Abstract
The aim of this study was to determine the validity of the hypothesis that excitatory amino acids are related to phosphorylation potential during primary and secondary cerebral energy failure observed in asphyxiated infants. We report here the results of experiments using newborn piglets subjected to severe transient cerebral hypoxia-ischemia followed by resuscitation. We examined cerebral energy metabolism by phosphorus nuclear magnetic resonance spectroscopy and changes in levels of amino acid neurotransmitters in the cortex by microdialysis before, during, and up to 24 h after the hypoxic-ischemic insult. The concentrations of aspartate, glutamate, taurine, and γ-aminobutyric acid were significantly elevated during the hypoxic-ischemic insult compared with prebaseline values. Shortly after resuscitation, glutamate, taurine, and γ-aminobutyric acid concentrations decreased but then began to increase again. These secondary elevations were greater than the primary elevations. A negative linear correlation was found between primary interstitial levels of glutamate and taurine and minimum values of phosphocreatine/inorganic phosphate during the secondary energy failure. The cerebral energy state depended on the time course of changes in excitatory amino acids, suggesting that amino acids play distinct roles during the early and delayed phases of injury.
Similar content being viewed by others
Main
Perinatal hypoxic-ischemic encephalopathy remains a major cause of permanent neurodevelopmental disability and infant mortality (1–4). High-energy phosphate metabolites in the brains of asphyxiated infants studied by phosphorus nuclear magnetic resonance spectroscopy (31P-MRS) on the first day of life showed no differences from that in normal infants. However, inverse changes in the concentrations of phosphocreatine (PCr) and inorganic phosphate (Pi) cause a significant reduction in the [PCr]/[Pi] ratio over the next several days despite optimal medical management. Low values of [PCr]/[Pi] were founded to be associated with a very poor prognosis for survival and early neurodevelopmental outcome (5, 6). The late metabolic deterioration that characterizes such infants indicates that there is chronic metabolic stress and suggests that there may be a therapeutic window in which appropriate therapy could markedly improve outcome. The origin of this secondary energy failure is probably multifactorial and related to a combination of prolonged exposure to excitatory amino acids (which initiates cellular damage mediated by Ca2+ and nitric oxide), damage caused by free radicals, immunocytotoxic reactions, impairment of protein synthesis, lack of growth factors, and decreased cerebral blood flow and oxygen delivery as a result of progressive cerebral edema (7–9). Several methods for preventing secondary brain damage have been proposed (10–15).
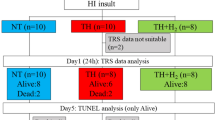
Some animal studies using 31P-MRS and proton magnetic resonance spectroscopy have demonstrated that transient hypoxia-ischemia is followed by impairment of energy metabolism 8–12 h after the initial injury (16–19). In this study, we subjected newborn piglets to severe transient cerebral hypoxic-ischemic insult followed by resuscitation, and we observed cerebral energy metabolism by 31P-MRS and changes in levels of amino acid neurotransmitters in the cortex by microdialysis before the insult, during the insult, and up to 24 h after the insult. The aim of this study was to determine the validity of the hypothesis that changes in excitatory amino acids are related to changes in phosphorylation potential during primary and secondary cerebral energy failure as assessed by 31P-MRS.
METHODS
Animal preparation.
The protocols for animal care were in compliance with institutional guidelines. Fifteen newborn piglets (seven used for the cerebral hypoxic-ischemic insult experiment and eight used as control) that were obtained within 24 h of birth and weighed 1.53–1.90 kg were each anesthetized with an intramuscular injection of sodium pentobarbital (2 mg/kg). The umbilical artery of each piglet was cannulated with a polyethylene tube for blood pressure monitoring and for blood sampling. A solution of 0.9% saline containing 1 U of heparin per 1 mL was infused at a rate of 2 mL/h through an arterial catheter attached to a strain-gauge blood pressure transducer. Maintenance solution (KN3B; Otsuka Pharmaceutical Co., Tokyo, Japan) was infused continuously at a rate of 4 mL · kg−1 · h−1via the umbilical vein. Each piglet was then paralyzed with pancuronium bromide at an initial dose of 0.1 mg/kg followed by infusion at 0.1 mg · kg−1 · h−1, anesthetized with fentanyl citrate at an initial dose of 10 μg/kg followed by infusion at 5 μg · kg−1 · h−1, intubated, and mechanically ventilated with an infant ventilator. Fraction of inspired oxygen (Fio2) was monitored with an oxygen electrode and adjusted to provide a Pao2 level of 70–100 mm Hg. Paco2 was maintained in the range of 35–45 mm Hg. Respiration and acid-base balance were checked by arterial blood gas analysis before, during, and after the hypoxic-ischemic insult. Ampicillin and cloxacillin sodium (100 mg/kg) were given every 12 h to prevent infection. Pao2, Paco2, pH, electrolyte, glucose, and lactate levels were measured by standard techniques. Throughout the experiment, rectal temperature was monitored and maintained between 38.0°C and 39.0°C using a heated-water mattress.
Microdialysis methods.
Each piglet was then placed in the prone position with the head positioned in a stereotaxic holder. The scalp was removed to expose the skull. A hole of approximately 3 mm in diameter was drilled through the skull. A microdialysis probe was inserted through the dura and implanted in the cerebral cortex (4 mm posterior and 4 mm lateral to the bregma and 6 mm vertical from the dura) in the position of the 31P-MRS surface coil. Several pilot studies were performed before the present study to determine accurately the coordinates for the cerebral cortex. The probe was perfused with artificial CSF (148 mM of NaCl, 2.7 mM of KCl, 1.2 mM of CaCl2, and 0.85 mM of MgCl2) at a flow rate of 2.0 μL/min using a microinfusion pump (Eicom, Kyoto, Japan). After an equilibrium period of 6 h, samples were collected 1 h before, during, and 3 h after the insult and then every 3 h until 24 h after the insult.
HPLC analysis.
The HPLC system consisted of a liquid chromatograph pump (LC-9A; Shimadzu, Kyoto, Japan), spectrofluorometric detector (RF10A; Shimadzu), and integrator (Chromatopac C-R6A; Shimadzu). The dialysates were kept at −80°C until analysis. Amino acids were analyzed using gradient HPLC with fluorescence detection and prelabeled derivitization with o-phthaldialdehyde according to the method previously reported (20). The perfusate (30 μL) was reacted with 10 μL of 20 mM o-phthalaldehyde regent. After a 2.5-min reaction period at 10.0°C, 10 μL of the derivatized sample mixture was autoinjected into the HPLC system (Gilson Model-231XL; Gilson, Villiersle Bel, France). Amino acid derivatives were then separated at a flow rate of 0.23 mL/min on an Eicompack SC-5ODS column (2.1φ × 150 mm; Eicom) using an isocratic mobile phase of 70% sodium phosphate buffer (0.1 M, pH 6.0) and 30% methanol containing 5 mg of EDTA-2 Na. The concentrations of amino acids in the perfusate were measured by the peak area fluorescent intensity at an excitation of 340 nm and an emission of 445 nm and calculated by measurement.
31P-MRS.
A 2.0 Tesla P-NMR spectroscopy system (Model BEM 250/80, 2.0 Tesla; Otsuka-Electronics, Osaka, Japan) was used to measure [PCr] and [Pi]. A surface coil of 3 cm in diameter was placed on the top of the skull with the scalp removed. A mean value of 0.4 ppm for the half-height line width in the water peak was established by shimming. A radio frequency pulse of 35.8 MHz was transmitted and received with the same coil at a pulse interval of 2.0 s. The conditions for measurement were a spectral width of 5 kHz, spectral data size of 1024 points, a 25-μs pulse width, and sum of 150 samples (total 5 min). We recognized that optimal spectral analysis is facilitated by a curve-fitting deconvolution routine. However, because a curve-fitting deconvolution routine is not available and a linear correlation was demonstrated between metabolite ratios calculated from peak heights and peak area (21), the spectra were analyzed by measuring the peak height from the baseline. [PCr]/[Pi] was calculated from the ratio of the [PCr] and [Pi] peak heights.
Hypoxic-ischemic insult.
After baseline observations, seven piglets underwent cerebral hypoxic-ischemic insult for 75–105 min (mean period, 87 min) induced by inflating a blood pressure cuff positioned around the piglet's neck and reducing the inspired oxygen fraction to 0.10–0.06. Tolazoline hydrochloride (1–3 mg/kg) was used to prevent a rise in blood pressure during the insult. After the [PCr] peak had disappeared and [β-ATP] had then decreased, the piglets were resuscitated if the [Pi] peak remained constant for a period of 20–25 min. Resuscitation was performed by stopping inflation of the blood pressure cuff and providing an Fio2 of 0.60, which was reduced as appropriate to normalize Pao2 after 30 min of resuscitation. Observations were continued for 24 h after resuscitation. During this period, all piglets received 10–20 mL of 5% pig albumin solution and noradrenaline to prevent hypotension. A base excess value of <−5.0 mM, which was caused by hypoxia-ischemia, was corrected as much as possible by sodium bicarbonate infusion to maintain pH between 7.1 and 7.5. After 24 h, the animals were killed, and the brain of each animal was perfused through the left ventricle with 0.9% saline and phosphate-buffered paraformaldehyde for another histologic experiment.
Statistical analysis.
The Stat-View 5.01 package for the Macintosh computer was used for statistical analysis. Comparisons of values obtained in the animals that had been subjected to hypoxic-ischemic insult and the control animals were made by the Mann-Whitney U test for physiologic parameters and [PCr]/[Pi] values. Analysis of amino acids was carried out by repeated-measures ANOVA using values obtained from 3 h after resuscitation. Values obtained at different times after baseline were compared by Wilcoxon's signed-rank test. The level of statistical significance was set at a probability of p < 0.05 for all tests. All measurement results are expressed as means ± SD.
RESULTS
Physiologic parameters.
Heart rates; mean arterial blood pressures; rectal temperatures; and levels of arterial pH, Pao2, Paco2, blood glucose, and lactate in the control group and experimental group are shown in Tables 1 and 2, respectively. No changes occurred during the 24-h period in the control group. In the experimental group, the most significant changes were decreases in heart rate, mean arterial blood pressure, arterial pH, and Pao2 and increase in lactate from the preinsult values during the period of acute hypoxic-ischemic insult. These values, except for that of lactate, subsequently returned to normal. Blood glucose level increased from 6 h after resuscitation.
31P MRS.
Data for [PCr]/[Pi] in the control and experimental groups are summarized in Figure 1. No changes occurred during the 24-h period in the control group. In the experimental group, [PCr]/[Pi] decreased during the insult from 1.50 (± 0.22) to 0.27 (± 0.12). This decrease was due to a reduction in [PCr] together with a reciprocal and then larger increase in [Pi]. [PCr]/[Pi] became more than 1, close to the baseline value, at 2–3 h after resuscitation, and thereafter progressively decreased. At 24 h after the insult, the [PCr]/[Pi] ratio had decreased to a minimum value (0.01–1.09) despite that there was no acidosis, hypoxia, or hypotension.
Values of [PCr]/[Pi] in the control group (•; n = 8) and insult group of piglets whose brains were subjected to acute hypoxia-ischemia (○; n = 7). Each value is the mean and SD. Time 0 means the start of resuscitation after hypoxia-ischemia. *p < 0.05 vs preinsult basal level using Wilcoxon's signed rank test; #p < 0.05 vs control group using the Mann-Whitney U test.
Changes in interstitial levels of amino acids during the insult.
The baseline interstitial values of amino acids in the cortical dialysate samples from 15 piglets are shown in Table 3. The levels of amino acids in the dialysate increased shortly after the onset of insult (Fig. 2), and the levels of all amino acids except glutamine reached a peak during a period of 2 h after resuscitation. The levels of those amino acids decreased after resuscitation. The level of taurine decreased slightly after resuscitation but remained significantly higher than the baseline level for 3 h into reperfusion.
Amino acid concentrations in dialysate (mean ± SD) in the control group (•; n = 8) and insult group (○; n = 7). Time 0 means the start of resuscitation after hypoxia-ischemia. Ala, alanine; Arg, arginine; Asp, aspartate; Asn, asparagine; Glu, glutamate; Gln, glutamine; Ser, serine; Tau, taurine. *p < 0.05 vs preinsult basal level using Wilcoxon's signed rank test; #p < 0.05 vs control group from 3 to 24 h after the start of resuscitation using repeated-measures ANOVA.
Changes in interstitial levels of amino acids during the period of secondary energy failure.
In the experimental group, the concentrations of all amino acids except taurine and glutamine briefly normalized shortly after resuscitation. The concentrations of all amino acids then began to increase again and were higher than the baseline concentrations at 24 h after reperfusion. These secondary elevations reached levels that were comparable with or even greater than the primary elevations. However, the amino acids for which the levels increased to significantly higher levels than the baseline levels were glutamate, taurine, and alanine. The levels of those amino acids as well as that of γ-aminobutyric acid (GABA) were significantly higher than the levels in the control group at 24 h after resuscitation.
Correlations between primary interstitial levels of amino acids and acute depletion of [PCr]/[Pi] during the insult.
The severity of the cerebral acute cerebral hypoxic-ischemic insults was determined by the time integral of depletion of [PCr]/[Pi] in the period from 1 h before resuscitation to 3 h after resuscitation. The area under the curve of total interstitial level of amino acids from the period of insult to 3 h after resuscitation was defined as primary amino acid interstitial level. As indicated by the results of linear regression analysis presented in Figure 3, primary glutamate and taurine interstitial levels in the experimental group showed negative correlations with the time integral of depletion of [PCr]/[Pi] during the insult. However, there were no significant correlations in interstitial levels of aspartate, asparagine, serine, glutamine, arginine, alanine, and GABA.
Correlations between the severity of acute cerebral hypoxic-ischemic insults as shown by the time integral of depletion of [PCr]/[Pi] in the period from 1 h before resuscitation to 3 h after resuscitation and the primary interstitial level of amino acids. Primary interstitial level of amino acid was calculated as the sum of dialysate content during the period from insult to 3 h after resuscitation. Ala, alanine; Asn, asparagine; Arg, arginine; Asp, aspartate; Glu, glutamate; Gln, glutamine; Ser, serine; Tau, taurine.
Correlations between primary interstitial levels of amino acids and minimum values of [PCr]/[Pi] during the secondary energy failure stage.
As indicated by the results of linear regression analysis presented in Figure 4, primary interstitial levels of glutamate, serine, taurine, and alanine in the experimental group showed negative correlations with minimum values of [PCr]/[Pi] during the period of secondary energy failure. However, there were no significant correlations in interstitial levels of aspartate, asparagine, glutamine, arginine, and GABA.
Correlations between the severity of subsequent secondary energy failure as shown by the minimum values of [PCr]/[Pi] at 3–24 h and interstitial levels of amino acids during the period from insult to 3 h after resuscitation. Ala, alanine; Asn, asparagine; Arg, arginine; Asp, aspartate; Glu, glutamate; Gln, glutamine; Ser, serine; Tau, taurine.
DISCUSSION
The present findings demonstrate a distinct sequence of changes in the concentrations of amino acids during the early and delayed phases of hypoxic-ischemic injury. It is particularly notable that the interstitial levels of glutamate, serine, taurine, and alanine during hypoxic-ischemic insult showed significant negative correlations with minimum values of [PCr]/[Pi] during the period of secondary energy failure.
Results of several studies using animal models of secondary energy failure in asphyxiated infants have been reported (22). Lorek et al.(16) reported that levels of brain high-energy phosphate compounds declined to 30% of baseline levels in piglets during a reversible hypoxic-ischemic insult induced by temporarily occluding both of the carotid arteries, progressively reducing Fio2, and preventing hypertension by using isoflurane. The severity of secondary energy failure, as judged by the lowest [PCr]/[Pi] recorded during the period of 24–48 h, was found to be directly related to the extent of acute energy depletion, calculated as the time integral of reduction in [nucleotide triphosphate concentration]/[exchangeable phosphate pool concentration]. Laptook et al.(23) used a piglet model in which ischemia was induced by combining neck compression with hemorrhagic hypotension and in which the severity of brain ischemia was measured by 31P-MRS. LeBlanc et al.(24) used newborn piglets in which both carotid arteries were reversibly ligated, blood pressure was reduced by one third by hemorrhage, and hypoxia was induced by reducing inspired oxygen. In the present study, we used a newborn piglet model of hypoxia-ischemia that was induced by combining neck compression with hypotension using tolazoline hydrochloride and hypoxia. We found that [PCr]/[Pi] decreased during the hypoxic-ischemic insult to 0.27 and became more than 1, close to the baseline level, at 2–3 h after resuscitation and thereafter progressively decreased despite that there was no acidosis, hypoxia, or hypotension. These results indicate that our hypoxic-ischemic piglet model is suitable as a model of secondary energy failure in asphyxiated infants.
Our results showed that extracellular levels of amino acids increased during the period of transient hypoxia-ischemia and that the primary interstitial level of glutamate had significant negative correlations with acute depletion of [PCr]/[Pi] during the insult and minimum values of [PCr]/[Pi] during the period of secondary energy failure. Results of in vivo microdialysis studies using various animal models of cerebral ischemia have shown that large elevations in concentrations of excitatory amino acids occur during ischemia (25–27). Increase in synaptic glutamate levels results in excessive release of glutamate from nerve terminals and reduces uptake of glutamate by re-uptake pumps on glial cells, the action of which normally keeps synaptic glutamate levels low. An increase in glutamate to a high level will trigger excessive activity at glutamate receptors and eventually excitotoxicity to damage of neurons (8). Furthermore, several studies have shown additional excitotoxicity after reperfusion. Lin et al.(28) reported the occurrence of larger secondary amino acid elevations during reperfusion after multiple ischemic insults that was not seen after a single ischemic insult. Tan et al.(29) found by using a fetal sheep that nitric oxide synthesis increased several hours after a severe hypoxic-ischemic injury and that seizures then occurred and edema developed concomitantly with accumulation of excitatory amino acids. The secondary rise in cortical glutamate concentration corresponds to that in the level of seizure activity. Matsumoto et al.(30) reported that the large secondary elevation in concentrations of transmitter amino acids occurred in the reperfusion phase after 2 h of transient focal ischemia in a rabbit model. They found correlations between primary (ischemic) and secondary (reperfusion) transmitter interstitial levels, suggesting that secondary elevations are related to the severity of the primary insult. Their results and our results indicate that primary and secondary increments in concentrations of excitatory amino acids are one of the factors that cause delayed secondary energy failure. However, we could not determine whether energy change drove amino acids or vice versa in the later phase, and further study is needed.
In this study, taurine concentration increased shortly after the onset of insult and increased again during the secondary energy failure. Taurine is one of the most abundant free amino acids in the CNS and plays a special role in immature brain tissue. This inhibitory amino acid is known to protect neural cells from the excitotoxicity induced by excitatory amino acids and is known as an osmoregulator and neuromodulator (31–33). The extracellular concentrations of taurine have been measured by microdialysis in several animal models of ischemic injury. The levels have been found to be increased in the rat striatum (34) and rabbit cerebral cortex (30) after transient focal ischemia. Taurine release during ischemia may be enhanced by several mechanisms, including Ca2+-dependent membrane transporters and facilitation of diffusion. Moreover, it has been suggested that the enhanced release of excitatory amino acids during ischemia may stem from membrane permeability changes elicited by the activation of phospholipases by elevation of intracellular Ca2+(35). Taurine efflux may also be a consequence of a regulatory volume decrease possibly mediated by ion channels and triggered as a response to ischemia-induced cell swelling (36). Thus, the increases in the concentration of taurine are thought to be due to increases in its extracellular level as a result of neuroprotective action and energy failure.
CONCLUSION
In summary, we evaluated the temporal profile of changes in concentrations of extracellular amino acids during hypoxic-ischemic insult and after resuscitation. The cerebral energy state was found to depend on changes in excitatory amino acids, suggesting that the amino acids play distinct roles during the early and delayed phases of injury.
Abbreviations
- Fio2:
-
fraction of inspired oxygen
- GABA:
-
γ-aminobutyric acid
- PCr:
-
phosphocreatine
- Pi:
-
inorganic phosphate
- 31P-MRS:
-
phosphorus nuclear magnetic resonance spectroscopy
References
Volpe JJ 2001 Hypoxic-ischemic encephalopathy: clinical aspects. In: Volpe JJ (ed) Neurology of the Newborn, 4th Ed. W.B. Saunders Company, Philadelphia, 331–394.
Vannucci RC 2000 Hypoxic-ischemic encephalopathy. Am J Perinatol 17: 113–120
Jin SH, Edwards JN Jr 1997 Hypoxic-ischemic encephalopathy. In: Stevenson DK, Sunshine P (eds) Fetal and Neonatal Brain Injury, 2nd Ed. Oxford University Press, Oxford, 277–286.
Whitelaw A, Thoresen M 2002 Clinical assessment and therapeutic interventions for hypoxic-ischemic encephalopathy in the full term infant. In: Lagercrantz H, Hanson M, Evrard P, Rodeck CH (eds) The Newborn Brain. Cambridge University Press, Cambridge, 415–442.
Younkin DP, Delivoria-Papadopolus M, Leonard J, Subramanian VH, Eleff S, Leigh JS, Chance B 1984 Unique aspects of human newborn cerebral metabolism evaluated with phosphorus nuclear magnetic resonance spectroscopy. Ann Neurol 6: 581–586
Hope PL, Costello AM, Cady EB, Delpy DT, Tofts PS, Chu A, Hamilton PA, Reynolds EOR, Wilkie DR 1984 Cerebral energy metabolism studied with phosphorus NMR spectroscopy in normal and birth-asphyxiated infants. Lancet 2: 366–370
Edwards AD, Mehmet H, Hagberg H 2002 Hypoxic-ischemic encephalopathy. In: Lagercrantz H, Hanson M, Evrard P, Rodeck CH (eds) The Newborn Brain. Cambridge University Press, Cambridge, 385–414.
Johnston MV, Trescher WH, Ishida A, Nakajima W 2001 Neurobiology of hypoxic-ischemic injury in the developing brain. Pediatr Res 49: 735–741
Feelman V, Ravio KO 1997 Reperfusion injury as the mechanism of brain damage after perinatal asphyxia. Pediatr Res 41: 599–606
Vannucci RC, Perlman JM 1997 Interventions for perinatal hypoxic-ischemic-encephalopathy. Pediatrics 100: 1004–1014
Wyatt JS, Thoresen M 1997 Hypothermia treatment and the newborn. Pediatrics 100: 1028–1030
Penrice J, Amess PN, Punwani S, Wylezinska M, Tyszczuk L, D'Souza P, Edwards AD, Cady EB, Wyatt JS, Reynolds EOR 1997 Magnesium sulfate after transient hypoxia-ischemia fails to prevent delayed cerebral energy failure in the newborn piglet. Pediatr Res 41: 443–447
Bona E, Hagberg H, Loberg EM, Bagenholm R, Thoresen M 1998 Protective effects of moderate hypothermia after neonatal hypoxia-ischemia: short- and long-term outcome. Pediatr Res 43: 738–745
Van Bel F, Shadid M, Moison RM, Dorrepaal CA, Fontijn J, Monteiro L, Van De Bor M, Berger HM 1998 Effect of allopurinol on postasphyxial free radical formation, cerebral hemodynamics, and electrical brain activity. Pediatrics 101: 185–193
Ichiba H, Tamai H, Negishi H, Ueda T, Kim TJ, Sumida Y, Takahashi Y, Fujinaga H, Minami H, Kansai Magnesium Study Group 2002 Randomized controlled trial of magnesium sulfate infusion for severe birth asphyxia. Pediatr Int 44: 505–509
Lorek A, Takei Y, Cady EB, Wyatt JS, Penrice J, Edwards AD, Peebles D, Wylezinska M, Owen-Reece H, Kirkbride V, Cooper CE, Aldridge RF, Roth SC, Brown G, Delpy DT, Reynolds EOR 1994 Delayed (“secondary”) cerebral energy failure after acute hypoxia-ischemia in newborn piglet: continuous 48-hour studies by phosphorus magnetic resonance spectroscopy. Pediatr Res 36: 699–706
Thoresen M, Penrice J, Lorek A, Cady EB, Wylezinska M, Kirkbride V, Cooper CE, Brown GC, Edwards AD, Wyatt JS, Reynolds EOR 1995 Mild hypothermia after severe transient hypoxia-ischemia ameliorates delayed cerebral energy failure in the newborn piglet. Pediatr Res 37: 667–670
Penrice J, Lorek A, Cady EB, Amess PN, Wylezinska M, Cooper CE, D'Souza P, Brown GC, Kirkbride V, Edwards AD, Wyatt JS, Reynolds EOR 1997 Proton magnetic resonance spectroscopy of the brain during acute hypoxia-ischemia and delayed cerebral energy failure in the newborn piglet. Pediatr Res 41: 795–802
Amess PN, Penrice J, Cady EB, Lorek A, Wylezinska M, Cooper CE, D'Souza P, Tyszczuk L, Thoresen M, Edwards AD, Wyatt JS, Reynolds EOR 1997 Mild hypothermia after severe transient hypoxia-ischemia reduces the delayed rise in cerebral lactate in the newborn piglet. Pediatr Res 41: 803–808
Lindroth P, Mopper K 1979 High performance liquid chromatographic determination of subpicomole amounts of amino acids by precolumn fluorescence derivatization with o-phthaldialdehyde. Anal Chem 51: 1667–1674
Younkin DP, Wagerle LC, Chance B, Maria J, Delivoria-Papadopoulos M 1987 31P-NMR studies of cerebral metabolic changes during graded hypoxia in newborn lambs. J Appl Physiol 62: 1569–1574
Roohey T, Raju TN, Moustogiannis AN 1997 Animal models for the study of perinatal hypoxic-ischemic encephalopathy: a critical analysis. Early Hum Dev 47: 115–146
Laptook AR, Corbett RJ, Sterett R, Burns DK, Garcia D, Tollefsbol G 1997 Modest hypothermia provides partial neuroprotection when used for immediate resuscitation after brain ischemia. Pediatr Res 42: 17–23
LeBlanc MH, Vig V, Smith B, Parker CC, Evans OB, Smith EE 1991 MK-801 does not protect against hypoxic-ischemic brain injury in piglets. Stroke 22: 1270–1275
Benveniste H, Drejer J, Schousboe A, Diemer NH 1984 Elevation of the extracellular concentrations of glutamate and aspartate in rat hippocampus during transient cerebral ischemia monitored by intracerebral microdialysis. J Neurochem 43: 1369–1374
Hillered L, Hallstrom A, Segersvard S, Persson L, Ungerstedt U 1990 Dynamics of extracellular metabolites in the striatum after middle cerebral artery occlusion in the rat monitored by intracerebral microdialysis. J Cereb Blood Flow Metab 9: 607–616
Shimizu H, Graham SH, Chang LH, Mintorovitch J, James TL, Faden AI, Weinstein PR 1993 Relationship between extracellular neurotransmitter amino acids and energy metabolism during cerebral ischemia in rats monitored by microdialysis and in vivo magnetic resonance spectroscopy. Brain Res 605: 33–42
Lin B, Globus MY, Dietrich WD, Busto R, Martinez E, Ginsberg MD 1992 Differing neurochemical and morphological sequelae of global ischemia: comparison of single- and multiple-insult paradigms. J Neurochem 59: 2213–2223
Tan WK, Williams CE, During MJ, Mallard CE, Gunning MI, Gunn AJ, Gluckman PD 1996 Accumulation of cytotoxins during the development of seizures and edema after hypoxic-ischemic injury in late gestation fetal sheep. Pediatr Res 39: 791–797
Matsumoto K, Lo EH, Pierce AR, Halpern EF, Newcomb R 1996 Secondary elevation of extracellular neurotransmitter amino acids in the reperfusion phase following focal cerebral ischemia. J Cereb Blood Flow Metab 16: 114–124
Fariello RG, Golden GT, Pisa M 1982 Homotaurine (3 aminopropanesulfonic acid; 3APS) protects from the convulsant and cytotoxic effect of systemically administered kainic acid. Neurology 32: 241–245
French ED, Vezzani A, Whetsell WO, Schwarcz R 1986 Anti-excitotoxic actions of taurine in the rat hippocampus studied in vivo and in vitro. Adv Exp Med Biol 203: 349–362
Trenkner E 1990 The role of taurine and glutamate during early postnatal cerebellar development of normal and weaver mutant mice. Adv Exp Med Biol 268: 239–244
Uchiyama-Tsuyuki Y, Araki H, Yae T, Otomo S 1994 Changes in the extracellular concentrations of amino acids in the rat striatum during transient focal cerebral ischemia. J Neurochem 62: 1074–1078
O'Regan MH, Smith-Barbour M, Perkins LM, Phillis JW 1995 A possible role for phospholipases in the release of neurotransmitter amino acids from ischemic rat cerebral cortex. Neurosci Lett 185: 191–194
Saransaari P, Oja SS 2000 Taurine and neural cell damage. Amino Acids 19: 509–526
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by grants-in-aid for scientific research (15591159, 14571051, and 13671140) and encouragement of young scientists (14770571 and 13770619) from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Rights and permissions
About this article
Cite this article
Kusaka, T., Matsuura, S., Fujikawa, Y. et al. Relationship between Cerebral Interstitial Levels of Amino Acids and Phosphorylation Potential during Secondary Energy Failure in Hypoxic-Ischemic Newborn Piglets. Pediatr Res 55, 273–279 (2004). https://doi.org/10.1203/01.PDR.0000102702.39608.82
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000102702.39608.82
This article is cited by
-
Conflicting findings on the effectiveness of hydrogen therapy for ameliorating vascular leakage in a 5-day post hypoxic-ischemic survival piglet model
Scientific Reports (2023)
-
Biomarkers of hypoxic–ischemic encephalopathy: a systematic review
World Journal of Pediatrics (2023)
-
Glucose and Intermediary Metabolism and Astrocyte–Neuron Interactions Following Neonatal Hypoxia–Ischemia in Rat
Neurochemical Research (2017)
-
Disrupted glutamate-glutamine cycle in acute encephalopathy with biphasic seizures and late reduced diffusion
Neuroradiology (2015)
-
Generation of lipid radicals in the hippocampus of neonatal rats after acute hypoxic-ischemic brain damage
Experimental Brain Research (2006)