Abstract
To examine the possible role of inflammatory cytokines in mediating neonatal brain injury, we investigated effects of intra-cerebral injection of IL-1beta (IL-1β) or tumor necrosis factor-alpha (TNFα) on brain injury in the neonatal rat. A stereotaxic intracerebral injection of IL-1βor TNFα(10 ng per pup) was performed in postnatal day 5 (P5) SD rats. Although no necrosis of neurons was found, increased astrogliosis, as indicated by GFAP positive staining was observed 24 and 72 h following the injection of IL-1βor TNFα. IL-1βinduced apoptotic cell death in the rat brain 24 h after the injection, as indicated by increases in positive TUNEL staining and caspase-3 activity, and apoptotic cell death was partially blocked by systemic administration of NBQX, an antagonist of the AMPA glutamate receptor. IL-1βalso significantly reduced the number of developing oligodendrocytes (OLs) 24 h after the injection and this impairment was not prevented by NBQX. On the contrary, TNFα induced a much smaller increase in the number of TUNEL positive cells and did not reduce the number of developing OLs. By P8, myelin basic protein (MBP) was clearly detected in the control rat brain, while MBP positive staining was very weak, if any, in the IL-1βtreated rat brain. MBP expression in the TNFα treated rat brain was less affected. The overall results indicate that IL-1β may directly cause injuries to developing OLs and impair myelination in the neonatal rat brain and TNFα may have different roles in mediating brain injury.
Similar content being viewed by others
Main
White matter disease, periventricular leukomalacia (PVL) in particular, is an important form of brain injury in very preterm infants, and is closely associated with severe neurologic disorders including cerebral palsy. Increasing evidence indicates that in addition to perinatal hypoxiaischemia (HI), maternal or placental infection may also be a major contributor to PVL (1–4) and that inflammatory cytokines derived from maternal infection are mediators between maternal infection and PVL in the infant brain (1,2,5).
Both clinical and experimental animal studies have provided supporting evidence for this hypothesis. Occurrence of PVL is frequently associated with increased concentrations of inflammatory cytokines such as tumor necrosis factor-α (TNFα), IL-1-β (IL-1β) and IL-6 in the infant brain (6–9), in the cord blood (10) or amniotic fluid (11). Maternal administration of endotoxin (lipopolysaccharide, LPS) induces PVL-like white matter injury in fetal sheep brain (12,13) and results in apoptotic cell death and gliosis in the offspring rat brain (14,15). White matter injuries in these studies are associated with the LPS-induced increase in expression of TNFα, IL-1βor IL-6 in the fetal or offspring brain (12,14,15). The protective effects of IL-1 receptor antagonists (IL-1ra) and/or soluble TNFα receptor or TNFα antibodies in HI-induced brain injury (16–21) have provided further evidence that inflammatory cytokines have important roles in mediating neonatal brain injury. However, the detailed role of inflammatory cytokines in mediating neuronal and/or white matter injury is still not completely understood. Controversial consequences following application of exogenous IL-1βor TNFα have been reported. Intracerebral injection of IL-1β has been found nonneurotoxic (19) or to induce apoptotic cell death and vasogenic edema (22) in the adult rat brain. In vitro studies show that IL-1β promotes oligodendrocyte (OL) death through glutamate excitotoxicity (23). TNFα induces damage to the blood-brain barrier in vivo (24) and causes death of OLs in vitro (25,26). TNFα has also been reported to attenuate NMDA or AMPA-induced neurotoxicity (27,28), to promote proliferation of OL progenitors and remyelination in vivo (29), and to protect neurons against amyloid-β-peptide toxicity in vitro (30).
In our previous work, we used an intracerebral injection of LPS to create a similar scenario as that during maternal infection. LPS is a component of the cell wall of Gram-negative bacteria and is responsible for most of the inflammatory effects of infection from Gram-negative bacteria. We found that intracerebral injection of LPS in the neonatal rat induced great increases in IL-1βand TNFα concentrations in the brain and resulted in selective white matter injury (31). Co-administration of LPS with IL-1ra, but not with antibodies to TNFα, protected the rat brain from LPS-induced white matter injury (32). To further examine the role of inflammatory cytokines in mediating brain injury, we investigated effects of intracerebral injection of IL-1βor TNFα on brain injury in the neonatal rat.
MATERIALS AND METHODS
Chemicals.
Unless otherwise stated, all chemicals used in this study were purchased from Sigma Chemical Co. (St. Louis, MO, U.S.A.). Recombinant rat IL-1βand rat TNFα, as well as Caspase-3 activity assay kit, were purchased from R&D System (Minneapolis, MN, U.S.A.). Monoclonal mouse antibodies against O4, O1 oligodendrocytes or myelin basic protein (MBP), and polyclonal rabbit antibodies against glial fibrillary acidic protein (GFAP) or NG2 were purchased from Chemicon (Temecula, CA, U.S.A.). Monoclonal mouse antibody against rat CD43 was purchased from Serotec (Raleigh, NC, U.S.A.). Apoptosis detection kit was purchased from Serologicals (Norcross, GA, U.S.A.).
Intracerebral injection and animal treatment.
Ninety-six rat pups were used in this study. The number of the rat pups injected with IL-1β or TNFα was 30 each. Twenty-two rat pups were injected with sterile saline containing 0.1% BSA (BSA) as the control. Eight rat pups were injected with IL-1βfollowed by intraperitoneal administration of 6-nitro-7-sulfamoylbenzoquinoxaline-2,3-dione (NBQX), an antagonist of the AMPA receptor. Six naïve rat brains were used for determination of the baseline level of caspase-3 activity and immunostaining. Intracerebral injection of IL-1βor TNFα to 5-d old Sprague-Dawley rat pups of both sexes was performed as previously described (31,32). Late OL progenitor cells, which have been proposed to be the major target in cerebral white matter injury in human infants (33), are the predominant OL lineage stage in the rat cerebral hemispheres between P2 to P7 (33). For ease of the stereotaxic injection, we performed intracerebral injection in P5 rats. Under light anesthesia with isoflurane (1.5%), IL-1βor TNFα (10 ng per rat pup) in sterile saline containing 0.1% BSA (total volume of 2 μL) was administered to the rat brain at the location of 1.0 mm posterior and 1.0 mm lateral to the bregma, and 2.0 mm deep to the skull surface at the left hemisphere in a stereotaxic apparatus with a neonatal rat adapter. The dose of IL-1βand TNFα was chosen based on the peak concentrations of IL-1βand TNFα achieved in the rat pup brain following LPS administration as reported previously (31,32) and on the published data (19,22). The injection was completed in 5 min and the needle was kept in this position for an additional 2 min and then retrieved slowly out of the brain. The wound was sutured and the pups were placed on a thermal blanket (34°C–35°C) for recovery before being returned to their dams. The accuracy of the injection site has been confirmed by the method of methyl green injection in some rat pups, as previously described (32). The injection site was located at the corpus callosum above the left ventricle. All animals survived the intracerebral injection. One and three days after the injection, rat pups were killed by transcardiac perfusion with normal saline followed by 4% paraformaldehyde for brain section preparation or by decapitation for brain tissue collection used in Caspase-3 activity assay. Consecutive frozen brain sections (near the injection site) in the thickness of 10 μm were prepared in a cryostat for immunohistochemistry and brain injury examination. To examine effects of inflammatory cytokines on developing OLs, free-floating brain sections (40 μm) were prepared in a freezing sliding microtome in the latter part of this study. For investigating mechanisms involved in the brain injury induced by IL-1β, intraperitoneal injection of NBQX (20 mg/kg) was performed immediately after IL-1βinjection and every 12 h thereafter until sacrifice, as described by Follett et al. (34). The experimental procedure was approved by the Institutional Animal Care and Use Committee at the University of Mississippi Medical Center and, in addition, was in accordance with the guidelines of the National Institutes of Health on the care and use of laboratory animals.
Immunohistochemical studies.
Brain injury was estimated based on the results of hematoxylin and eosin (H&E) staining and immunohistochemistry in consecutive frozen sections prepared from the rat brain 1 and 3 d (P6 and P8) after the intracerebral injection. For all brain injury studies, brain sections near the site of injection were used. Three sections from each brain were examined. For immunohistochemistry, the final concentrations of the primary antibodies were diluted as follows: CD43 for polymorphonuclear (PN) cells (1:200), GFAP for astrogliosis (1:300), MBP (1:100), neurofilament (NF, 1:100), and O4 (10 μg/mL, over night at 4°C). For free-floating section immunostaining, the primary antibodies against NG2, O4 or O1 were used at a dilution of 1 μg/mL. After being incubated with biotinylated second antibodies for 1 h at RT, brain sections were further incubated with FITC- or Cy3-conjugated avidin or the avidin-horseradish peroxidase system (ABC kit from Vector Laboratories, Burlingame, CA, U.S.A.) for an additional 1 h in dark at RT. In free-floating section immunostaining, DAPI (100 ng/mL) was simultaneously used to identify nuclei in the final visualization. Sections incubated in the absence of primary antibody were used as negative controls. Microglia were detected using lectin histochemistry. Biotinylated tomato lectin was used at a concentration of 10 μg/mL and the results were visualized using the Vector ABC system.
To compare the inflammatory responses and brain injury markers among the treatment groups, positively stained cells were counted. For cell counting, a digital microscopic image for each brain section was captured at the area where the positive cells were most abundant. Cell number in each image was counted and the average of the three sections from each brain was taken. When the cellular boundary was not clearly separated (such as some O4 or O1 positive cells), numbers of DAPI-stained nuclei from the superimposed images were counted as the cell number. The size of the image measured by the National Institutes of Health software was 0.3 mm2. The results were expressed as the average number of cells per image.
TUNEL staining and double labeling.
Apoptosis was detected using terminal deoxynucleotidyl transferase-mediated uridine 5′-triphosphate-biotin nick end labeling (TUNEL) kits and double labeling techniques were used to identify the cell type of the TUNEL positive cells. For TUNEL staining, the manufacturer's instructions were followed. Following incubation with terminal deoxynucleotidyl transferase for 1 h at 37°C, the sections were incubated with the primary antibody for specific cell markers or with biotinylated lectin for 2 h at RT (GFAP, CD43, NF) or overnight at 4°C (O4). After washing, the sections were incubated with biotinylated donkey anti-rabbit or anti-mouse antibody (depending on the primary antibody) at a dilution of 1: 200 for 1 h at RT. When TUNEL staining was performed in combination with biotinylated lectin, the step of incubation with a secondary antibody was omitted. The sections were then incubated with a mixture of the fluorescein-labeled anti-digoxigenin conjugate and Cy3-labeled avidin (1:200) for 0.5 h at RT in dark. After washing and mounting, the results were examined under a fluorescence microscope using appropriate excitation and emission filters. The TUNEL positive cells show green color and the Cy3 stained cells show bright orange color.
Caspase-3 activity.
Elevation in caspase-3 activity is an early marker of apoptosis. Caspase-3 activity in the rat brain was determined 24 h after injection with IL-1βor TNFα by an assay kit, following manufacturer's instruction. Briefly, the ipsilateral forebrain was weighed and homogenized in 4× volume of lysis buffer (wt/vol), and the homogenate was kept on ice for 10 min. After centrifugation at 12,000 × g for 10 min at 4°C, caspase-3 activity in the supernatant was determined colorimetrically with a microplate reader (Bio-Tek, Winooski, VT, U.S.A.) at 405 nm. Caspase-3 activity in the naïve rat pup brain was determined as the baseline level. Caspase-3 activity in the rat brain from other groups was expressed as a percentage of the baseline level.
Statistics.
Data of cell counting and caspase-3 activity were presented as the means ± SEM. The cell counting and caspase-3 data were analyzed by one-way ANOVA followed by Student-Newman-Keuls test. Results with a p <0.05 were considered statistically significant.
RESULTS
Inflammatory responses and bleeding in the brain.
Intra-cerebral injection of IL-1βor TNFα induced inflammatory responses in the rat brain, as indicated by increases in the number of CD43 positive PN cells and activated microglia. CD43 positive PN cells were rarely seen in the naïve and the saline-injected P6 or P8 (24 h or 3 d after the intracerebral injection) rat brain. Widely distributed CD43 positive PN cells (Fig. 1A insert) were observed in the frontal cortex, the corpus callosum and the subventricular area in both hemispheres 24 h after IL-1β or TNFα administration. The number of CD43 positive PN cells in the IL-1β-injected rat brain was similar to that in the TNFα -injected rat brain (44.5 ± 4.1 versus 37.8 ± 8.1 in the subventricular area, for example). By P8, the number of CD43 positive cells was reduced in both groups. As shown in Fig. 1A and B, however, the IL-1β -injected rat brain had more CD43 positive cells in the subventricular area compared with the TNFα -injected rat brain (21.8 ± 1.1 versus 2.8 ± 1.1 for left brain and 16.8 ± 3.6 versus 2.6 ± 1.0 for right brain, p <0.01).
Inflammatory responses and hemorrhage in the neonatal rat brain following the intracerebral injection of IL-1βor TNFα. Intracerebral injection was performed in 18 P5 rat brains (saline, 4; IL-1β, 7 and TNFα, 7). CD43 positive polymorphonuclear (PN) cells, as indicated by white arrows, were greatly induced following injection of IL-1β (A), and, to a less extent, of TNFα (B). The insert in A is the magnified part of the white box. Microglia at resting status (C, arrows indicated) were seen in the control rat brain. Activated microglia (arrowheads indicated) were found in IL-1β(D) and TNFαE) treated rat brain. In H&E stained brain sections, hemorrhage was seen at the injection site in the control (F), and IL-1βor TNFα (H) treated rat brains. Hemorrhage was also seen at the contralateral side of rat brain treated with IL-1βor TNFα(I, indicated by arrows), but not of the control rat brain (G). Magnification: 100×. Scale bar in G, 100 μm.
Microglia were widely distributed in the whole brain of the control and the naïve rats, and almost all the microglia were in the resting status (Fig. 1C). Injection of IL-1β greatly stimulated activation of microglia 24 h after the injection, especially at the frontal cortex and the subventricular area (Fig. 1D). Compared with IL-1β, TNFα stimulated less microglia activation (Fig. 1E). The number of activated microglia stimulated by IL-1βand by TNFα in the subventricular area was 38.2 ± 3.3 versus 15.2 ± 2.0, respectively (p < 0.01). Although activated microglia stimulated by IL-1β in the frontal cortex area were also more than that stimulated by TNFα, the difference was not of statistical significance (34.4 ± 3.1 versus 24.6 ± 4.1). By P8, activated microglia were rarely observed in the rat brain regardless of treatments.
H&E staining showed that intracerebral injection with saline caused slight bleeding at the site of injection, as indicated by accumulation of red blood cells (Fig. 1F), but not at the contralateral side (Fig. 1G). Injection with IL-1βor TNFα not only caused more severe hemorrhage at the site of injection (Fig. 1H), but also caused bleeding at the contralateral corpus callosum and the frontal cortex 24 h after the injection (Fig. 1I). No other apparent histopathological changes were observed. By P8, accumulated red blood cells were not observed in either side of the brain in all treatment groups.
Astrogliosis.
GFAP positive staining was observable at the corpus callosum area and the subcortical white matter tract in the control and the naïve P6 rat brain, but was never seen in the cortex (Fig. 2A), except at the needle path of some saline injected rat brains. IL-1β greatly increased GFAP positive cells at the frontal and the parietal cortex of the P6 rat brain (Fig. 2B), suggesting active astrogliosis. Similarly increased GFAP positive staining at the frontal and the parietal cortex in the TNFα -injected rat brain was also observed 24 h after the injection (Fig. 2C). The increased GFAP positive staining was also observed in the P8 IL-1βor TNFα-injected rat brain (data not shown).
Representative GFAP immunostaining in the rat brain 24 h after intracerebral injection of IL-1β or TNFα. The number of brains examined was the same as that in Fig. 1. Greatly increased GFAP positive cells at the frontal and the parietal cortex were observed in the IL-1β (B) or TNFα (C) treated rat brain, but not in the control rat brain (A). Magnification: 100× Scale bar in A, 100 μm.
IL-1β increased TUNEL staining and Caspase-3 activity.
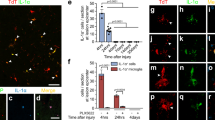
TUNEL positive staining was rarely seen in the control rat brain (Fig. 3A). Injection of IL-1β significantly increased the number of TUNEL positive cells in the rat brain 24 h after the injection (Figs. 3B and 4A). TUNEL positive cells were primarily localized in the outer layers of the cortex and in the subventricular area of both hemispheres. Double labeling indicated that the TUNEL positive cells were microglia (Fig. 3D, mostly distributed in the outer layers of the cortex), O4 positive OLs (Fig. 3E, in the corpus callosum and the subventricular area) and a few neurons (Fig. 3F). Neither the astrocyte nor the PN cell was found to be TUNEL positive (data not shown). Although the number of TUNEL positive cells was also increased following TNFα injection, the increase was significantly less than that induced by IL-1β (Figs. 3C and 4A). The number of TUNEL positive cells in the subventricular area of the IL-1β-injected and the TNFα -injected rat brain was 14.4 ± 1.2 and 4.4 ± 1.1, respectively, whereas that number in the control rat brain was 1.6 ± 0.2. No TUNEL positive cells were observed in the P8 rat brain regardless of treatments.
TUNEL staining in the 6-d old rat brain and MBP immunostaining in the 8-d old rat brain. Intracerebral injection was performed in 36 P5 rat brains (control, 8; IL-1β, 14; and TNFα, 14). Increased number of TUNEL positive cells (green) was observed in the subventricular area of the rat brain treated with IL-1β (B) 24 h after the injection. To a less extent, TNFα also induced TUNEL positive cells (C), but no TUNEL positive cells were seen in the same area of the control rat brain (A). Double labeling showed that TUNEL positive cells were lectin positive microglia (D, arrows indicated), O4+ oligodendrocytes (E, arrows indicated), and a few neurofilament positive neurons (F). MBP positive staining (brown color) was observed at the corpus callosum area, the subcortical white matter and the internal capsule area in the P8 control rat brain injected with sterile saline (G). Injection with IL-1β almost completely suppressed MBP expression (H). Expression of MBP in the rat brain treated with TNFα was less affected (I). Magnification: 100×. Scale bar in G, 100 μm.
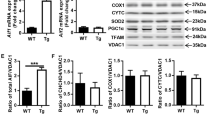
The number of TUNEL positive cells in the P6 rat brain (A) and the number of NG2+, O4+ and O1+ cells per 0.3 mm2 in the P6 (B) and P8 (C) rat brain. TUNEL staining, immunostaining of developing OLs, and quantification of positively stained cells were performed in free-floating brain sections prepared as described in methods. Intracerebral injection was performed in 32 P5 rat brains (8 for each treatment group). (A) IL-1β significantly increased TUNEL positive cells and this increase could be partially blocked by systemic injection of NBQX. To a less extent, TNFα also caused an increase in TUNEL positive cells. **p < 0.05 from the value for all groups (n = 4 for each group). *p < 0.05 from the value for the control group. (B) Intracerebral injection of IL-1β or TNFα did not significantly alter NG2+ cell number. IL-1β, but not TNFα, significantly reduced O4+ and O1+ OLs 24 h after the injection. NBQX was unable to prevent the reduction in O4+ and O1+ cell numbers. *p < 0.05 from the value for the IL-1β or the IL-1β+NBQX groups (n = 4 for each group). © By P8, numbers of NG2+ and O4+ cells were not different among groups. Number of O1+ cells in the rat brain treated with IL-1β was significantly lower than that in the control rat brain. *p < 0.05 from the value for the control group (n = 4 for each group).
Consistent with the TUNEL staining data, caspase-3 activity in the rat brain injected with IL-1β was significantly higher than that in the saline-injected or TNFα -injected rat brain 24 h after the injection, suggesting that apoptotic cell death may occur following IL-1β administration (Fig. 5). The elevation of caspase-3 activity over that in the naïve rat brain was 107.7 ± 9.3%, 147.9 ± 2.0%, and 114.6 ± 4.9% for the control, the IL-1β-injected and the TNFα -injected groups, respectively.
Caspase-3 activity in the rat brain 24 h after the intracerebral injection of IL-1β or TNFα. The control rats were injected with sterile saline containing 0.1% BSA. Caspase-3 activity in the ipsilateral forebrain was determined as described in methods. The baseline level of caspase-3 activity was determined in 3 naïve rat brains. Data are presented as the Mean ± SEM of samples for each treatment (n = 4). *p < 0.05 from the value for the other groups.
IL-1β reduced MBP staining.
MBP positive staining was clearly detected in the P8 control rat brain, primarily at the subcortical white matter tract, the internal capsule and the corpus callosum areas (Fig. 3G). A grade system was used to score the intensity of MBP positive staining. The score was defined as the following: mild, 1; moderate, 2; strong, 3; and no immunoreactivity, 0. Digital microscopic images were taken at the above-mentioned three areas for each brain section. The average of the three scores was used to represent the grade of MBP staining for each brain. The MBP staining grade in the control, the IL-1β-injected and the TNFα -injected rat brain was 2.1 ± 0.2, 0.3 ± 0.2, and 1.8 ± 0.3, respectively. Intracerebral injection of IL-1β significantly suppressed expression of MBP and almost no positive or very weak positive MBP staining, if any, was detected in the P8 IL-1β-injected rat brain (Fig. 3H). Expression of MBP in the rat brain injected with TNFα was less affected (Fig. 3I) and MBP staining score in the TNFα -injected rat brain was not significantly different from that in the control rat brain.
NBQX attenuated IL-1β-induced apoptosis, but failed to reduce IL-1β-induced injury to developing OLs.
MBP is produced by OLs. It is possible that the suppressed expression of MBP following IL-1βinjection is an indication of injury to OL development. The sequence of OL development is thought to begin with NG2+/O4− early OL progenitor cells, and to progress to O4+/O1− late OL progenitor cells, O4+/O1+ immature OLs, and mature OLs that express MBP (33). We used antibodies against NG2, O4 or O1 to examine effects of IL-1βon OL development. Furthermore, in vitro experiments have shown that IL-1βpromotes OL death through glutamate excitotoxicity and NBQX, an antagonist of the AMPA glutamate receptor, blocks OL apoptotic cell death induced by IL-1β in mixed glial cultures (23). To examine whether the effect of IL-1βon developing OLs is also mediated by the glutamate receptor, NBQX was administered following IL-1β injection. As shown in Fig. 4A, NBQX partially, but signifi-cantly, reduced the number of TUNEL positive cells induced by IL-1β. It is an indication that the apoptotic cell death following IL-1β administration in the present study is at least partially associated with glutamate excitotoxicity. However, NBQX did not prevent the IL-1β -induced injury to developing OLs (Figs. 4B, C and 6). Neither IL-1β nor TNFα significantly altered density of NG2 positive cells, which were widely distributed in the whole brain section (Figs. 4B, C). O4 positive cells were largely distributed in the corpus callosum and subcortical white matter tract, and a few of them were distributed in the subventricular area. The O1 positive cells had a similar distribution as the O4+ cells did, except that the distribution of O1+ cells in the subventricular area was denser. IL-1β, but not TNFα, significantly reduced the density of O4+or O1+cells 24 h after tahe injection (Figs. 4B and 6). NBQX was unable to prevent the reduction of O4+ or O1+cells caused by IL-1β. By P8, the density of O1+ cells at the corpus callosum area in the IL-1β treated rat brain was still significantly lower than that in the control group, although the density of O4+ OLs was not significantly different among groups.
Representative immunostaining of O4+ cells 24 h after the intracerebral injection. The injection was performed in 16 P5 rat brains as described in methods (4 for each treatment group) and immunostaining was performed in free-floating brain sections. Strong O4+ staining was observed in the corpus callosum and subcortical white matter tract of the control rat brain (A and E) and the rat brain injected with TNFα (D and H). IL-1β injection greatly suppressed O4+ staining (B and F) and systemic treatment with NBQX was unable to prevent the loss of O4+ staining (C and G). Magnification:A–D, 25× E–H, 100×. Scale bar in A, 300 μm; Scale bar in E, 100 μm.
DISCUSSION
IL-1β, when administered alone, has been reported to be nontoxic in many in vivo studies (19,27,35) and only few studies have shown that IL-1β alone may induce apoptosis in the adult rat brain (22). Results from the current study provide supporting evidence that IL-1β may also induce apoptotic cell death in the neonatal rat brain. Furthermore, data from the current study show for the first time that IL-1β directly causes injury to developing OLs in the neonatal rat brain. Recent studies have shown that late OL progenitor cells (O4+ /O1−) are selectively vulnerable to hypoxicischemic injury and coincide with the developmental window for vulnerability for human perinatal white matter injury (33,36). Consistently, our results indicate that IL-1βselectively causes injury to O4+ OLs and to a less extent, to O1+ OLs (Figs. 4B, C and 6). Our data support the hypothesis that the increased IL-1β concentrations (6,7,11) derived from maternal infection may contribute to the occurrence of PVL in the infant brain.
Infiltrated leukocytes and activated microglia have been proposed to contribute to white matter damage induced by hypoxiaischemia or inflammation/infection in extremely low gestational age newborns (37,38). This hypothesis is supported by our observation that more severe brain injury in the IL-1β-injected rat brain compared with that in the TNFα -injected rat brain was associated with the higher increase in the number of activated microglia and CD43+ PN cells in the neonatal rat brain following intracerebral injection of IL-1β Our data further indicate that the more severe brain injury in the IL-1β-injected rat brain was linked with the more sustained elevation of the number of CD43+ PN cells in the IL-1β-injected rat brain. This is an indication that sustained activation of leukocytes may lead to more damage than a short-lived inflammatory cytokine cascade (37). The increased number of CD43+ PN cells suggests that IL-1β and TNFα may cause injuries to the endothelia of blood vessels and the blood-brain barrier, and facilitate the process of transendothelial migration of the activated leukocytes from the circulation to the brain. Results from the current study did not reveal the detailed role of the increased PN cells and activated microglia in the injury to OLs. Although investigation of the role of activated leukocytes and microglia in white matter damage is beyond the scope of the current study, this is certainly a very important area in future investigations for the mechanisms involved in PVL-like white matter damage.
IL-1β induces apoptotic OL cell death in a mixed glial culture, but not in pure OL cultures, and its effect could be blocked by NBQX or CNQX, antagonists of the AMPA glutamate receptor (23). It is thought that IL-1β is not directly cytotoxic to OLs and that its effect on OLs is through the impairment of the glutamate transporter expression or glutamate-uptaking capacity of astrocytes (23,39,40). In the current study, NBQX also attenuated apoptotic cell (including OL, Fig. 3E) death (Fig. 4A), suggesting that glutamate excitotoxicity is involved in the mechanism underlying apoptotic cell death induced by IL-1β. However, results from the current study are not sufficient to support the possibility that apoptotic cell death observed in the present study is due to the blockade of glutamate uptake by astrocytes following IL-1βadministration. Although astrogliosis stimulated by IL-1β (Fig. 2) might be an indication of injuries to astrocytes, similar astrogliosis was also observed following injection of TNFα, which induced much less apoptotic cell death (Fig. 4A). Therefore, astrogliosis observed in the present study is rather an indication of the general response to the injury or an indication of trophic effects of IL-1βor TNFα on astrocytes (41).
HI-induced OL injury has been shown to be attenuated by AMPA receptor antagonist NBQX (34), whereas injuries to developing OLs induced by IL-1β in the present study were not affected by NBQX (Figs. 4 and 6), suggesting that the mechanism involved in the IL-1β-induced injury to developing OLs may be different from that underlying OL injury caused by perinatal HI. Double labeling has shown that IL-1β-induced apoptotic cell death includes developing OLs, and therefore, apoptosis may partially explain the reduction in O4+ and O1+ immunoreactivity one day after IL-1β injection. However, apoptotic cell death was observed primarily in the subventricular area, while loss of O4+ and O1+ immunoreactivity was largely seen in the corpus callosum and the subcortical white matter tract in the current study. Furthermore, the number of TUNEL positive cells was not comparable to the reduction in number of O4+ and O1+ OLs (Figs. 4A, B). In addition, NBQX reduced number of TUNEL positive cells, while it failed to prevent the loss of immunoreactivity of developing OLs. In the present study, it is unlikely that apoptosis is the major cause for the loss of O4+and O1+ OL immunoreactivity following IL-1βadministration. Significant loss of O4+ and O1+ OL immunoreactivity was observed one day after IL-1βinjection in the current study. By P8, O4+ cell density in the IL-1β-treated rat brain was not significantly different from that in the control rat brain (Fig. 4C). Because the loss of O4+ cells was observed following a single injection of IL-1β, it is reasonable to speculate that prolonged exposure of OLs to IL-1βmight result in more losses of OLs. Alternatively, this could be a reflection of either functional recovery of the injured OLs or a compensatory proliferation or maturation of NG2+ OLs to O4+ OLs. The significantly reduced O1+ OLs in the P8 IL-1β -treated rat brain could result from the lower number of O4+ OLs for differentiation in the P6 rat brain. Functional recovery of injured OL proliferation and maturation of OL progenitors as indicated by restoration of the lost MBP staining in the neonatal rat brain has been reported after moderate, but not after more severe, cerebral hypoxiaischemia (42). Since no necrotic or dead cells were found in the H&E stained sections from either the P6 or the P8 rat brain, it is likely that IL-1β did not kill OLs, but instead impaired OL function or delayed OL development and differentiation. The present data have not provided direct evidence for this possibility and further investigation is needed.
TNFα has been reported to induce damage of the blood-brain barrier in vivo (41) and cause death of OLs in vitro (25,26). In the present study, TNFα did not cause major injury to OLs compared with IL-1β and induced far less severe apoptosis compared with that in the IL-1β-treated rat brain, although it stimulated similar astrogliosis (Fig. 2) and hemorrhage as that by IL-1β (Fig. 1). The lack of effects of TNFα on OL injury observed in this study suggests that TNFα and IL-1β may play different roles in mediating brain white matter injury. Enhanced TNFα expression induced by LPS has been found not to trigger apoptosis in glial cells, both in vivo and in vitro (43). Failure of TNFα, at doses either lower or higher than that used in the present study, in stimulation of apoptotic cell death has also been reported in adult rat brains by other investigators (22). These authors find that intracerebral injection of IL-1β stimulates expression of the proapoptotic factor Bax and the antiapoptotic factor Bcl-2 and that IL-1β stimulated apoptosis is associated with the presence of more Bax expressing cells than Bcl-2 expressing cells (22). They also find IL-1β-induced apoptotic cell death is closely associated with the extent of inflammatory responses. In our ongoing studies, we find that while the number of Bcl-2 expressing cells is similar in the IL-1β-treated and the TNFα-treated rat brains, the number of Bax expressing cells in the IL-1β-treated rat brain is significantly more than that in the TNFα-treated rat brain (data not shown). It is possible that the difference between IL-1βand TNFα in induction of apoptotic cell death is associated with differential expression of Bax and Bcl-2 stimulated by them. In addition, the density of the activated microglia stimulated by TNFα was significantly less than that stimulated by IL-1β in the present study. More activated microglia in IL-1β-treated brain may contribute to more apoptosis in these rat brains compared with in the TNFα -treated rat brain, although the detailed mechanisms remain to be elucidated. We found in our previous study that application of TNFα antibody was unable to protect LPS-induced OL injury, while an IL-1 receptor antagonist blocked LPS-induced brain injury, suggesting that increased TNFα may not have a direct causal-effect in LPS-induced brain injury (32). The lack of effect of TNFα on developing OLs observed in the current study is consistent with our previous results. Data from both studies indicate that TNFα might not cause severe brain injury in an in vivo setting of experimental conditions like the present study. However, it is premature to exclude TNFα from the list of factors mediating infection and/or inflammation-induced neonatal white matter injury. Our studies primarily look at acute effects. Recent studies have shown that TNFα pro-tective IGF-1 (IGF-1) signaling pathway (44,45). IGF plays important roles in regulation of OL survival and development (46). TNFα may cause injuries to OLs and white matter through its interference with the IGF system and this possibility is worth further investigation.
In summary, intracerebral injection of IL-1β, but not TNFα, can cause apoptotic cell death and impairment of developing OLs. The AMPA receptor antagonist, NBQX can partially attenuate IL-1β induced apoptotic cell death, but is unable to prevent its deteriorative effect on developing OLs. IL-1β may contribute significantly to white matter injury in the neonatal brain.
Abbreviations
- IL-1β:
-
interleukin-1beta
- TNFα:
-
tumor necrosis factor-alpha
- PVL:
-
periventricular leukomalacia
- LPS:
-
lipopolysaccharide
- HI:
-
hypoxiaischemia
- OL:
-
oligodendrocyte
- NF:
-
neurofilament
- GFAP:
-
glial fibrillary acidic protein
- MBP:
-
myelin basic protein
- NBQX:
-
6-nitro-7-sulfamoylbenzoquinoxaline-2,3-dione
- PN:
-
polymorphonuclear
- TUNEL:
-
terminal deoxynucleotidyl transferase-mediated uridine 5′-triphosphate-biotin nick end labeling
References
Dammann O, Leviton A 1997 Maternal intrauterine infection, cytokines, and brain damage in the preterm newborn. Pediatr Res 42: 1–8.
Dammann O, Leviton A 1998 Infection remote from the brain, neonatal white matter damage, and cerebral palsy in the preterm infant. Semin Pediatr Neurol 5: 190–201.
Volpe JJ 1997 Brain injury in the premature infant. Neuropathology, clinical aspects, pathogenesis, and prevention. Clin Perinatal 24: 567–587.
Volpe JJ 2001 Neurology of the Newborn. 4th Edition. WB Saunders Co, Philadelphia, 231–276.
Leviton A 1993 Preterm birth and cerebral palsy: is tumor necrosis factor the missing link Dev?. Med Child Neurol 35: 553–558.
Deguchi K, Mizuguchi M, Takashima S 1996 Immunohistochemical expression of tumor necrosis factor alpha in neonatal leukomalacia. Pediatr Neurol 14: 13–16.
Deguchi K, Oguchi K, Takashima S 1997 Characteristic neuropathology of leukomalacia in extremely low birth weight infants. Pediatr Neurol 16: 296–300.
Kadhim H, Tabarki B, Verellen G, De Prez C, Rona AM, Sebire G 2001 Inflammatory cytokines in the pathogenesis of periventricular leukomalacia. Neurology 56: 1278–1284.
Yoon BH, Romero R, Kim CJ, Koo JN, Choe G, Syn HC, Chi JG 1997 High expression of tumor necrosis factor-α and interleukin-6 in periventricular leukomalacia. Am J Obstet Gynecol 177: 406–411.
Yoon BH, Romero R, Yang SH, Jun JK, Kim IO, Choi JH, Syn HC 1996 Interleukin-6 concentrations in umbilical cord plasma are elevated in neonates with white matter lesions associated with periventricular leukomalacia. Am J Obstet Gynecol 174: 1433–1440.
Yoon BH, Jun JK, Romero R, Park KH, Gomez R, Choi JH, Kim IO 1997 Amniotic fluid inflammatory cytokines (interleukin-6, interleukin-1β, and tumor necrosis factor-α), neonatal brain white matter lesions, and cerebral palsy. Am J Obstet Gynecol 177: 19–26.
Duncan JR, Cock ML, Scheerlinck JP, Westcott KT, McLean C, Harding R, Rees SM 2002 White matter injury after repeated endotoxin exposure in the preterm ovine fetus. Pediatr Res 52: 941–949.
Mallard C, Welin AK, Peebles D, Hagberg H, Kjellmer I 2003 White matter injury following systemic endotoxemia or asphyxia in the fetal sheep. Neurochem Res 28: 215–223.
Bell MJ, Hallenbeck JM 2002 Effects of intrauterine inflammation on developing rat brain. J Neurosci Res 70: 570–579.
Cai Z, Pan ZL, Pang Y, Evans OB, Rhodes PG 2000 Cytokine induction in fetal rat brain and brain injury in neonatal rats after maternal lipopolysaccharide administration. Pediatr Res 47: 64–72.
Barone FC, Arvin B, White RF, Miller A, Webb CL, Willette RN, Lysko PG, Feuerstein GZ 1997 Tumor necrosis factor-alpha. A mediator of focal ischemic brain injury. Stroke 28: 1233–1244.
Hagberg H, Gilland E, Bona E, Hanson LA, Hahin-Zoric M, Blennow M, Holst M, McRae A, Soder O 1996 Enhanced expression of interleukin (IL)-1 and IL-6 messenger RNA and bioactive protein after hypoxiaischemia in neonatal rats. Pediatr Res 40: 603–609.
Hara H, Friedlander RM, Gagliardini V, Ayata C, Fink K, Huang Z, Shimizu-Sasamata M, Yuan J, Moskowitz MA 1997 Inhibition of interleukin 1beta converting enzyme family proteases reduces ischemic and excitotoxic neuronal damage. Proc Natl Acad Sci U.S.A. 94: 2007–2012.
Loddick SA, Rothwell NJ 1996 Neuroprotective effects of human recombinant interleukin-1 receptor antagonist in focal cerebral ischaemia in the rat. J Cereb Blood Flow Metab 16: 932–940.
Nawashiro H, Martin D, Hallenbeck JM 1997 Neuroprotective effects of TNF binding protein in focal cerebral ischemia. Brain Res 778: 265–271.
Relton JK, Martin D, Thompson RC, Russell DA 1996 Peripheral administration of Interleukin-1 receptor antagonist inhibits brain damage after focal cerebral ischemia in the rat. Exp Neurol 138: 206–217.
Holmin S, Mathiesen T 2000 Intracerebral administration of interleukin-1β and induction of inflammation, apoptosis, and vasogenic edema. J Neurosurg 92: 108–120.
Takahashi JL, Giuliani F, Power C, Imai Y, Yong VW 2003 Interleukin-1β promotes oligodendrocyte death through glutamate excitotoxicity. Ann Neurol 53: 588–595.
Megyeri P, Abraham CS, Temesvari P, Kovacs J, Vas T, Speer CP 1992 Recombinant human tumor necrosis factor-alpha constricts pial arterioles and increases blood-brain barrier permeability in newborn piglets. Neurosci Lett 148: 137–140.
Selmaj KW, Raine CS 1988 Tumor necrosis factor mediates myelin and oligodendrocytes damage in vitro. Ann Neurol 23: 339–346.
Selmaj K, Raine CS, Farooq M, Norton WT, Brosnan CF 1991 Cytokine cytotoxicity against oligodendrocytes. Apoptosis induced by lymphotoxin. J Immunol 147: 1522–1529.
Allen SM 2002 Varied actions of proinflammatory cytokines on excitotoxic cell death in the rat central nervous system. J Neurosci Res 67: 428–434.
Liu XH, Xu H, Barks JD 1999 Tumor necrosis factor-α attenuates N-methyl-D-aspartate-mediated neurotoxicity in neonatal rat hippocampus. Brain Res 851: 94–104.
Arnett HA, Mason J, Marino M, Suzuki K, Matsushima GK, Ting JP 2001 TNF-alpha promotes proliferation of oligodendrocyte progenitors and remyelination. Nat Neurosci 4: 1116–1122.
Barger SW, Horster D, Furukawa K, Goodman Y, Krieglstein J, Mattson MP 1995 Tumor necrosis factor alpha and beta protect neurons against amyloid beta-peptide toxicity: Evidence for involvement of kappa-B-binding factor and attenuation of peroxide and Ca2+ accumulation. Proc Natl Acad Sci U.S.A. 92: 9328–9332.
Pang Y, Cai Z, Rhodes PG 2003 Disturbance of oligodendrocyte development, hypomyelination and white matter injury in the neonatal rat brain after intracerebral injection of lipopolysaccharide. Brain Res Dev Brain Res 140: 205–214.
Cai Z, Pang Y, Lin S, Rhodes PG 2003 Differential roles of tumor necrosis factor-alpha and interleukin-1beta in lipopolysaccharide-induced brain injury in the neonatal rat. Brain Res 975: 37–47.
Back SA, Han BH, Luo NL, Chricton CA, Xanthoudakis S, Tam J, Arvin KL, Holtzman DM 2002 Selective vulnerability of late oligodendrocyte progenitors to hypoxiaischemia. J Neurosci 22: 455–463.
Follett PL, Rosenberg PA, Volpe JJ, Jensen FE 2000 NBQX attenuates excitotoxic injury in developing white matter. J Neurosci 20: 9235–9241.
Patel HC, Boutin H, Allan SM 2003 Interleukin-1 in the brain: mechanisms of action in acute neurodegeneration. Ann NY Acad Sci 992: 39–47.
Back SA, Luo NL, Borenstein NS, Levine JM, Volpe JJ, Kinney HC 2001 Late oligodendrocyte progenitors coincide with the developmental window of vulnerability for human perinatal white matter injury. J Neurosci 21: 1302–1312.
Dammann O, Durum S, Levition A 2001 Do white cells matter in white matter damage?. Trends Neurosci 24: 320–324.
Stoll G, Jander S 1999 The role of microglia and macrophages in the pathophysiology of the CNS. Prog Neurobiol 58: 233–247.
Hu S, Sheng WS, Ehrlich LC, Peterson PK, Chao CC 2000 Cytokine effects on glutamate uptake by human astrocytes. Neuroimmunomodulation 7: 153–159.
Ye ZC, Sontheimer H 1996 Cytokine modulation of glial glutamate uptake: a possible involvement of nitric oxide. Neuroreport 7: 2181–2185.
Merrill JE 1991 Effects of interleukin-1 and tumor necrosis factor-alpha on astrocytes, microglia, oligodendrocytes, and glial precursors in vitro. Dev Neurosci 13: 130–137.
Liu Y, Silverstein FS, Skoff R, Barks JD 2002 Hypoxic-ischemic oligodendroglial injury in neonatal rat brain. Pediatr Res 51: 25–33.
Cheng YJ, Yang BC, Hsieh WC, Huang BM, Liu MY 2002 Enhancement of TNF-alpha expression does not trigger apoptosis upon exposure of glial cells to lead and lipopolysaccharide. Toxicology 178: 183–191.
Venters HD, Dantzer R, Kelley KW 2000 A new concept in neurodegeneration: TNF-alpha is a silencer of survival signals. Trends Neurosci 23: 173–180.
Venters HD, Tang Q, Liu Q, VanHoy RW, Dantzer R, Kelley KW 1999 A new mechanism of neurodegeneration: a proinflammatory cytokine inhibits receptor signaling by a survival peptide. Proc Natl Acad Sci U.S.A. 96: 9879–9884.
Orentas DM, Miller RH 1998 Regulation of oligodendrocyte development. Mol Neurobiol 18: 247–259.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by HD 35496.
Rights and permissions
About this article
Cite this article
Cai, Z., Lin, S., Pang, Y. et al. Brain Injury Induced by Intracerebral Injection of Interleukin-1beta and Tumor Necrosis Factor-alpha in the Neonatal Rat. Pediatr Res 56, 377–384 (2004). https://doi.org/10.1203/01.PDR.0000134249.92944.14
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000134249.92944.14
This article is cited by
-
Caught in vicious circles: a perspective on dynamic feed-forward loops driving oxidative stress in schizophrenia
Molecular Psychiatry (2022)
-
Neuroprotective effect of liraglutide in an experimental mouse model of multiple sclerosis: role of AMPK/SIRT1 signaling and NLRP3 inflammasome
Inflammopharmacology (2022)
-
Downregulation of phosphoglycerate mutase 5 improves microglial inflammasome activation after traumatic brain injury
Cell Death Discovery (2021)
-
Maternal Progesterone Treatment Reduces Maternal Inflammation-Induced Fetal Brain Injury in a Mouse Model of Preterm Birth
Reproductive Sciences (2021)
-
Sex-specific maternofetal innate immune responses triggered by group B Streptococci
Scientific Reports (2019)