Abstract
Among pathologies prevalent in western societies, anorexia nervosa has increased over the last decade. Its effects on bone mass need to be defined, and prognostic factors, either clinical or biochemical, could aid clinicians in individual patient management. To determine which clinical and/or biochemical parameters could be related to bone mass status in adolescent female anorexia nervosa patients, 73 female patients were classified according to different stages of their illness and studied in terms of clinical and biochemical parameters and bone densitometric mineral content at lumbar spine. Patients (age 17.2 ± 1.7 y, mean ± SD) with Tanner pubertal stage 5, regular menstruation for more than 3 mo before the onset of secondary amenorrhea, and diagnosed with anorexia nervosa were consecutively studied and classified in three clinical situations:I) active phase (34 patients): undernourished and amenorrheic;II) weight recovered but still amenorrheic (20 patients);III) fully recovered (19 patients). Clinical data were recorded at the time of bone density measurement, concomitant with blood sample extraction for study of IGF-I, IGF-binding protein 3 (IGFBP-3), IGFBP-1, estradiol, sex hormone-binding globulin, dehydroepiandrosterone sulfate, prealbumin, amino-terminal propeptide of procollagen III, osteocalcin, bone alkaline phosphatase, carboxy-terminal propeptide of procollagen I, amino-terminal propeptide of procollagen I, carboxy-terminal telopeptide of collagen I, 25-OH-vitamin D, 1,25(OH)2-vitamin D, and parathormone. In addition, a 24-h urine collection was made for cortisol, GH, deoxypyridinoline, amino-terminal telopeptide of collagen I, and calcium and creatinine content analysis. IGF-I, estradiol, and biochemical bone formation markers were higher and IGFBP-1, sex hormone-binding globulin, and biochemical bone resorption markers were lower in the weight-recovered stages (stages II and III) compared with the active phase (stage I). Bone formation markers correlated positively with body mass index SD score and IGF-I, whereas bone resorption markers correlated negatively with body mass index SD score and estradiol. Although no statistically significant differences regarding lumbar spine bone mineral density SD score values were recorded among the three stages of the illness, the proportion of osteopenic patients was clearly lower among stage III patients. The actual bone mineral density was inversely related to the duration of amenorrhea and directly related to duration of postmenarcheal menses before amenorrhea. In addition, a subset of osteopenic patients (five of 19) in the fully clinically recovered group with accelerated bone turnover was identified. Normal circulating estrogen level exposure time predicts actual bone mineral density at lumbar spine in young adolescent anorexia nervosa patients. In addition to psychiatric and nutritional interventions, estrogen-deprivation periods must be shortened to less than 20 mo. Patients remaining osteopenic at full clinical recovery require additional follow-up studies.
Similar content being viewed by others
Main
Osteoporosis constitutes one of the major health problems to be prevented and treated when human longevity is analyzed in terms of costs and quality of life. Maximal peak bone mass is acquired in the early twenties in both sexes (1), after the end of the period of skeletal longitudinal growth. During infancy and puberty, acquisition of adequate bone mineralization requires normal nutrition and metabolic and endocrine functions and absence of chronic pathologies. Hormones and growth factors that play a major role in regulating bone metabolism include T3, sex steroids, vitamin D, PTH, and GH together with the IGF-IGFBP system, and an intricate local system of growth and transcription factors (2–7). In the critical stage of their illness, patients with AN develop a state of undernutrition accompanied by a constellation of metabolic and hormonal alterations, with the hypothalamo-pituitary-gonadal axis being one of the most severely affected (8, 9). Bone mineralization risks being altered in this situation as a consequence of low levels of nutrients, growth factors, and hormones (principally sex steroids). Several works studied the alterations of bone mineralization in such patients (10–21) and described diminished BMD that was correlated with the degree and duration of undernutrition, clinical and biochemical indexes of nu trition, and, in some of those studies, clinical and hormonal markers of endocrine disturbances. As this pathology in its initial stage and subsequent evolution occurs during one of the periods of higher bone mass acquisition (puberty and late adolescence) (1), we studied the clinical, hormonal, and bone metabolic characteristics at different stages of the illness in female adolescent patients. Our aim was to determine the clinical and biochemical data that, related to bone mass, may become indicators of subsequent risk for osteopenia/osteoporosis and require an additional specific therapy.
METHODS
Subjects.
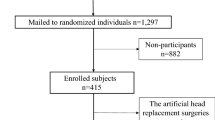
Seventy-three female patients with Tanner pubertal stage 5 (age 17.2 ± 1.7 y, mean ± SD, range 13.8–22.6 y) who menstruated regularly for more than 3 mo before the onset of secondary amenorrhea and who were diagnosed with AN according to DSM-IV criteria (22) were consecutively enrolled and classified in three clinical situations (Table 1):I) active phase (34 patients): undernourished and amenorrheic (defined as BMI lower than −1 SDS for age and amenorrhea for more than 3 mo);II) weight recovered but still amenorrheic (20 patients): BMI higher than −1 SDS but still amenorrheic after weight recovery;III) fully recovered (19 patients): BMI higher than −1 SDS with regular menses for more than 3 mo after weight recovery.
The present study was approved by the Ethics Committee of Hospitals Vall d'Hebron and informed consent from patients and/or parents was obtained.
Clinical studies.
Anthropometric (height, weight, BMI) and gynecologic data (age at menarche, age at onset of amenorrhea, months of amenorrhea, and months of regular menses after weight recovery) were recorded (Table 1). BMI was calculated as SDS for age and sex according to Hernández et al.(23).
Bone densitometry studies.
Bone densitometry was determined by DEXA with LUNAR DPX-L apparatus at lumbar spine L2–L4 and results expressed as SDS for age and sex according to reference data in our normal population (1).
Biochemical studies.
Baseline blood was drawn between 0800 and 0900 after an overnight fast. During the 24 h preceding the blood extraction, urine was collected at 4°C and protected from light; aliquots were frozen at −80°C protected from light for DPD and with BSA at 2 g/L for GH. Blood was extracted during the initial follicular phase of the menstrual cycle (d 2–5) for patients with regular menstruation. Blood samples were obtained consecutively throughout the year; the distribution between more and less sunny months was equally distributed in stage I and II patients (46% samples in autumn-winter and 54% samples in spring-summer for stage I and 50% autumn-winter and 50% spring-summer for stage II), whereas in stage III patients, autumn-winter samples predominated (62%).
Serum samples were analyzed for IGF-I, IGFBP-3, IGFBP-1, E2, SHBG, DHEA-S, prealbumin, PIIINP, OC, BAP, PICP, PINP, ICTP, 25-VitD, 1,25-VitD, and PTH concentrations. Cortisol, GH, DPD, NTx, calcium, and creatinine content were analyzed in the 24-h urine samples.
All assays were performed with commercially available kits. IGF-I and urinary GH were measured by RIA (Biomérieux, Marcy l'Etoile, France); IGFBP-3, 25-VitD, and 1,25-VitD by RIA (Nichols Institute Diagnostics, San Juan Capistrano, CA, U.S.A.); IGFBP-1 by ELISA (Medix Biochemica Ab, Kaunianien, Finland); PIIINP, PICP, PINP, ICTP, and E2 by RIA (Orion Diagnostica, Espoo, Finland); SHBG and intact PTH by IRMA and DHEA-S and urinary cortisol by RIA (Diagnostic Products Corporation, Los Angeles, CA, U.S.A.); intact OC by IRMA (Immutopics Inc., San Clemente, CA, U.S.A.); BAP by IRMA (Hybritech, Liège, Belgium); DPD by ELISA (Metra Biosystems, Palo Alto, CA, U.S.A.); and NTx by ELISA (Ostex, Seattle, WA, U.S.A.).
Normal ranges for all assays were obtained in a group of healthy postpubertal females (age 18.2 ± 2.5 y, n = 30) at the initial follicular phase.
Statistical analysis.
Comparisons between means of anthropometric and biochemical data of the three stages were analyzed by ANOVA and differences considered significant at p < 0.05. χ2 analysis was performed for differences in BMD-SDS value (normal, osteopenic, and osteoporotic) distribution among the three stages. Correlations between clinical and biochemical data were analyzed by linear and multiple regression analysis and considered significant at p < 0.05. These analyses were performed with the Statview 4.5 version for Macintosh.
In addition, correlations between bone metabolism biochemical markers and clinical, biochemical, and hormonal data were analyzed after grouping the seven parameters (OC, BAP, PICP,PINP, ICTP, DPD, and NTx) into two nonintercorrelated indexes (matrix of factors), by using a principal compound analysis, the first being the index better summarizing the information contained in the initial seven variables and the second summarizing the information not explained by the first. The indexes were submitted to an orthogonal varimax rotation. The first index contained the formation markers (OC, BAP, PICP, and PINP) and accounted for 30.757% of variance and the second the resorption markers (ICTP, DPD, and NTx) accounting for 33.795% of variance. Linear and multiple regression analysis were performed between each matrix of factors and clinical, biochemical, and hormonal data. This analysis was performed with the statistical program SYSTAT.
RESULTS
Clinical data.
Patients in the three clinical stages (Table 1) presented no differences for age, height, age at menarche, and duration of menses before amenorrhea. Weight and BMI were significantly higher in stages II and III (p < 0.0001).
BMD data.
BMD showed no significant differences between the three clinical stages, but results expressed in SDS for age and sex showed that the means were below −1 SDS in stages I and II and above in stage III (Table 1). The trend toward higher BMD was demonstrated by a statistically significant different distribution of BMD-SDS values [normal (≥ −1 SDS), osteopenic (< −1 and ≥ −2.5 SDS), and osteoporotic (< −2.5 SDS) (χ2 test, p = 0.02)] among the three stages studied.
Hormonal data.
Patients in the active phase of the disease (stage I) presented mean serum IGF-I levels below the lower normal limit for age and sex and an extremely low serum level of E2 (Table 2). Weight recovery (stage II) was characterized by a significantly increased mean IGF-I and E2 (p < 0.005) and decreased SHBG (p < 0.05). Recovery of regular menses (stage III) was characterized by higher urinary GH excretion and serum IGFBP-3 (p < 0.05) and E2 (p < 0.005 versus stage II) levels and lower IGFBP-1 (p < 0.05 versus stage I) serum levels. No significant differences were observed for DHEA-S or urinary cortisol (only two patients, one in stage I and the other in stage II, presented moderately elevated urinary cortisol excretion) (data not shown).
Calcium metabolism data.
Calciuria was abnormally high in stage I and was significantly lower in stages II and III (p < 0.005 for calciuria and p < 0.05 and < 0.001 for uCa/Cr, respectively) (Table 3). Phosphate tubular resorption and mean serum PTH, 25-VitD, and 1,25-VitD were within normal limits in the three clinical stages, although significantly higher levels were observed for PTH (p < 0.05) in stage II versus stage I and for 1,25-VitD in stage III (p < 0.0005 versus stage I and p < 0.05 versus stage II). Abnormally low levels of 25-VitD were observed in 24.6% of patients (17.6% in stage I, 35% stage II, and 26.3% stage III). Only five patients presented 1,25-VitD levels slightly below the normal range (three in stage I, one in stage II, and one in stage III), and only one patient presented PTH levels slightly above the normal range, coinciding with diminished 25-VitD.
Biochemical bone metabolism markers.
Bone formation markers (OC, BAP, PICP, and PINP) presented normal mean serum levels in stage I but were significantly higher with weight recovery in stage II (p < 0.005 for OC and PICP and p < 0.0001 for BAP and PINP), with mean levels being higher than age and sex upper limits for BAP, PICP, and PINP (Table 4). Similar levels were sustained in stage III except for PICP, which was again significantly lower (p < 0.05).
Among the bone resorption markers studied (ICTP, DPD, and NTx), only ICTP presented significant differences among stages: a decrease was observed between stages I and II (p < 0.05) and II and III (p < 0.005), with mean levels being above the upper limit for age and sex at all stages.
Clinical and biochemical determinants of bone metabolism.
No significant correlation was observed between BMD-SDS values and any hormonal or biochemical data in the overall group of patients. In simple linear regression analysis, BMD-SDS correlated positively with height (r = 0.55;p < 0.001), weight (r = 0.32;p = 0.006), and duration of menses before amenorrhea (r = 0.31;p = 0.01) in all patients (Fig. 1B) and negatively with the duration of amenorrhea (r = −0.48;p < 0.0005) in amenorrheic patients (stages I and II) (Fig. 1A). When amenorrhea periods were longer than 20 mo, all patients except one had BMD values lower than −1 SDS; however, with amenorrhea periods under 20 mo, approximately 50% of patients presented BMD values in the osteopenic range and the rest were within normal limits (Fig. 1). In stage III patients, no correlation was observed between BMD-SDS and duration of regular menses or with duration of amenorrhea before recovery. Multiple regression analysis showed a significant correlation between BMD-SDS and BMI-SDS (b = 0.285;p = 0.002) and the duration of amenorrhea (b = −0.046;p < 0.001).
Bone formation markers (OC, BAP, PICP, PINP) as a matrix of factors correlated positively with IGF-I (r = 0.41;p = 0.001), BMI-SDS (r = 0.56;p < 0.001), and weight (r = 0.54;p < 0.001) in simple linear regression and with IGF-I (p = 0.01) and BMI-SDS (p < 0.0001) in multiple regression. Individually, the highest correlation with IGF-I was observed for PINP (r = 0.49;p < 0.0001), followed by BAP (r = 0.41;p = 0.0004) and OC (r = 0.27;p = 0.02), whereas no correlation was observed with PICP.
Bone resorption markers (ICTP, DPD, NTx) as a matrix of factors correlated negatively with E2 (r = −0.36;p = 0.004), BMI-SDS (r = −0.34;p = 0.007), and weight (r = −0.46;p < 0.001) in simple linear regression and with E2 (p = 0.05) in multiple regression. Individually, only ICTP correlated significantly and negatively with weight (r = −0.44;p < 0.0001), BMI (r = −0.43;p = 0.0001), and BMI-SDS (r = −0.28;p = 0.02) and positively with SHBG (r = 0.39;p = 0.0007).
Calciuria correlated negatively with weight (r = −0.31;p = 0.01), BMI-SDS (r = −0.30;p < 0.05), and E2 (r = −0.28;p < 0.05). 1,25-VitD correlated positively with weight (r = 0.35;p = 0.005), BMI-SDS (r = 0.36;p = 0.005), and E2 (r = 0.42;p < 0.0005).
Osteopenic patients in stage III.
Twenty-six percent of patients in stage III remained osteopenic (BMD-SDS < −1) (five of 19) and, with respect to nonosteopenic patients in this stage, presented no significant difference for any clinical data (age, BMI, evolution time, duration of amenorrhea, duration of menses, duration of menses before amenorrhea, age at menarche) except BMD-SDS (−1.73 ± 0.36 versus −0.45 ± 0.60;p < 0.005) (Table 5). Among the hormonal and biochemical data, the only significant differences between osteopenic and nonosteopenic patients were found for biochemical markers of bone metabolism, which indicated higher bone turnover as demonstrated by higher OC (9.2 ± 2.5 versus 4.8 ± 1.9 ng/mL;p < 0.005) and PINP (119.8 ± 20.0 versus 91.6 ± 20.8 ng/mL;p < 0.05) for bone formation and ICTP (7.7 ± 0.5 versus 5.9 ± 1.5 ng/mL;p < 0.05) for bone resorption.
DISCUSSION
Female patients with AN are at increased risk for osteoporosis because of the association of undernutrition with loss of ovarian sex steroid secretion. Several works have studied bone mineralization status in this pathology (10–21). We analyzed cross-sectionally the clinical and biochemical characteristics of adolescent female AN patients that may be related to bone metabolism in the three most characteristic stages of the illness (undernutrition and amenorrhea, renutrition and amenorrhea, and, finally, full recovery with normal weight and circulating female sex steroids) in an attempt to clarify which clinical and/or biochemical data may be related to or predict osteopenia.
In the stage of undernutrition and amenorrhea, patients presented low IGF-I and extremely low circulating E2. In this situation, biochemical markers of bone metabolism indicated a shift toward bone resorption because, with normal levels of bone formation markers (OC, BAP, PICP, and PINP), bone resorption markers were elevated (serum ICTP) or at the upper normal limit (urinary DPD and NTx). Furthermore, calciuria was abnormally elevated. On average, 60% of patients were osteopenic (BMD < −1 SDS), and of these, 26% were osteoporotic (BMD < −2.5 SDS), although we lack previous information on their bone mineralization evolution, i.e. whether they had bone density loss during the process of undernutrition and amenorrhea or just failed to attain the normal increase in bone mineralization, characteristic of the end of puberty (1). The degree of undernutrition in our patients in stage I corresponded to a weight loss between 10 and 25% (23 patients) and 26 and 40% (11 patients) of ideal weight. This explains why IGF-I, though low for age and sex, was not accompanied by high GH secretion (only one patient presented clear high urinary GH excretion) or by high IGFBP-1 and low IGFBP-3. Similar results were described by Golden et al.(24). This contrasts with other studies in which patients presented high GH secretion (25), high IGFBP-1, and low IGFBP-3 accompanying low IGF-I (26), although in the study of Argente et al.(27), IGF-I, IGFBP-3, and GHBP low levels did not correlate with the GH secretory status, which could be independently increased or decreased. Other studies have also shown high cortisol secretion (28–30) and low DHEA-S response to ACTH stimulation (31), and in accordance with the clinical characteristics previously mentioned, our patients presented normal urinary cortisol excretion and normal serum DHEA-S.
IGF-I is one of the principal regulators of bone metabolism (5, 6, 32–34); circulating serum levels of IGF-I correlate with BMD in the normal population (35–37), and other pathologies such as GH deficiency characterized by low circulating levels of IGF-I also present lowered BMD. IGF-I exerts a double effect on bone metabolism by stimulating osteoblastic activity and the resorption process (38). The need for normal estrogen secretion for bone mass acquisition and maintenance has been demonstrated in adolescent and young women (39, 40), and hypogonadal states are characterized by low mineralization not only in women but also in men lacking estrogen action (owing to E2 resistance or aromatase deficiency) (41). The effects of E2 on bone metabolism have been described as inhibitory for the resorption process, although direct effects on osteoblastic activity have been described (4, 42–44). Clinical data showed that estrogen and progesterone oral replacement therapy in amenorrheic AN patients was effective in preventing progressive osteopenia only in the subgroup with the lowest initial body weight, whereas a significant increase in BMD was only seen in fully recovered patients (45).
Recovery of normal BMI was characterized by normalization of IGF-I serum levels and lower IGFBP-I and SHBG, both known to be regulated by insulin secretion. Although patients in stage II remained amenorrheic, circulating total E2 levels were significantly higher than in stage I patients, which together with lower SHBG indicated a clearly higher free E2 fraction. Although normal cyclic gonadotrophin secretion had not been recovered, the increase in IGF-I may have stimulated granulosa cell E2 secretion. The conjunction of IGF-I and E2 increases explains the stimulation of osteoblastic activity (increase in all biochemical bone formation markers) and the decrease in osteoclastic activity (decrease in one of the bone resorption markers) and the significant decrease in calciuria. The overall change in bone metabolism represents a clear shift toward bone formation. In our study, this is reflected by slightly higher though not statistically significant BMD values. Recovery of normal circulating levels of gonadal steroids in stage III patients could lead to an increase in mean BMD-SDS, and the proportion of osteopenic and osteoporotic patients in this group is lower. However, longitudinal follow-up of patients is required for the clinical significance of these changes to be assessed. Our preliminary longitudinal study in 11 patients (19) showed a significant increase in BMD, resulting in values similar to those at the onset of the disease only after gonadal function was recovered. In addition, in the present study, patients remaining osteopenic in the stage of full clinical recovery showed higher bone turnover indicated by higher levels of bone formation and resorption markers.
Our study shows that only clinical data may correlate with BMD and that the most sensitive are BMI and duration of amenorrhea, followed by duration of regular menses before amenorrhea. BMD dependence on BMI has been detected in all clinical studies on BMD determinants (46). The relationship between BMD and duration of amenorrhea demonstrated in our study shows that periods longer than 20 mo predict BMD in the osteopenic range. The relationship between BMD and duration of regular menses before amenorrhea demonstrates that the longer the interval with menses after menarche, the less probable is the occurrence of osteopenia. Thus, the duration and normal progression of estrogenic activity throughout puberty and at the end of adolescence are crucial for the risk of osteopenia/osteoporosis when a disease such as AN develops. These two clinical data may support the recommendation of closer bone metabolism study and follow-up in patients at increased risk for osteopenia. However, some patients present osteopenia with shorter amenorrhea duration. This indicates that osteopenia genesis is multifactorial and that other bone mineralization regulators, including bone mass peaking achievement before the onset of illness, physical activity, and genetics, may be important in some individuals and that individual evaluation is warranted in these patients.
Biochemical markers of bone metabolism have been shown to correlate with bone metabolism changes occurring during physiologic and pathologic stages of human development: accelerated growth and mineralization during puberty, menopause, and a number of metabolic bone diseases (47–50). In our study, no correlation was found between BMD and any individual hormonal or biochemical bone metabolism marker, which indicates that none of these parameters could predict bone mineralization status. However, bone formation markers correlated positively with IGF-I and bone resorption markers negatively with E2, indicating that IGF-I is one of the major bone formation stimulators, whereas in the overall result of E2 action, bone resorption inhibition predominates. The highest correlation was found for PINP as a bone formation marker and for ICTP as a bone resorption marker. Hotta et al.(51) demonstrated a significant positive correlation of BMI, IGF-I, and IGFBP-3 with OC as bone formation marker, whereas a negative correlation for the bone resorption marker CrossLaps was only found with the BMI. Soyka et al.(52) also demonstrated that bone formation (indicated by OC and BAP) in AN was largely due to IGF-I levels; however, those authors found no increased bone resorption and did not study the effect of E2 levels. Serum bioavailable E2 was found to be an independent predictor of BMD in both men and postmenopausal women and to correlate negatively with the bone resorption marker urinary Ntx (53). Although our study is cross-sectional, the differences observed in bone metabolism markers between the different clinical stages of AN illustrate the shifts produced toward bone resorption or bone formation in accordance with nutritional (BMI and IGF-I) and hormonal status (IGF-I, E2, SHBG, PTH, 1,25VitD). The calcium metabolism balance was substantiated by calciuria, which was abnormally high in stage I patients and normalized in stages II and III and 1,25VitD levels that were significantly higher in stage III patients and that probably afforded higher intestinal calcium and phosphorus absorption for enhanced bone mineralization. In the subgroup of fully recovered patients who maintain BMD in the osteopenic range, the bone metabolism markers indicate accelerated bone turnover with an increase in both formation (OC and PINP) and resorption (ICTP), with no other biochemical or clinical differences having been detected to date. This subgroup of patients would, therefore, be candidates for the study of other bone mineralization determinants such as genetics.
In conclusion, our data indicate that in young postpubertal patients with AN, osteopenia is more frequent when patients initiate the process at younger ages and when the duration of amenorrhea is longer. The best predictors for osteopenia are clinical: duration of amenorrhea, duration of regular menses before amenorrhea, and actual BMI. Hormonal and bone metabolism markers in a cross-sectional point may be predicted by BMI, with IGF-I correlating positively with bone formation markers (PINP followed by BAP and OC) and E2 correlating negatively with bone resorption markers (only ICTP). Patients remaining osteopenic despite clinical and hormonal recovery present accelerated bone turnover. Thus, an individual initial evaluation of bone mineralization must be performed to characterize these patients who may require a longitudinal follow-up.
Abbreviations
- BMD:
-
bone mineral density
- AN:
-
anorexia nervosa
- BMI:
-
body mass index
- SDS:
-
standard deviation score
- DEXA:
-
dual energy x-ray absorptiometry
- IGFBP-3:
-
insulin-like growth factor binding protein 3
- IGFBP:
-
insulin-like growth factor binding protein 1
- E2:
-
estradiol
- SHBG:
-
sex hormone-binding globulin
- DHEA-S:
-
dehydroepiandrosterone sulphate
- PIINP:
-
amino-terminal propeptide of procollagen III
- OC:
-
osteocalcin
- BAP:
-
bone alkaline phosphatase
- PICP:
-
carboxy-terminal propeptide of procollagen I
- PINP:
-
amino-terminal propeptide of procollagen I
- ICTP:
-
carboxy-terminal telopeptide of collagen I
- 25-VitD:
-
25-OH-vitamin D
- 25-VitD:
-
1,25(OH)2-vitamin D
- PTH:
-
parathormone
- DPD:
-
deoxypyridinoline
- NTx:
-
amino-terminal telopeptide of collagen I
References
Del Rio L, Carrascosa A, Pons F, Gussinyé M, Yeste D, Domenech M 1994 Bone mineral density of the lumbar spine in white Mediterranean Spanish children and adolescents: changes related to age, sex, and puberty. Pediatr Res 35: 362–366
Rodan GA 1998 Control of bone formation and resorption: biological and clinical perspective. J Cell Biochem Suppl 30–31: 55–61
Mundy GR 1999 Cellular and molecular regulation of bone turnover. Bone 24: 35S–38S
Huang WH, Zheng MH 1999 Steroid hormones and bone. Histol Histopathol 14: 1257–1268
Ohlsson C, Bengtsson BA, Isaksson OGP, Andreassen TT, Slootweg MC 1998 Growth hormone and bone. Endocr Rev 19: 55–79
Van Wyk JJ, Smith EP 1999 Insulin-like growth factors and skeletal growth: possibilities for therapeutic interventions. J Clin Endocrinol Metab 84: 4349–4354
Stevens DA, Williams GR 1999 Hormone regulation of chondrocyte differentiation and endochondral bone formation. Mol Cell Endocrinol 151: 195–204
Müller EE, Locatelli V 1992 Undernutrition and pituitary function: relevance to the pathophysiology of some neuroendocrine alterations of anorexia nervosa. J Endocrinol 132: 327–329
Stoving RK, Hangaard J, Hansen-Nord M, Hagen C 1999 A review of endocrine changes in anorexia nervosa. J Psychiatr Res 33: 139–152
Rigotti NA, Nussbaum SR, Herzog DB, Neer RM 1984 Osteoporosis in women with anorexia nervosa. N Engl J Med 311: 1601–1606
Brotman AW, Stern TA 1985 Osteoporosis and pathologic fractures in anorexia nervosa. Am J Psychiatry 142: 495–496
Bachrach LK, Guido D, Katzman D, Litt IF, Marcus R 1990 Decreased bone density in adolescent girls with anorexia nervosa. Pediatrics 86: 440–447
Rigotti NA, Neer RM, Skates SJ, Herzog DB, Nussbaum SR 1991 The clinical course of osteoporosis in anorexia nervosa. A longitudinal study of cortical bone mass. JAMA 265: 1133–1138
Bachrach LK, Katzman DK, Litt IF, Guido D, Marcus R 1991 Recovery from osteopenia in adolescent girls with anorexia nervosa. J Clin Endocrinol Metab 72: 602–606
Kiriiki N, Iketani T, Nakanishi S, Nagata T, Inoue K, Okuno M, Ochi H, Kawakita Y 1992 Reduced bone mineral density and major hormones regulating calcium metabolism in anorexia nervosa. Acta Psychiatr Scand 86: 358–363
Seeman E, Szmukler GI, Formica C, Tsalamandris C, Mestrovic R 1992 Osteoporosis in anorexia nervosa: influence of peak bone density, bone loss, oral contraceptive use, and exercise. J Bone Miner Res 7: 1467–1474
Carrascosa A, Gussinyé M, Yeste D, Del Río L, Audí L, Enrubia M, Vargas D 1996 Skeletal mineralization during infancy, childhood, and adolescence in the normal population and in populations with nutritional and hormonal disorders. Dual X-ray absorptiometry (DEXA) evaluation. In: Schönau E (ed) Paediatric Osteology. New Developments in Diagnosis and Therapy. Elsevier Science B.V, Amsterdam, 93–102
Grinspoon S, Herzog D, Klibanski A 1997 Mechanisms and treatment options for bone loss in anorexia nervosa. Psychopharmacol Bull 33: 399–404
Carrascosa A, Gussinyé M, Audí L, Vargas D, Enrubia M 1998 Bone mass in anorexia nervosa patients. In: Schönau E, Matkovic V (eds). Paediatric Osteology. Prevention of Osteoporosis—a Paediatric Task? Elsevier Science Pte Ltd, Amsterdam, 95–102
Grinspoon S, Miller K, Coyle C, Krempin J, Armstrong C, Pitts S, Herzog D, Klibanski A 1999 Severity of osteopenia in estrogen-deficient women with anorexia nervosa and hypothalamic amenorrhea. J Clin Endocrinol Metab 84: 2049–2055
Lucas AR, Melton J III Crowson CS, O' Fallon WM 1999 Long-term fracture risk among women with anorexia nervosa: a population-based cohort study. Mayo Clin Proc 74: 972–977
American Psychiatric Association 1994 Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), 4th Ed. Washington, 558–559
Hernández M, Castellet J, Narvaiza JL, Rincón JM, Ruiz I, Sánchez E, Sobradillo B, Zurimendi A 1988 Curvas y tablas de crecimiento. Instituto de investigación sobre crecimiento y desarrollo. Fundación F. Orbegozo, Madrid
Golden NH, Kreitzer P, Jacobson MS, Chasalow FI, Schebendach J, Freedman SM, Shenker IR 1994 Disturbances in growth hormone secretion and action in adolescents with anorexia nervosa. J Pediatr 125: 655–660
Stoving RK, Veldhuis JD, Flyvbjerg A, Vinten J, Hangaard J, Koldkjaer OG, Kristiansen J, Hagen C 1999 Jointly amplified basal and pulsatile growth hormone (GH) secretion and increased process irregularity in women with anorexia nervosa: indirect evidence for disruption of feedback regulation within the GH-insulin-like growth factor axis. J Clin Endocrinol Metab 84: 2056–2063
Counts DR, Gwirtsman H, Carlsson LMS, Lesem M, Cutler GB Jr 1992 The effect of anorexia nervosa and refeeding on growth hormone-binding protein, the insulin-like growth factors (IGFs), and the IGF-binding proteins. J Clin Endocrinol Metab 75: 762–767
Argente J, Caballo N, Barrios V, Muñoz MT, Pozo J, Chowen JA, Morande G, Hernández M 1997 Multiple endocrine abnormalities of the growth hormone and insulin-like growth factor axis in patients with anorexia nervosa: effect of short- and long-term weight recuperation. J Clin Endocrinol Metab 82: 2084–2092
Biller BMK, Saxe V, Herzog DB, Rosenthal DI, Holzman S, Klibanski A 1989 Mechanisms of osteopenia in adult and adolescent women with anorexia nervosa. J Clin Endocrinol Metab 68: 548–554
Abrams SA, Silber TJ, Esteban NV, Vieira NE, Stuff JE, Meyers R, Majd M, Yergey AL 1993 Mineral balance and bone turnover in adolescents with anorexia nervosa. J Pediatr 123: 326–331
Carmichael KA, Carmichael DH 1995 Bone metabolism and osteopenia in eating disorders. Medicine 74: 254–267
Winterer J, Gwirtsman HE, George DT, Kaye WH, Loriaux DL, Cutler GB Jr 1985 Adrenocorticotropin-stimulated adrenal secretion in anorexia nervosa: impaired secretion at low weight with normalization after long-term weight recovery. J Clin Endocrinol Metab 61: 693–697
Jones JI, Clemmons DR 1995 Insulin-like growth factors and their binding proteins: biological actions. Endocr Rev 16: 3–34
Eriksen EF, Kassem M, Langdahl B 1996 Growth hormone, insulin-like growth factors, and bone remodelling. Eur J Clin Invest 26: 525–534
Langdahl BL, Kassen M, Moller MK, Eriksen EF 1998 The effects of IGF-I and IGF-II on proliferation and differentiation of human osteoblasts and interaction with growth hormone. Eur J Clin Invest 28: 176–183
Langlois JA, Rosen CJ, Visser M, Hannan MT, Harris T, Wilson PWF, Kiel DP 1998 Association between insulin-like growth factor I and bone mineral density in older women and men: the Framingham Heart Study. J Clin Endocrinol Metab 83: 4257–4262
Rosen CJ, Donahue LR 1998 Insulin-like growth factors and bone: the osteoporosis connection revisited. Proc Soc Exp Biol Med 219: 1–7
Mora S, Pitukcheewanont P, Nelson JC, Gilsanz V 1999 Serum levels of insulin-like growth factor I and the density, volume, and cross-sectional area of cortical bone in children. J Clin Endocrinol Metab 84: 2780–2783
Canalis E 1997 Insulin-like growth factors and osteoporosis. Bone 21: 215–216
Hergenroeder AC 1995 Bone mineralization, hypothalamic amenorrhea, and sex steroid therapy in female adolescents and young adults. J Pediatr 126: 683–689
Carrascosa A, Gussinyé M, Terradas P, Yeste D, Audí L, Vicens-Calvet E 2000 Spontaneous, but not induced, puberty permits adequate bone mass in adolescent Turner syndrome patients. J Bone Miner Res 15: 2005–2010
MacGillivray MH, Morishima A, Conte F, Grumbach M, Smith EP 1998 Pediatric endocrinology update: an overview. The essential roles of estrogens in pubertal growth, epiphyseal fusion, and bone turnover: lessons from mutations in the genes for aromatase and the estrogen receptor. Horm Res 49: ( suppl 1): 2–8
Marcus R 1998 New perspectives on the skeletal role of estrogen. J Clin Endocrinol Metab 83: 2236–2238
Delaveyne-Bitbol R, Garabedian M 1999 In vitro responses to 17β-estradiol throughout pubertal maturation in female human bone cells. J Bone Miner Res 14: 376–385
Robinson JA, Waters KM, Turner RT, Spelsberg TC 2000 Direct action of naturally occurring estrogen metabolites on human osteoblastic cells. J Bone Miner Res 15: 499–506
Klibanski A, Biller BMK, Schoenfeld DA, Herzog DB, Saxe VC 1995 The effects of estrogen administration on trabecular bone loss in young women with anorexia nervosa. J Clin Endocrinol Metab 80: 898–904
Bergenstal RM, Fish LH, List S 1998 Body weight predicts bone density better than resorption markers. Arch Intern Med 158: 298
Robins SP, New SA 1997 Markers of bone turnover in relation to bone health. Proc Nutr Soc 56: 903–914
Bikle DD 1997 Biochemical markers in the assessment of bone disease. Am J Med 103: 427–436
Christenson RH 1997 Biochemical markers of bone metabolism: an overview. Clin Biochem 30: 573–593
Garnero P, Delmas PD 1998 Biochemical markers of bone turnover. Applications for osteoporosis. Endocrin Metab Clin North Am 27: 303–323
Hotta M, Fukuda I, Sato K, Hizuka N, Shibasaki T, Takano K 2000 The relationship between bone turnover and body weight, serum insulin-like growth factor (IGF) I, and serum IGF-binding protein levels in patients with anorexia nervosa. J Clin Endocrinol Metab 85: 200–206
Soyka LA, Grinspoon S, Levitsky LL, Herzog DB, Klibanski A 1999 The effects of anorexia nervosa on bone metabolism in female adolescents. J Clin Endocrinol Metab 84: 4489–4496
Khosla S, Melton LJ III, Atkinson EJ, O'Fallon WM, Klee GG, Riggs BL 1998 Relationship of serum sex steroid levels and bone turnover markers with bone mineral density in men and women: a key role for bioavailable estrogen. J Clin Endocrinol Metab 83: 2266–2274
Acknowledgements
The authors thank Dr. Lluis Armadans from the Preventive Medicine and Epidemiology Service in Hospitals Vall d'Hebron for his contribution to the statistical analyses. We also thank Christine O'Hara for useful help with the English version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by Spanish grants from Fondos de Investigación Sanitaria (FIS) numbers 94/0466 and 99/1067 and by Novo-Nordisk Spain.Both L.A. and D.M.V. contributed equally to this work.This study received the 1999 Award for Research in Pediatrics from Agrupación Mutua del Comercio y de la Industria.
Rights and permissions
About this article
Cite this article
Audí, L., Vargas, D., Gussinyé, M. et al. Clinical and Biochemical Determinants of Bone Metabolism and Bone Mass in Adolescent Female Patients with Anorexia Nervosa. Pediatr Res 51, 497–504 (2002). https://doi.org/10.1203/00006450-200204000-00016
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200204000-00016
This article is cited by
-
Bone mineral density and oxidative stress in adolescent girls with anorexia nervosa
European Journal of Pediatrics (2022)
-
Vitamin D status in young Swedish women with anorexia nervosa during intensive weight gain therapy
European Journal of Nutrition (2017)
-
The Unexplored Crossroads of the Female Athlete Triad and Iron Deficiency: A Narrative Review
Sports Medicine (2017)
-
Skeletal outcomes by peripheral quantitative computed tomography and dual-energy X-ray absorptiometry in adolescent girls with anorexia nervosa
Osteoporosis International (2016)
-
An Overview of the Metabolic Functions of Osteocalcin
Current Osteoporosis Reports (2015)