Abstract
We report here a case with severe intrauterine growth restriction from the first trimester and clinical features of Silver-Russell syndrome including microcephaly, low-set ear, atrial septum defect, ventricular septum defect, diaphragmatic relaxation, and rocker bottom feet. Silver-Russell syndrome is thought to result from deletion of the distal long arm of chromosome 15 on which the IGF-I receptor (IGF-IR) gene is located. We measured both the maternal and cord blood levels of GH, IGF-I, and IGF-binding protein and performed an immunohistochemical study of IGF-IR in the placenta to investigate whether these IGF-related proteins were affected in this patient. The hormonal level of these proteins did not significantly differ from normal neonates, and immunohistochemical analysis suggested IGF-IR protein levels in the placenta were comparable to normal term neonates. These results support the hypothesis that growth insufficiency could occur in patients with monosomy of the distal long arm of chromosome 15 and suggest a critical threshold for IGF-related fetal growth in early pregnancy.
Similar content being viewed by others
Main
Silver-Russell syndrome is one of the clinical entities causing severe IUGR. Monosomy of the IGF-IR gene resulting from deletion of the distal long arm of chromosome 15 has been identified in patients presenting with features of Silver-Russell syndrome (1). Sieblar et al. (2) report decreased IGF-IR receptor number and mRNA expression in cultured fibroblasts from two patients diagnosed with this syndrome shown to be hemizygous for the IGF-IR gene. These findings demonstrate that loss of even a single copy of the IGF-IR gene could cause severe growth defects.
IGFs and their binding proteins (IGFBPs) are thought to have an important role in fetal growth (3). Several reports have provided evidence of abnormalities of the IGF-IR in patients with short stature (4–6). The IGF-related proteins null mice show severe defects in intrauterine growth (7) and multiple investigators have reported low levels of IGF-I at birth in IUGR fetuses (8–10). Taken together, these studies support the hypothesis that IGF-related proteins play a key role in fetal development. Based on this model, one might expect patients with Silver-Russell syndrome to have abnormal levels of hormonal and cellular IGF-related proteins. Unfortunately, there has been limited information on serum hormone levels for patients with this syndrome. The GH and IGF-I levels reported in infants are essentially normal except for one report of a single elevated measurement at 2 y of age (3). There has been no information in the published literature concerning hormone levels at birth in patients diagnosed with this syndrome.
We have diagnosed antenatally a case of partial monosomy of chromosome 15 associated with features of Silver-Russell syndrome. The fetus showed several deformities and severe IUGR occurred in the first trimester. To investigate the profile of the IGF axis in this case, we measured IGF-related protein levels in cord blood and performed IGF-IR staining in the placenta.
CASE PRESENTATION
A 27-y-old Japanese woman, gravida 1, para 0, went to a private gynecologist and was diagnosed to be at 6 wk of gestation. At 9 wk of gestation, the expected date of delivery was confirmed by crown-rump length. From 13 wk of gestation, the fetal biparental diameter (BPD) was sustained around the mean −2.5 SD. Although amniocentesis was performed to exclude chromosomal abnormality, fetal karyotype was diagnosed as normal, 46XX. She was referred to our hospital under the diagnosis of severe IUGR at 28 wk of gestation.
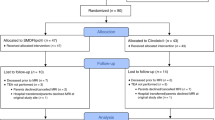
On admission, the estimated fetal body weight was 580 g (mean −3 SD). Maternal vascular disease, maternal metabolic disorders, and fetomaternal infectious diseases were excluded. Oligohydramnios, tetralogy of Fallot, single umbilical artery, and diaphragmatic relaxation were suspected by ultrasound scan. Amniocentesis was repeated and precise fetal karyotype analysis using GTG-banded analysis and fluorescent in situ hybridization (FISH) analysis confirmed the chromosomal aberration of 46XX, der (15) t (15; ?) (q26; ?), ish der (15) (wcp215-, D15S396-) (Fig. 1).
FISH analysis in fetal chromosome. Fluorescent in situ hybridization (FISH) was performed using probes recognizing chromosome 15. Left panel: whole chromosome paint, red staining;right panel: D15Z (green arrows) and D15S396 (red arrow), which are specific for the proximal and distal region of the chromosome 15, respectively.
After counseling and discussion with the patient and her husband, we kept the patient in ward to monitor the fetus closely. The parents desired active resuscitation and intensive treatment for the neonate. At 38 wk of gestation, fetal growth was judged to have ceased and labor was induced. A cesarean section was performed in response to nonreassuring fetal status with impending profound hypoxemia indicated by cardiotocogram. The baby weighed 898 g with cord blood pH of 7.356 and an Apgar score of 6 and 7 at 1 and 5 min, respectively. The placenta weighed 120 g and appeared histologically normal. The baby showed the phenotype of Silver-Russell syndrome with microcephaly, low-set ear, atrial septum defect, ventricular septum defect, diaphragmatic relaxation, and rocker bottom feet and was referred to the neonatal intensive care unit. The baby was treated with nitrogen oxide, prostaglandins, digitalization, and high-frequency oxygenation due to persistent heart failure and pulmonary hypertension. She died from circulation failure on d 135 after birth.
Both the patient and her husband underwent chromosomal analysis after delivery and it was determined that the husband had a translocation of 46XY t (15, 18)(q26: p11.2) (Fig. 2).
MATERIALS AND METHODS
Measurement of GH, IGF-I, and IGFBP3 and Immunohistochemical Study
All analysis was performed after obtaining consent from the parent and the study was approved by the applicable institutional review board.
To measure GH, IGF-I, and IGFBP3, RIA was performed using the commercially available GH-kit (Daiichi Radioisotope Laboratories, Kenkyusho, Tokyo, Japan), Somatomedine C (II) (Byel Medical, Tokyo, Japan), and IGFBP3-IRMA (Daiichi Radioisotope), respectively. All measurements were performed by a commercial service (BML, Tokyo, Japan)
Immunohistochemical analysis for IGF-IR in placenta was performed by the labeled polymer method using the EnVision+ kit (DAKO, Carpinteria, CA, U.S.A.). Placental tissue excised through the full thickness immediately after delivery was formalin-fixed and paraffin-embedded. Four-micrometer sections were deparaffinized and rehydrated. After blocking endogenous peroxidase with 0.3% hydrogen peroxidase in methanol for 30 min, slides were washed and microwaved for 15 min in 10 mM citrate buffer (pH 6.0) to enhance antigen detection. Slides were then incubated with rabbit anti-IGF-IRα polyclonal antibody (diluted 1:100; Santa Cruz Biochemicals, Santa Cruz, CA, U.S.A.) for 60 min and exposed to goat anti-rabbit Ig conjugated to peroxidase-labeled dextran polymer for 20 min, followed by staining with 3,3′-diaminobenzidine tetrahydrochloride. Counterstaining with hematoxylin followed. Normal full-term placenta was used as a positive control.
RESULTS
Table 1 shows GH, IGF-I, and IGFBP3 levels from cord blood and maternal blood taken just after delivery. All hormonal levels were essentially normal in both maternal vein and cord blood.
To address whether fetal IGF-IR protein expression was affected, we performed immunohistochemical staining with anti-IGF-IR antibody in the placenta of the patient and normal full-term controls. These controls were confirmed to have normal karyotype. Surprisingly, the expression of IGF-IR was not different between the patient and controls (Fig. 3).
Immunohistochemical staining against IGF-I receptor. Each block of tissues was collected immediately after delivery and prepared as described in “Materials and Methods.” The tissues were then stained by anti-IGF-IR antibody and visualized by horseradish peroxidase labeling. The expression of IGF-IR was not different between the patient and controls. (a) Patient's placenta; (b) and (c) placenta from normal full-term delivery. Magnification ×400.
DISCUSSION
Herein we reported profiles of IGF-related proteins at delivery in a case of antenatally diagnosed distal 15q deletion. Although we could not perform Southern blot analysis on the IGF-IR gene, the clinical phenotype corresponded to that of Silver-Russell syndrome (1). FISH analysis confirmed the deletion of distal chromosome 15q (Fig. 1), and the aberrant chromosome is considered derived from paternal translocation, 18p. Silver-Russell syndrome, as well as ring chromosome 15 syndrome, are both associated with terminal 15q deletions (1, 11) thought to result in IUGR and postnatal growth failure in addition to other developmental abnormalities. It has been proposed that absence of one copy of the IGF-IR gene located on the affected chromosome in these syndromes plays a major role in growth insufficiency (3, 12). There have been many reports on IGF-related proteins in cord and maternal blood during pregnancy, suggesting a correlation between these proteins and fetal growth (8–10). Experiments using knockout mice provided support that IGF systems play a major role in antenatal/postnatal growth (7, 13). Taken together, it is most likely that loss of one copy of IGF-IR is involved in the pathophysiology of the present case.
Lacking one copy of the IGF-IR gene might be expected to cause primary IGF-I resistance through a quantitative deficiency of the receptor, resulting in end-organ insensitivity and negative feedback by IGF-I levels (3). However, in the present case, there was no significant elevation in IGF-I level in cord blood, nor was any evidence of negative feedback found. The GH and IGFBP3 levels were also normal. There has been limited information on serum hormone levels in patients diagnosed with this syndrome (Table 2) and the GH and IGF-I levels reported in infants are essentially normal except for a single elevated measurement at 2 y of age (3). There has been no information in the published literature concerning hormone levels at birth for this syndrome. Our results indicated that IGF-related protein levels were essentially normal in Silver-Russell syndrome even at birth.
No significant differences in IGF-IR expression were observed in the immunohistochemical staining of the placenta when compared with normal controls. Holmes et al. (14) detected IGF-IR in endothelial cells, stromal cells, trophoblasts, and deciduas and the intensity of staining was not different among small-for-gestational-age neonates, IUGR, and normal controls. The independence of placental IGF-IR levels to changes in fetal growth was also reported by Culler et al. (15). Sieblar et al. (2) reported decreased IGF-IR receptor number and mRNA expression in cultured fibroblasts from two patients hemizygous for the IGF-IR gene, but they could not find any impaired biologic response to IGF-I in these cells. These findings suggested that there might be another essential mechanisms in IGF-I–IGF-IR function as well as the amount of receptor protein. Unfortunately, we could not assess the exact amount of IGF-IR protein from our immunohistochemical analysis. However, it may be assumed that there is a critical threshold for IGF in determining fetal growth at the early phase of pregnancy because the growth restriction began in the first trimester.
We analyzed IGF-related proteins in cord blood and IGF-IR expression in placenta at birth in a case of Silver Russell syndrome diagnosed antenatally with monosomy of the distal long arm of chromosome 15 resulting in growth insufficiency and phenotypic diagnosis of Silver-Russell syndrome. We did not observe reduced IGF-IR expression nor was negative feedback in IGF axis demonstrated. This result supports previous studies of affected infants and suggests that normal protein levels are present at birth (16–18).
Abbreviations
- IGFBP:
-
IGF binding protein
- IGF-IR:
-
IGF I receptor
- IUGR:
-
intrauterine growth restriction
References
Roback EW, Barakat VG, Mbikay DM, Chretien M, Butler MG 1995 An infant with deletion of the distal long arm of chromosome 15 (q26.1→qter) and loss of insulin like growth factor 1 receptor gene. Am J Med Genet 38: 74–79
Siebler T, Lopaczynski W, Terrry CL, Casella SJ, Munson PM, Leon DD, Phang L, Blakemore KJ, Mcevoy RC, Kelley R, Nissley P 1995 Insulin like growth factor 1 receptor expression and function in fibroblasts from two patients with deletion of the distal long arm of chromosome 15. J Clin Endo Metabol 80: 3447–3457
Jain S, Goled DW, Bailey R, Geffner ME 1998 Insulin like growth factor 1 resistance. Endocr Rev 19: 625–646
Bierich FR, Moeller H, Ranke MB, Rosenfeld RG 1984 Pseudopituitary dwarfism due to resistance to somatomedin; a new syndrome. Eur J Pediatr 142: 186–188
Van Obberghen-Schilling EE, Rechler MM, Romanus JA, Knight AB, Nissley SP, Humbel RE 1981 Receptors for insulin-like growth factor I are defective in fibroblasts from a patient with leprechaunism. J Clin Invest 68: 1356–1365
Geffner ME, Bailey RC, Bersch N, Vera JC, Golde DW 1993 Insuline likegrowth factor I unresponsiveness in an Efe pygmy. Biophysis Res Commun 13: 566–595
Baker J, Liu JP, Robertson E, Efstratiadis A 1993 Role of growth factors in embryonic and postnatal growth. Cell 75: 73–82
Hills FA, English J, Chard T 1996 Circulating levels of IGF-I and IGF-binding protein throughout pregnancy: relation to birth weight and maternal weight. J Endocrinol 148: 303–309
Bennett Am, Wilson DM, Liu F, Nagashima R, Rosenfeld RG, Hintz RL 1983 Levels of insulin like growth factors 1 and 2 in human cord blood. J Clin Endocrinol Metabol 57: 609–612
Lassarre C, Hardouin S, Daffos F, Forestier F, Frankenne F, Binoux M 1991 Serum insulin-like growth factors and insulin-like growth factor binding proteins in the human fetus: relationships with growth in normal subjects and in subjects with intrauterine growth retardation. Pediatr Res 29: 219–225
Yang SW, Yu JS 2000 Relationship of insulin-like growth factor 1, insulin-like growth factor binding protein 3, insulin, growth hormone in cord blood and maternal factors with birth height and birth weight. Pediatr Int 42: 31–36
Guidice LC, Martina NA, Crystal RA, Tazuke S, Druzin M 1997 Insulin-like growth factor binding protein-1 at the maternal–fetal interface and insulin-like growth factor-2 and insulin-like growth factor binding protein-1 in the circulation of women with severe preeclampsia. Am J Obstet Gynecol 176: 751–758
Pirazzoli P, Cacciari E, De Iasio R, Pittalis MC, Dallacasa P, Zucchini S, Guali S, Salardi S, David C, Boschi S 1997 Developmental pattern of fetal growth hormone, insulin-like growth factor 1, growth hormone binding protein and insulin-like growth factor binding protein 3. Arch Dis Child Fetal Neonatal Ed 77: 100–104
Tamura T, Tohma T, Ohta T, Soejima H, Harada N, Abe K, Niikawa N 1993 Ring chromosome 1 involving deletion of the insulin-like growth factor 1 receptor gene in a patient with features of Silver-Russell syndrome. Clin Dysmorphol 2: 106–113
Alsat E, Marcotty C, Gabriel R, Igout A, Frankenne F, Hennen G, Evain-Brion D 1995 Molecular approach to intrauterine growth retardation: an overview of recent data. Reprod Fertil Dev 7: 1457–1464
Accili D, Nakane J, Kim JJ, Park B, Rother KI 1999 Targeted gene mutations define the roles of insulin and IGF-I receptors in mouse embryonic development. J Pediatr Endocrinol Metab 12: 475–485
Holmes R, Porter H, Newcomb P, Holly JMP, Soothill P 1999 An immunohistochemical study of type 1 insulin-like growth factor receptors in the placenta of pregnancies with appropriately grown of growth restricted fetuses. Placenta 20: 325–330
Culler FL, Tung RF, Jansons RA, Moiser HD 1996 Growth promoting peptides in diabetic and non-diabetic pregnancy: interactions with trophoblastic receptors and serum carrier proteins. J Pediatr Endocrinol Metab 9: 21–29
Acknowledgements
The authors thank Dr. H. Nakayama, Maternity and Perinatal Care Unit, Kyushu University Hospital, for information about neonatal management.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported, in part, by a grant-in-aid from the Ministry of Education (12671608, 12671613).
Rights and permissions
About this article
Cite this article
Fukushima, K., Komatsu, H., Matsumoto, M. et al. IGF-Related Proteins at Birth in a Case of Antenatally Diagnosed Silver-Russell Syndrome. Pediatr Res 51, 323–327 (2002). https://doi.org/10.1203/00006450-200203000-00010
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200203000-00010
This article is cited by
-
Array comparative genomic hybridization in patients with congenital diaphragmatic hernia: mapping of four CDH-critical regions and sequencing of candidate genes at 15q26.1–15q26.2
European Journal of Human Genetics (2006)
-
Clinical Examples of Disturbed IGF Signaling: Intrauterine and Postnatal Growth Retardation due to Mutations of the Insulin-Like Growth Factor I Receptor (IGF-IR) Gene
Reviews in Endocrine and Metabolic Disorders (2005)