxydicarboxylic aciduria. In 1995, Sims et al. (30) first defined a molecular basis of this association in three families using DNA analysis. In another large case series, Strauss and co-workers (31) found that 62% of mothers carrying an affected fetus with LCHAD deficiency developed AFLP or the HELLP syndrome during their pregnancies. Since that time, similar associations have been described for defects in other enzymes in the FAO pathway. In isolated LCHAD (24,30–34) or general trifunctional protein (TFP) (24,31,32,35) deficiency, maternal liver disease is common, occurring in approximately 20–70% of affected pregnancies. MCAD (36), short-chain acyl CoA dehydrogenase (SCAD) (37,38), and CPT-1 (39) deficiencies have been associated with maternal liver disease in single case reports.
ROLE OF FAO IN THE PLACENTA AND FETUS DURING GESTATION
Although studies in humans with genetic defects in FAO have steadily generated evidence for an essential role of fatty acid oxidation in the fetoplacental unit, recent basic science work has demonstrated that human placenta indeed, expresses six key enzymes of the β-oxidation pathway. Crude human placental extracts showed high activity of these enzymes, comparable to skeletal muscle; and isolated placental trophoblast cells are able to use labeled long-chain fatty acids, palmitate, and myristate in substantial quantities (40–42). As shown in Figure 2, when a heterozygous mother is pregnant with an affected fetus, the placenta and the fetus are unable to optimally oxidize fatty acids, potentially leading to transfer of metabolic intermediates to the maternal circulation. These compounds have been postulated to cause maternal preeclampsia, HELLP syndrome, and AFLP. In a recent study of 33 preeclamptic mothers, maternal plasma had significantly higher long and very-long chain acylcarnitines compared with controls (43). Although the etiology of preeclampsia remains unknown, this indirect evidence suggests that perturbation of mitochondrial FAO may be partially responsible for this condition.
Several other elegant animal studies have produced unequivocal data demonstrating that fatty acid metabolism is critical for placental function and fetal development. Ablation of genes encoding enzymes involved in FAO such LCAD, VLCAD, and TFP is associated with increased in utero fetal demise, reduced fertility, and fetal growth restriction (44–46). Similarly, ablation of the genes coding for the transcription factors peroxisome proliferator-activated receptors β/δ and γ (PPARβ/δ and PPARγ) and the co-activator of PPARγ (PGC-1) that are the master regulators of fatty acid metabolism, results in embryonic lethality. More importantly, inactivation of these transcription factors leads to specific placental phenotypes in which the syncytiotrophoblast, the functional unit of the placenta, fails to develop and sustain pregnancy (47–49). Ablation of the gene encoding fatty acid synthase also leads to fetal demise (50). Thus, fatty acids play a critical role in placental development and function and in fetal well being.
LABORATORY INVESTIGATION OF FAOD
The biochemical features of FAOD commonly seen in clinical situations include hypoglycemia without evidence of appropriate ketone body production, lactic acidosis, and elevated liver enzymes like AST and ALT. Along with clinical features listed earlier, these laboratory abnormalities should prompt immediate work up for a FAOD, including at the least urine organic acids, and plasma or blood acylcarnitine analysis. Additional biochemical investigations, such as urine acyl-glycine and plasma FFA profiling, as well as determination of total fatty acids, and free and total carnitine in plasma should also be considered (1–3). Measurement of free and total carnitine in urine is only recommended in a patient at risk of primary carnitine uptake defect and only before l-carnitine supplementation. Samples for analysis should preferably be procured early during the acute manifestation because successful reversal of catabolism may normalize the biochemical phenotype of several FAOD. If the patient is doing well, samples should be collected before a meal. Fasting tests, which are potentially life threatening, can be avoided in most patients and should only be conducted in controlled settings and with i.v. access. Biochemical investigations during a metabolic crisis are usually suggestive, if not diagnostic, of a particular FAOD, and allow for initiation of appropriate treatment.
Definitive diagnosis of individual FAOD is accomplished by measurement of individual enzyme activities and FAO substrate utilization rates in fibroblasts derived from a small skin biopsy. Molecular genetic analysis of genomic DNA can often define the exact defect and is particularly helpful when an FAOD is caused by an enzyme not expressed in fibroblasts. Once a FAOD has been diagnosed, the above mentioned analyses can aid in determination of treatment efficacy. For example, fatty acid profiling can be used to avoid nutritional deficiencies of essential fatty acids by overt dietary fat restriction (51,52).
The metabolic work-up of patients who suffered a sudden unexpected death (“metabolic autopsy”) should include the investigation for a FAOD because they have been identified as the underlying cause of death in 5–8% of cases (53). This is facilitated by acylcarnitine analysis that can be performed most efficiently on small samples of blood and bile collected postmortem and dried on filter paper (Table 2) (54).
To identify and initiate treatment of patients with an FAOD before the development of symptoms, acylcarnitine analysis by MS/MS can also be performed on newborn screening blood spots. The ongoing introduction of MS/MS into newborn screening laboratories since the early 1990s has markedly increased the number of diagnosed and successfully treated patients with a FAOD (55).
Once a diagnosis has been made, family investigations and genetic counseling should be pursued. Prenatal diagnosis of most FAOD is possible by molecular genetic, enzyme, or metabolite analyses using chorionic villi, amniotic fluid, or amniocyte cultures (56). Although FAOD are associated with high morbidity and mortality, it must be remembered that some FAOD, like MCAD deficiency, which have an excellent prognosis when treatment consisting of avoidance of fasting is initiated at birth, are questionable candidates for invasive prenatal diagnostic procedures or pregnancy termination.
MS/MS
Mass spectrometry was first introduced in clinical medicine in the 1960s (57) to diagnose organic acidemia by gas chromatography-mass spectrometry (GC-MS). In the 1980s, MS/MS was applied to the diagnosis of inborn errors of metabolism by acylcarnitine analysis (58). Due to the development of affordable, computer-driven, and relatively user-friendly instruments, MS/MS as a highly sensitive and versatile analytical technology is becoming an integral part of biochemical genetics, clinical chemistry, and newborn screening laboratories, as attested by several excellent reviews published in recent years (59–62). This analytical technique measures the weight of ions derived from a neutral compound after ionization. Most instruments currently used in clinical laboratories consist of two triple-quadrupole mass spectrometers in series separated by a collision cell. The liquid samples are introduced into the first MS after ionization that occurs in the ion source. The quadrupoles consist of four rods that separate the ions by their mass-to-charge ratio (m/z). When passing through the collision cell, the ions are fragmented by collision with an inert gas (i.e. nitrogen) and the resulting ion fragments' weights are determined by the second MS. Analysis, data acquisition, and generation of a mass spectrum are completed in minutes. Due to the unique fragmentation pattern of molecules, only limited sample clean-up and preparations are typically necessary (61).
MS/MS IN NEWBORN SCREENING FOR FAOD
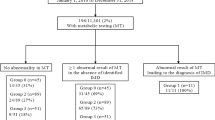
Due to the high sensitivity of MS/MS instruments and the availability of isotopically labeled internal standards, researchers at Duke University Medical Center (Durham, NC) in the early 1990s began to study the possibility to use MS/MS for the analysis of acylcarnitines and amino acids in dried blood spots collected for newborn screening. After a short sample preparation, which consists of the extraction of analytes (acylcarnitines and amino acids) from small (typically 1/8–3/16 in) dried blood spot discs punched from the screening card, the addition of isotopically labeled internal standards, and esterification with butanol-HCl, Chace and colleagues (63) first demonstrated the feasibility of MS/MS-based screening for phenylketonuria. The first FAOD that was demonstrated to be detectable by MS/MS in newborn screening blood spots was MCAD deficiency (64). Newborn screening for MCAD deficiency by MS/MS is now included in 34 states in the United States (http://genes-r-us.uthscsa.edu/) and many other parts of the developed world (65). Twenty-eight of these 34 states also mandate the inclusion of a variable number of additional FAOD, organic acidemias, and amino acidemias into their panels because MS/MS analysis allows the simultaneous detection of at least 30 different inborn errors fatty acid and amino acid metabolism in the same sample (http://genes-r-us.uthscsa.edu/). Table 3 summarizes recent reports about individual programs' experiences with MS/MS. MCAD deficiency is the most frequently detected FAOD by these programs that screen primarily white populations. Surprisingly, LCHAD deficiency appears unexpectedly rare among the detected FAOD. The reason for this is not entirely clear as several publications were able to demonstrate pathologic acyl-carnitine profiles when retrospectively analyzing the original newborn screening samples of patients who were diagnosed either during an acute episode or postmortem (66–68). Part of the problem may be the analytical platform represented by MS/MS, which currently does not provide “plug-and-play” characteristics and is fundamentally different to the traditional single-analyte screening assays, in particular the original Guthrie test, a bacterial inhibition assay. MS/MS not only requires experience with this technology but also with the interpretation of metabolite profiles generated for acylcarnitines and amino acids.
The first pilot studies using MS/MS for newborn screening were conducted in North Carolina, and the first report of North Carolina's state newborn screening program's experience included 237,774 infants screened over a 2-y period. The incidence of MCAD was found to be 1 in 13,600 live births, with an overall incidence of inborn errors of fatty acid and amino acid metabolism detected by MS/MS of 1 in 4,400 (69). The newborn screening program of New South Wales, Australia, reported their findings in 362,000 newborns over a 4-y period. Analysis of data showed that rate of detection of MCAD and other FAOD increased significantly compared with the time before expanded newborn screening (55). MS/MS screening of 382,247 subjects from Bavaria, Germany, compared with 844,575 subjects among whom diagnosis or ascertainment was done after symptomatic presentation of FAO showed a much higher yield of diagnosis when MS/MS technology was used (70).
LOGISTICAL, FINANCIAL, AND ETHICAL CONSIDERATIONS FOR THE INCLUSION OF FAOD IN NEWBORN SCREENING PROGRAMS
Screening of newborn infants for genetic diseases has been in existence for 40 y with the objective of identifying effectively treatable disorders in the presymptomatic stage to avoid long-term morbidity and mortality by early initiation of treatment (71). Selection of the disorders to be screened has been at the discretion of each state. However, with the advent of MS/MS technology and its ability to identify more than 30 different inborn errors of metabolism simultaneously in a small blood spot sample, the discrepancies between states become more pronounced. The US Department of Health and Human Services has therefore established the Secretary's Advisory Committee on Heritable Disorders and Genetic Diseases in Newborns and Children. This committee has recently submitted their recommendations for a universal newborn screening panel listing 30 disorders (http://www.modimes.org/professionals/681_1200.asp).
Newborn screening by MS/MS by individual state screening programs involves the purchase and maintenance of the necessary equipment, training of personnel, and establishment of a system of follow-up by experts for diagnosed or suspected patients. Although this suggests increased costs to states' health-care systems, a recent study showed that the incremental cost of MS/MS screening over and above traditional newborn screening assays used in state laboratories is only about $0.70 per sample (55). Moreover, thorough cost-benefit analysis studies demonstrate definite benefits of early diagnosis by avoidance of long-term care costs (55,72–74) for FAOD patients who suffer from neurologic sequelae of their disease manifestation. Newborn screening clearly prevents death and disability in most patients. A recent study from Boston has reviewed this aspect of screening and found that proactive newborn screening identified significantly more disorders and reduced the rate of mental retardation and parental anxiety among screened population (75).
Expanded MS/MS-based newborn screening, despite the modest extra costs involved and some limitations, has revolutionized our ability to diagnose FAOD disorders early in life. The benefits to society of expanded newborn screening are evident, and this screening should be adopted as a standard of care. The often-voiced concern about a lack of specialists available for follow-up of patients identified by newborn screening seems unwarranted. However, the benefits of newborn screening for the individuals, their families, and society can only be achieved in a newborn screening system characterized by effective communication between the public health department that must provide the framework, the screening laboratories that must provide reliable results, the primary care providers, and the metabolic specialists (76). At the same time, there is an urgent need to impart extensive education to health-care professionals about these disorders hitherto considered rare, their outcomes, and the appropriate follow-up and preventive management. Expanded newborn screening with MS/MS will bring new challenges to our health-care systems, and there is need for open communication between all involved in the screening process to formulate a rational approach to FAOD diagnosis and management.
Abbreviations
- AFLP:
-
acute fatty liver of pregnancy
- FAO:
-
fatty acid oxidation
- FAOD:
-
fatty acid oxidation disorders
- HELLP:
-
hemolysis, elevated liver enzymes, and low platelets syndrome
- HMGCL:
-
3-hydroxy-3-methylglutaryl-CoA lyase
- HMGCS2:
-
3-hydroxy-3-methylglutaryl-CoA synthetase
- LCAD:
-
long-chain acyl CoA dehydrogenase
- LCHAD:
-
long-chain l-3-hydroxyacyl CoA dehydrogenase
- LKAT:
-
long-chain 3-ketoacyl-CoA thiolase
- MCAD:
-
medium-chain acyl CoA dehydrogenase
- MS/MS:
-
tandem mass spectrometry
- MTP:
-
mitochondrial trifunctional protein
- OA:
-
organic acidemias
- SCHAD:
-
short-chain l-3-hydroxyacyl CoA dehydrogenase
- SIDS:
-
sudden infant death syndrome
- VLCAD:
-
very-long-chain acyl CoA dehydrogenase
References
Rinaldo P, Matern D, Bennett MJ 2002 Fatty acid oxidation disorders. Annu Rev Physiol 64: 477–502
Bennett MJ, Rinaldo P, Strauss AW 2000 Inborn errors of mitochondrial fatty acid oxidation. Crit Rev Clin Lab Sci 37: 1–44
Sim KG, Hammond J, Wilcken B 2002 Strategies for the diagnosis of mitochondrial fatty acid beta-oxidation disorders. Clin Chim Acta 323: 37–58
Preece MA, Green A 2002 Pregnancy and inherited metabolic disorders: maternal and fetal complications. Ann Clin Biochem 39: 444–455
DiMauro S, DiMauro PM 1973 Muscle carnitine palmityltransferase deficiency and myoglobinuria. Science 182: 929–931
Bartlett K, Eaton S 2004 Mitochondrial beta-oxidation. Eur J Biochem 271: 462–469
Dutta-Roy AK 2000 Cellular uptake of long-chain fatty acids: role of membrane-associated fatty-acid-binding/transport proteins. Cell Mol Life Sci 57: 1360–1372
Schaffer JE 2002 Fatty acid transport: the roads taken. Am J Physiol Endocrinol Metab 282: E239–E246
Abumrad N, Coburn C, Ibrahimi A 1999 Membrane proteins implicated in long-chain fatty acid uptake by mammalian cells: CD36, FATP and FABPm. Biochim Biophys Acta 1441: 4–13
Wu X, Prasad PD, Leibach FH, Ganapathy V 1998 cDNA sequence, transport function, and genomic organization of human OCTN2, a new member of the organic cation transporter family. Biochem Biophys Res Commun 246: 589–595
Kerner J, Hoppel C 2000 Fatty acid import into mitochondria. Biochim Biophys Acta 1486: 1–17
Wanders RJ, Vreken P, den Boer ME, Wijburg FA, van Gennip AH, IJlst L 1999 Disorders of mitochondrial fatty acyl-CoA beta-oxidation. J Inherit Metab Dis 22: 442–487
Lea W, Abbas AS, Sprecher H, Vockley J, Schulz H 2000 Long-chain acyl-CoA dehydrogenase is a key enzyme in the mitochondrial beta-oxidation of unsaturated fatty acids. Biochim Biophys Acta 1485: 121–128
Yamaguchi S, Indo Y, Coates PM, Hashimoto T, Tanaka K 1993 Identification of very-long-chain acyl-CoA dehydrogenase deficiency in three patients previously diagnosed with long-chain acyl-CoA dehydrogenase deficiency. Pediatr Res 34: 111–113
Ye X, Ji C, Zhou C, Zeng L, Gu S, Ying K, Xie Y, Mao Y 2004 Cloning and characterization of a human cDNA ACAD10 mapped to chromosome 12q24.1. Mol Biol Rep 31: 191–195
Boles RG, Buck EA, Blitzer MG, Platt MS, Cowan TM, Martin SK, Yoon H, Madsen JA, Reyes-Mugica M, Rinaldo P 1998 Retrospective biochemical screening of fatty acid oxidation disorders in postmortem livers of 418 cases of sudden death in the first year of life. J Pediatr 132: 924–933
Roe CR, Ding J 2001 Mitochondrial fatty acid oxidation disorders. In: Scriver CR, Sly WS, Childs B, Beaudet AL, Valle D, Kinzler KW, Bert Vogelstein B (eds) The Metabolic and Molecular Bases of Inherited Disease. McGraw-Hill, New York, pp 2297–2326
Cuthbert CD, Tortorelli S, Ensenauer R, Rinaldo P, Matern D 2004 Inherited abnormalities in mitochondrial fatty acid oxidation. In: Walker WA, Goulet OJ, Kleinman RE, Sanderson IR, Sherman PM, Shneider BL (eds) Pediatric Gastrointestinal Diseases: Pathophysiology, Diagnosis, Management. BC Decker, Hamilton, Ontario, pp 1287–1307
Rahman TM, Wendon J 2002 Severe hepatic dysfunction in pregnancy. QJM 95: 343–357
Barton JR, Sibai BM 2004 Diagnosis and management of hemolysis, elevated liver enzymes, and low platelets syndrome. Clin Perinatol 31: 807–833
Sibai BM 2004 Imitators of severe pre-eclampsia/eclampsia. Clin Perinatol 31: 835–852
Martin JN Jr, Rinehart BK, May WL, Magann EF, Terrone DA, Blake PG 1999 The spectrum of severe preeclampsia: comparative analysis by HELLP (hemolysis, elevated liver enzyme levels, and low platelet count) syndrome classification. Am J Obstet Gynecol 180: 1373–1384
Strauss AW, Bennett MJ, Rinaldo P, Sims HF, O'Brien LK, Zhao Y, Gibson B, Ibdah J 1999 Inherited long-chain 3-hydroxyacyl-CoA dehydrogenase deficiency and a fetal-maternal interaction cause maternal liver disease and other pregnancy complications. Semin Perinatol 23: 100–112
Tyni T, Ekholm E, Pihko H 1998 Pregnancy complications are frequent in long-chain 3-hydroxyacyl-coenzyme A dehydrogenase deficiency. Am J Obstet Gynecol 178: 603–608
Abramovici D, Friedman SA, Mercer BM, Audibert F, Kao L, Sibai BM 1999 Neonatal outcome in severe preeclampsia at 24 to 36 weeks' gestation: does the HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome matter?. Am J Obstet Gynecol 180: 221–225
Castro MA, Fassett MJ, Reynolds TB, Shaw KJ, Goodwin TM 1999 Reversible peripartum liver failure: a new perspective on the diagnosis, treatment, and cause of acute fatty liver of pregnancy, based on 28 consecutive cases. Am J Obstet Gynecol 181: 389–395
Moise KJ Jr, Shah DM 1987 Acute fatty liver of pregnancy: etiology of fetal distress and fetal wastage. Obstet Gynecol 69: 482–485
Knopp RH, Warth MR, Charles D, Childs M, Li JR, Mabuchi H, Van Allen MI 1986 Lipoprotein metabolism in pregnancy, fat transport to the fetus, and the effects of diabetes. Biol Neonate 50: 297–317
Wilcken B, Leung KC, Hammond J, Kamath R, Leonard JV 1993 Pregnancy and fetal long-chain 3-hydroxyacyl coenzyme A dehydrogenase deficiency. Lancet 341: 407–408
Sims HF, Brackett JC, Powell CK, Treem WR, Hale DE, Bennett MJ, Gibson B, Shapiro S, Strauss AW 1995 The molecular basis of pediatric long chain 3-hydroxyacyl-CoA dehydrogenase deficiency associated with maternal acute fatty liver of pregnancy. Proc Natl Acad Sci U S A 92: 841–845
Ibdah JA, Bennett MJ, Rinaldo P, Zhao Y, Gibson B, Sims HF, Strauss AW 1999 A fetal fatty-acid oxidation disorder as a cause of liver disease in pregnant women. N Engl J Med 340: 1723–1731
Yang Z, Zhao Y, Bennett MJ, Strauss AW, Ibdah JA 2002 Fetal genotypes and pregnancy outcomes in 35 families with mitochondrial trifunctional protein mutations. Am J Obstet Gynecol 187: 715–720
Spiekerkoetter U, Sun B, Khuchua Z, Bennett MJ, Strauss AW 2003 Molecular and phenotypic heterogeneity in mitochondrial trifunctional protein deficiency due to beta-subunit mutations. Hum Mutat 21: 598–607
Treem WR, Shoup ME, Hale DE, Bennett MJ, Rinaldo P, Millington DS, Stanley CA, Riely CA, Hyams JS 1996 Acute fatty liver of pregnancy, hemolysis, elevated liver enzymes, and low platelets syndrome, and long chain 3-hydroxyacyl-coenzyme A dehydrogenase deficiency. Am J Gastroenterol 91: 2293–2300
Isaacs JD Jr, Sims HF, Powell CK, Bennett MJ, Hale DE, Treem WR, Strauss AW 1996 Maternal acute fatty liver of pregnancy associated with fetal trifunctional protein deficiency: molecular characterization of a novel maternal mutant allele. Pediatr Res 40: 393–398
Nelson J, Lewis B, Walters B 2000 The HELLP syndrome associated with fetal medium-chain acyl-CoA dehydrogenase deficiency. J Inherit Metab Dis 23: 518–519
Matern D, Hart P, Murtha AP, Vockley J, Gregersen N, Millington DS, Treem WR 2001 Acute fatty liver of pregnancy associated with short-chain acyl-coenzyme A dehydrogenase deficiency. J Pediatr 138: 585–588
Bok LA, Vreken P, Wijburg FA, Wanders RJ, Gregersen N, Corydon MJ, Waterham HR, Duran M 2003 Short-chain Acyl-CoA dehydrogenase deficiency: studies in a large family adding to the complexity of the disorder. Pediatrics 112: 1152–1155
Innes AM, Seargeant LE, Balachandra K, Roe CR, Wanders RJ, Ruiter JP, Casiro O, Grewar DA, Greenberg CR 2000 Hepatic carnitine palmitoyltransferase I deficiency presenting as maternal illness in pregnancy. Pediatr Res 47: 43–45
Shekhawat P, Bennett MJ, Sadovsky Y, Nelson DM, Rakheja D, Strauss AW 2003 Human placenta metabolizes fatty acids: implications for fetal fatty acid oxidation disorders and maternal liver diseases. Am J Physiol Endocrinol Metab 284: E1098–E1105
Rakheja D, Bennett MJ, Foster BM, Domiati-Saad R, Rogers BB 2002 Evidence for fatty acid oxidation in human placenta, and the relationship of fatty acid oxidation enzyme activities with gestational age. Placenta 23: 447–450
Oey NA, den Boer ME, Ruiter JP, Wanders RJ, Duran M, Waterham HR, Boer K, van der Post JA, Wijburg FA 2003 High activity of fatty acid oxidation enzymes in human placenta: implications for fetal-maternal disease. J Inherit Metab Dis 26: 385–392
Thiele IG, Niezen-Koning KE, van Gennip AH, Aarnoudse JG 2004 Increased plasma carnitine concentrations in preeclampsia. Obstet Gynecol 103: 876–880
Kurtz DM, Rinaldo P, Rhead WJ, Tian L, Millington DS, Vockley J, Hamm DA, Brix AE, Lindsey JR, Pinkert CA, O'Brien WE, Wood PA 1998 Targeted disruption of mouse long-chain acyl-CoA dehydrogenase gene reveals crucial roles for fatty acid oxidation. Proc Natl Acad Sci U S A 95: 15592–15597
Cox KB, Hamm DA, Millington DS, Matern D, Vockley J, Rinaldo P, Pinkert CA, Rhead WJ, Lindsey JR, Wood PA 2001 Gestational, pathologic and biochemical differences between very long-chain acyl-CoA dehydrogenase deficiency and long-chain acyl-CoA dehydrogenase deficiency in the mouse. Hum Mol Genet 10: 2069–2077
Ibdah JA, Paul H, Zhao Y, Binford S, Salleng K, Cline M, Matern D, Bennett MJ, Rinaldo P, Strauss AW 2001 Lack of mitochondrial trifunctional protein in mice causes neonatal hypoglycemia and sudden death. J Clin Invest 107: 1403–1409
Barak Y, Nelson MC, Ong ES, Jones YZ, Ruiz-Lozano P, Chien KR, Koder A, Evans RM 1999 PPAR gamma is required for placental, cardiac, and adipose tissue development. Mol Cell 4: 585–595
Barak Y, Liao D, He W, Ong ES, Nelson MC, Olefsky JM, Boland R, Evans RM 2002 Effects of peroxisome proliferator-activated receptor delta on placentation, adiposity, and colorectal cancer. Proc Natl Acad Sci U S A 99: 303–308
Lim H, Gupta RA, Ma WG, Paria BC, Moller DE, Morrow JD, DuBois RN, Trzaskos JM, Dey SK 1999 Cyclo-oxygenase-2-derived prostacyclin mediates embryo implantation in the mouse via PPARdelta. Genes Dev 13: 1561–1574
Chirala SS, Chang H, Matzuk M, Abu-Elheiga L, Mao J, Mahon K, Finegold M, Wakil SJ 2003 Fatty acid synthesis is essential in embryonic development: fatty acid synthase null mutants and most of the heterozygotes die in utero. Proc Natl Acad Sci U S A 100: 6358–6363
Spiekerkotter U, Schwahn B, Korall H, Trefz FK, Andresen BS, Wendel U 2000 Very-long-chain acyl-coenzyme A dehydrogenase (VLCAD) deficiency: monitoring of treatment by carnitine/acylcarnitine analysis in blood spots. Acta Paediatr 89: 492–495
Gillingham MB, Connor WE, Matern D, Rinaldo P, Burlingame T, Meeuws K, Harding CO 2003 Optimal dietary therapy of long-chain 3-hydroxyacyl-CoA dehydrogenase deficiency. Mol Genet Metab 79: 114–123
Rinaldo P, Yoon HR, Yu C, Raymond K, Tiozzo C, Giordano G 1999 Sudden and unexpected neonatal death: a protocol for the postmortem diagnosis of fatty acid oxidation disorders. Semin Perinatol 23: 204–210
Bennett MJ, Rinaldo P 2001 The metabolic autopsy comes of age. Clin Chem 47: 1145–1146
Wilcken B, Wiley V, Hammond J, Carpenter K 2003 Screening newborns for inborn errors of metabolism by tandem mass spectrometry. N Engl J Med 348: 2304–2312
Rinaldo P, Studinski AL, Matern D 2001 Prenatal diagnosis of disorders of fatty acid transport and mitochondrial oxidation. Prenat Diagn 21: 52–54
Tanaka K, Budd MA, Efron ML, Isselbacher KJ 1966 Isovaleric acidemia: a new genetic defect of leucine metabolism. Proc Natl Acad Sci U S A 56: 236–242
Millington DS, Maltby DA, Roe CR 1986 Rapid detection of argininosuccinic aciduria and citrullinuria by fast atom bombardment and tandem mass spectrometry. Clin Chim Acta 155: 173–178
Chace DH 2003 Mass spectrometry-based diagnostics: the upcoming revolution in disease detection has already arrived. Clin Chem 49: 1227–1229
Chace DH, Kalas TA, Naylor EW 2003 Use of tandem mass spectrometry for multianalyte screening of dried blood specimens from newborns. Clin Chem 49: 1797–1817
Matern D, Magera MJ 2001 Mass spectrometry methods for metabolic and health assessment. J Nutr 131: 1615S–1620S
Chace DH 2001 Mass spectrometry in the clinical laboratory. Chem Rev 101: 445–477
Chace DH, Millington DS, Terada N, Kahler SG, Roe CR, Hofman LF 1993 Rapid diagnosis of phenylketonuria by quantitative analysis for phenylalanine and tyrosine in neonatal blood spots by tandem mass spectrometry. Clin Chem 39: 66–71
Chace DH, Hillman SL, Van Hove JL, Naylor EW 1997 Rapid diagnosis of MCAD deficiency: quantitatively analysis of octanoylcarnitine and other acylcarnitines in newborn blood spots by tandem mass spectrometry. Clin Chem 43: 2106–2113
Schulze A, Lindner M, Kohlmuller D, Olgemoller K, Mayatepek E, Hoffmann GF 2003 Expanded newborn screening for inborn errors of metabolism by electrospray ionization-tandem mass spectrometry: results, outcome, and implications. Pediatr 111: 1399–1406
Matern D, Strauss AW, Hillman SL, Mayatepek E, Millington DS, Trefz FK 1999 Diagnosis of mitochondrial trifunctional protein deficiency in a blood spot from the newborn screening card by tandem mass spectrometry and DNA analysis. Pediatr Res 46: 45–49
Schwab KO, Ensenauer R, Matern D, Uyanik G, Schnieders B, Wanders RA, Lehnert W 2003 Complete deficiency of mitochondrial trifunctional protein due to a novel mutation within the beta-subunit of the mitochondrial trifunctional protein gene leads to failure of long-chain fatty acid beta-oxidation with fatal outcome. Eur J Pediatr 162: 90–95
Hintz SR, Matern D, Strauss A, Bennett MJ, Hoyme HE, Schelley S, Kobori J, Colby C, Lehman NL, Enns GM 2002 Early neonatal diagnosis of long-chain 3-hydroxyacyl coenzyme a dehydrogenase and mitochondrial trifunctional protein deficiencies. Mol Genet Metab 75: 120–127
Millington D, Koeberl D 2003 Metabolic screening in the newborn. Growth, Genetics and Hormones 19: 33–38
Hoffmann GF, von Kries R, Klose D, Lindner M, Schulze A, Muntau AC, Roschinger W, Liebl B, Mayatepek E, Roscher AA 2004 Frequencies of inherited organic acidurias and disorders of mitochondrial fatty acid transport and oxidation in Germany. Eur J Pediatr 163: 76–80
Levy HL, Albers S 2000 Genetic screening of newborns. Annu Rev Genomics Hum Genet 1: 139–177
Schoen EJ, Baker JC, Colby CJ, To TT 2002 Cost-benefit analysis of universal tandem mass spectrometry for newborn screening. Pediatrics 110: 781–786
Pollitt RJ, Green A, McCabe CJ, Booth A, Cooper NJ, Leonard JV, Nicholl J, Nicholson P, Tunaley JR, Virdi NK 1997 Neonatal screening for inborn errors of metabolism: cost, yield and outcome. Health Technol Assess 1: i–iv, 1–202
Insinga RP, Laessig RH, Hoffman GL 2002 Newborn screening with tandem mass spectrometry: examining its cost-effectiveness in the Wisconsin Newborn Screening Panel. J Pediatr 141: 524–531
Waisbren SE, Albers S, Amato S, Ampola M, Brewster TG, Demmer L, Eaton RB, Greenstein R, Korson M, Larson C, Marsden D, Msall M, Naylor EW, Pueschel S, Seashore M, Shih VE, Levy HL 2003 Effect of expanded newborn screening for biochemical genetic disorders on child outcomes and parental stress. JAMA 290: 2564–2572
McCann M, Rinaldo P, Matern D, Hahn SH, Berry S, Whitley C, Schimmenti L 2004 Expanded newborn screening: The Minnesota model. Proceedings of the 2004 Newborn Screening and Genetic Testing Symposium, Atlanta, GA, May 2004; pp 107
Chace DH, DiPerna JC, Mitchell BL, Sgroi B, Hofman LF, Naylor EW 2001 Electrospray tandem mass spectrometry for analysis of acylcarnitines in dried postmortem blood specimens collected at autopsy from infants with unexplained cause of death. Clin Chem 47: 1166–1182
Wilcox RL, Nelson CC, Stenzel P, Steiner RD 2002 Postmortem screening for fatty acid oxidation disorders by analysis of Guthrie cards with tandem mass spectrometry in sudden unexpected death in infancy. J Pediatr 141: 833–836
Shigematsu Y, Hirano S, Hata I, Tanaka Y, Sudo M, Sakura N, Tajima T, Yamaguchi S 2002 Newborn mass screening and selective screening using electrospray tandem mass spectrometry in Japan. J Chromatogr B Analyt Technol Biomed Life Sci 776: 39–48
Andresen BS, Dobrowolski SF, O‘Reilly L, Muenzer J, McCandless SE, Frazier DM, Udvari S, Bross P, Knudsen I, Banas R, Chace DH, Engel P, Naylor EW, Gregersen N 2001 Medium-chain acyl-CoA dehydrogenase (MCAD) mutations identified by MS/MS-based prospective screening of newborns differ from those observed in patients with clinical symptoms: identification and characterization of a new, prevalent mutation that results in mild MCAD deficiency. Am J Hum Genet 68: 1408–1418
Carpenter K, Wiley V, Sim KG, Heath D, Wilcken B 2001 Evaluation of newborn screening for medium chain acyl-CoA dehydrogenase deficiency in 275,000 babies. Arch Dis Child Fetal Neonatal Ed 85: F105–F109
Zytkovicz TH, Fitzgerald EF, Marsden D, Larson CA, Shih VE, Johnson DM, Strauss AW, Comeau AM, Eaton RB, Grady GF 2001 Tandem mass spectrometric analysis for amino, organic, and fatty acid disorders in newborn dried blood spots: a two-year summary from the New England Newborn Screening Program. Clin Chem 47: 1945–1955
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported in part by a combined intramural grant of University System of Georgia and National Institutes of Health grants HL 5R01DK061762-05 and HD 048867-01.
Rights and permissions
About this article
Cite this article
Shekhawat, P., Matern, D. & Strauss, A. Fetal Fatty Acid Oxidation Disorders, Their Effect on Maternal Health and Neonatal Outcome: Impact of Expanded Newborn Screening on Their Diagnosis and Management. Pediatr Res 57, 78–86 (2005). https://doi.org/10.1203/01.PDR.0000159631.63843.3E
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000159631.63843.3E
This article is cited by
-
Estimating the Prevalence of Rare Diseases: Long-Chain Fatty Acid Oxidation Disorders as an Illustrative Example
Advances in Therapy (2022)
-
Repression of the transcriptional activity of ERRα with sequence-specific DNA-binding polyamides
Medicinal Chemistry Research (2020)
-
Clinical manifestations and management of fatty acid oxidation disorders
Reviews in Endocrine and Metabolic Disorders (2020)
-
Management and diagnosis of mitochondrial fatty acid oxidation disorders: focus on very-long-chain acyl-CoA dehydrogenase deficiency
Journal of Human Genetics (2019)
-
Acute Fatty Liver Disease of Pregnancy: Updates in Pathogenesis, Diagnosis, and Management
American Journal of Gastroenterology (2017)