Abstract
Respiratory syncytial virus (RSV) is the most important respiratory pathogen in infancy and early childhood and may predispose to subsequent lower respiratory tract illness. Recent data indicate that RSV up-regulates the substance P receptor, making the airways abnormally susceptible to the proinflammatory effects of this peptide released from sensory nerves. The present study was designed to determine whether the administration of RSV antibodies prevents the potentiation of neurogenic inflammation in rat airways. Five days after inoculation, sensory nerve-mediated extravasation of Evans blue-labeled albumin was significantly greater in the airways of RSV-infected rats than in pathogen-free controls. Polyclonal immune globulin enriched for RSV-neutralizing antibodies (RSVIG) reduced neurogenic extravasation when injected 24 h before intranasal inoculation of the virus but not when injected before endotracheal inoculation. A humanized MAb against RSV fusion protein (palivizumab) was twice as potent as RSVIG when given before intranasal inoculation and also caused significant inhibition after endotracheal inoculation. Furthermore, palivizumab inhibited neurogenic inflammation in RSV-infected rats when given 72 h after virus inoculation. These data suggest that palivizumab protects the respiratory tract from RSV-induced inflammation when given before or in the early phase of the viral infection. The administration of palivizumab to high-risk infants may limit the severity of the acute airway inflammation and may protect against subsequent lower respiratory tract illness.
Similar content being viewed by others
Main
RSV infection presents a large public health burden worldwide. This virus is estimated to cause up to 90% of the cases of bronchiolitis and approximately 50% of all pneumonia in infancy, resulting in over 90 000 hospitalizations and 4500 deaths annually in the United States (1). Furthermore, there is mounting interest in the hypothesis that RSV infection in early childhood is an important risk factor for the subsequent development of recurrent wheezing and asthma (2, 3). The natural portal of entry for this virus is the nose, and the infection usually remains confined to the respiratory tract, spreading by cell-to-cell transfer from the upper to the lower airway.
The mechanisms by which this virus causes airway inflammation and hyperreactivity are still unclear. Recently, we found in a rat model that lower respiratory tract infection with RSV causes a strong potentiation of neurogenic-mediated inflammation (4, 5), which has been proposed as playing an important role in the pathophysiology of asthma (6). Specifically, the increase in microvascular permeability evoked by the stimulation of sensory nerves is exaggerated during RSV infection due to up-regulation of the high-affinity neurokinin-1 receptor for the neuropeptide substance P (7). We have also found that the potentiation of this inflammatory pathway is a long-term phenomenon, which persists after the virus has been cleared from the lung (8).
The therapeutic options for the management of RSV infections are limited and their indications and efficacy remain unclear, but significant progress has been made in the area of passive prophylaxis. Human-derived RSVIG (RespiGam, Massachusetts Public Health Laboratories, Boston, MA) was licensed in 1996 by the U.S. Food and Drug Administration for the prevention of serious lower respiratory tract disease caused by RSV in premature infants and infants with bronchopulmonary dysplasia (9). More recently, a humanized MAb against the surface fusion (F) glycoprotein (palivizumab, MEDI-493, Synagis, MedImmune, Inc., Gaithersburg, MD) was licensed with similar indications (10). Whereas RSV antibodies prevent the development of severe disease in a large proportion of patients, it is not known whether they protect against the inflammatory sequelae of RSV infection, particularly childhood asthma.
With this study, we sought to determine in our rat model whether the prophylactic administration of RSVIG or palivizumab prevents the exaggerated neurogenic-mediated inflammation of the lower respiratory tract caused by inoculation of RSV either in the upper airways (intranasal route) or in the lower airways (endotracheal route). In addition, we tested whether palivizumab reduces neurogenic inflammation in RSV-infected rats when given 72 h after intranasal inoculation of the virus.
METHODS
Animals.
We used a total of 99 adult (12 wk of age) Fischer F-344 pathogen-free male rats from Charles River Breeding Laboratories (Raleigh, NC). Average body weight in the RSV group (n = 67) was 249 ± 3 g before inoculation and 246 ± 2 g after 5 d of incubation. In contrast, pathogen-free rats gained weight during the 5-d period (246 ± 2 to 264 ± 3 g;n = 32). To prevent microbial contamination, groups of two or three rats each were housed in polycarbonate cages isolated by polyester filter covers. These cages were placed on racks providing positive individual ventilation with class 100 air to each cage at the rate of approximately one cage change of air per minute (Maxi-Miser, Thoren Caging Systems, Hazleton, PA). We used separate rooms for housing infected and pathogen-free rats serviced by specifically trained husbandry technicians. All manipulations were conducted inside a class 100 laminar flow hood. Bedding, water, and feed were autoclaved before use, and the packages were opened only under the laminar flow hood. Cages and water bottles were run through a tunnel washer after each use and disinfected with both chemicals and heat. The experimental procedures followed in this study were approved by the Division of Veterinary Resources of the University of Miami School of Medicine.
Preparation of RSV suspensions.
HEp-2 cells from the American Type Culture Collection (ATCC; Rockville, MD) were grown in MEM (GIBCO-BRL, Grand Island, NY) supplemented with 10% fetal bovine serum (GIBCO-BRL). Confluent monolayers of HEp-2 cells were infected with 0.1 plaque-forming units of human RSV Long strain (ATCC), and the infection was allowed to proceed at 37°C in 5% CO2 atmosphere until more than 75% of the cells exhibited cytopathic effect. Cell debris was removed by centrifugation at 9500 ×g for 20 min in a refrigerated centrifuge (4°C). Aliquots of the virus stock were snap-frozen in liquid nitrogen and stored at −70°C. Before inoculation, the virus stock was titrated and diluted as needed for a final titer of 5 × 104 TCID50 in 0.1 mL. Supernatants and cell lysates from virus-free flasks of HEp-2 cells in MEM were harvested, centrifuged, and aliquoted following the same protocol to obtain the virus-free medium used as a sham infection control.
Virus inoculation.
Rats were inoculated either intranasally or endotracheally under sodium pentobarbital anesthesia (50 mg/kg i.p.). For intranasal inoculation, 50 μL of virus suspension was deposited in each nostril. For endotracheal inoculation, the vocal cords were visualized with a rodent laryngoscope, and the trachea was carefully intubated with a 16-gauge cannula (11). An 18-gauge inner cannula connected to a tuberculin syringe was passed through the endotracheal cannula to deposit 100 μL of virus suspension over the airway mucosa between the cricoid cartilage and the first tracheal ring. The rats used in this study were inoculated with RSV suspensions containing 5 × 104 TCID50 in 0.1 mL (7). Control rats were dosed with 100 μL of virus-free medium.
Virus detection.
Immunoperoxidase staining for RSV detection was performed on formalin-fixed 3-μm-thick lung sections. Endogenous peroxidase activity was blocked by incubation in 6% hydrogen peroxide for 5 min. The sections were incubated for 30 min in a humidity chamber with a 1:400 dilution of a pool of mouse MAb composed of four clones specific for the matrix 2 (M2) protein, phosphoprotein (P), F protein, and nuclear (N) protein of human RSV (Vector Laboratories, Burlingame, CA). This technique has been shown to maximize the sensitivity of RSV detection (12). The localization of RSV antigens was delineated by the streptavidin-biotin peroxidase complex method by use of an immunostaining kit (DAKO, Carpinteria, CA) and developed with the 3,3′-diaminobenzidine tetrahydrochloride chromogen. With this technique, cells expressing viral antigens are stained with a dark-brown precipitate lining the cell membrane and cytoplasm (Fig. 1). All slides were coded and were interpreted by a pathologist who did not know whether the section corresponded to an RSV-inoculated or to a medium-inoculated animal.
RSV detection in lungs from rats killed 5 d after inoculation. Immunoperoxidase staining was performed using a pool of mouse MAb composed of four clones specific for the matrix 2 (M2) protein, phosphoprotein (P), F protein, and nuclear (N) protein of human RSV. There was no detectable virus in the lungs of control rats inoculated with virus-free medium (top). A dark-brown reaction reveals the presence of viral antigens on the membranes and in the cytoplasm of infected bronchiolar epithelial cells (bottom). Internal scale = 25 μm.
Albumin extravasation.
The increase in vascular permeability in response to sensory nerve stimulation with capsaicin was measured 5 d after inoculation of the virus on the basis of previous studies of neurogenic inflammation in rats infected with RSV or with other respiratory viruses (7, 11, 13, 14). Also, previous studies in rodents suggest that RSV titer peaks in the lungs 4 to 5 d after inoculation (15).
The rats were anesthetized with sodium pentobarbital and injected with Evans blue dye (30 mg/kg i.v. over 5 s) to measure the extravasation of albumin from airway blood vessels (16). Immediately after the injection of the tracer, groups of RSV-infected and pathogen-free rats received an intravenous injection of capsaicin (75 μg/kg over 2 min) to stimulate the release of the neuropeptides contained in sensory nerves of the airways mucosa (17). Capsaicin (8-methyl-N-vanillyl-6-nonenamide; Sigma Chemical Co., St. Louis, MO) was dissolved in a vehicle having a final concentration of 0.75% ethanol, 0.375% Tween 80, and 0.85% NaCl in aqueous solution.
Five minutes after injection of the tracer, the chest was opened, a cannula inserted into the ascending aorta through the left ventricle, and the circulation perfused for 2 min with PBS (Sigma Chemical Co.) by using a syringe pump set at the rate of 50 mL/min. The extrapulmonary airways (from the first tracheal ring to the end of the main stem bronchi) were dissected and prepared for Evans blue extraction. The specimens free of connective tissue and opened along the ventral midline were blotted, weighed, and incubated in 1 mL of formamide (Sigma Chemical Co.) at 50°C for 18 h to extract the extravasated Evans blue dye.
The extravasation of Evans blue-labeled albumin from the tracheobronchial microcirculation was quantified by measuring the OD of the formamide extracts at a wavelength of 620 nm (16). The quantity of Evans blue dye extravasated in the airway tissues, expressed in nanograms per milligram of wet weight, was interpolated from a standard curve of Evans blue concentrations (0.5 to 10 μg/mL).
Experimental protocols.
RSV was inoculated either intranasally or endotracheally 24 h after the injection of RSV antibodies. After we found the protective effect of palivizumab against RSV delivered to the lower airways, we tested this antibody 72 h after intranasal inoculation of the virus. The 72-h interval was chosen on the basis of previous studies (15) with the goal of injecting the antibody before the phase of maximal viral replication, which starts 4 to 5 d after intranasal inoculation.
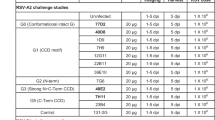
We studied four treatment groups:a) RSVIG (750 mg/kg, 15 mL/kg i.v.);b) RSVIG vehicle (albumin 10 mg/mL and sucrose 50 mg/mL in water; 15 mL/kg i.v.);c) palivizumab (15 mg/kg, 1 mL/kg s.c.); and d) palivizumab vehicle (0.9% NaCl; 1 mL/kg s.c.). The dose of RSVIG and palivizumab used for these experiments corresponds to the dose currently used in routine clinical practice on the basis of previous studies conducted in animal models (18, 19).
Control rats inoculated either intranasally or endotracheally with RSV or with virus-free medium received no treatment and were injected with capsaicin 5 d after inoculation. In addition, we studied groups of pathogen-free rats treated with palivizumab 24 h before or 72 h after intranasal instillation of virus-free medium to confirm that the antibody had no direct effect on the neurogenic inflammatory cascade.
Statistical analysis.
Data are expressed as the mean ± SEM. The effects of RSV and RSV antibodies on mean values of Evans blue extravasation were analyzed by 2-factor ANOVA (20). Multiple comparisons between means were performed with the Fisher protected least significant difference test (21). Statistical analysis was performed using the software SuperANOVA (Abacus Concepts, Berkeley, CA). Differences having a p value < 0.05 were considered significant.
RESULTS
Immunoperoxidase staining performed on lung sections from rats killed 5 d after either intranasal or endotracheal inoculation of RSV confirmed the presence of viral antigens on the membranes and in the cytoplasm of bronchiolar epithelial cells (Fig. 1, bottom). As described previously (7), the histopathologic changes caused by RSV consisted of a predominantly mononuclear cell infiltration in the bronchiolar mucosa. No virus was detected in the airways of rats dosed with virus-free medium (Fig. 1, top). In addition, rats inoculated with RSV and treated with palivizumab had no evidence of viral antigens or histopathologic changes in the bronchiolar epithelium.
After pharmacologic stimulation of sensory nerves with capsaicin, Evans blue extravasation in the airways of RSV-infected rats increased significantly (p < 0.01;n = 5–6 rats per group) and was approximately twice that measured in pathogen-free controls injected with the same dose of capsaicin. The magnitude of this potentiation was similar after intranasal or endotracheal inoculation of the virus (Figs. 2 and 3, open bars). Pretreatment with vehicle of either RSVIG or palivizumab 24 h before RSV inoculation did not affect capsaicin-induced extravasation in infected airways (Figs. 2 and 3, hatched bars).
Effect of pretreatment with RSV antibodies on capsaicin-induced neurogenic inflammation in the airways of rats 5 d after intranasal inoculation of RSV. Control rats inoculated intranasally with virus-free medium or with RSV received no pretreatment. RSVIG, palivizumab, or the respective vehicle was injected 24 h before viral inoculation. The extravasation of Evans blue-labeled albumin produced by capsaicin in infected rats was partially reduced by RSVIG, but palivizumab had a stronger inhibitory effect, abolishing virus-induced potentiation. ★p < 0.05; ★★★p < 0.001 = significantly different from RSV-infected rats pretreated with vehicle.
Effect of pretreatment with RSV antibodies on capsaicin-induced neurogenic inflammation in the airways of rats 5 d after endotracheal inoculation of RSV. Control rats inoculated endotracheally with virus-free medium or with RSV received no pretreatment. RSVIG, palivizumab, or the respective vehicle was injected 24 h before viral inoculation. The extravasation of Evans blue-labeled albumin produced by capsaicin in infected rats was strongly inhibited by palivizumab, whereas RSVIG had no significant effect. ★★p < 0.01 = significantly different from RSV-infected rats pretreated with vehicle.
RSVIG pretreatment 24 h before inoculation with RSV via the intranasal route (Fig. 2, center bars) reduced capsaicin-induced Evans blue extravasation in the airways by 30% (p = 0.03;n = 5–6) compared with RSV-infected rats pretreated with vehicle. However, extravasation in RSVIG-treated infected rats was still significantly larger than in pathogen-free controls (p = 0.04). In contrast, the inhibitory effect obtained using palivizumab before intranasal RSV inoculation (Fig. 2, right bars) was much stronger (−61%, p = 0.0001;n = 5), and extravasation in palivizumab-treated infected rats was not different from pathogen-free controls (p = 0.98).
RSVIG administered before endotracheal RSV inoculation (Fig. 3, center bars) did not have any inhibitory effect (p = 0.39;n = 7–8). In contrast, palivizumab inhibited significantly capsaicin-induced Evans blue extravasation in the airways of rats inoculated with RSV via the endotracheal route (Fig. 3, right bars), although the magnitude of this inhibitory effect (−45%, p = 0.002;n = 5) was smaller than with intranasal inoculation.
Because palivizumab was effective against RSV infecting the lower respiratory tract, we investigated whether this MAb given after intranasal inoculation of the virus still inhibits neurogenic inflammation. Palivizumab administered 72 h after intranasal inoculation of RSV (Fig. 4, top) inhibited neurogenic inflammation in infected airways by 47% (p = 0.005;n = 5). Again, the magnitude of this inhibitory effect was smaller than with palivizumab given 24 h before intranasal RSV inoculation. In pathogen-free rats (Fig. 4, bottom), palivizumab administered either 24 h before (p = 0.94) or 72 h after (p = 0.18) the intranasal instillation of virus-free medium did not affect capsaicin-induced extravasation significantly.
Comparison of the inhibitory effect of palivizumab injected either 24 h before or 72 h after intranasal inoculation of RSV or virus-free medium in rats. Both treatment modalities inhibited significantly capsaicin-induced Evans blue extravasation in RSV-infected rats, although the magnitude of the inhibitory effect was larger when the antibody was administered before the virus. Palivizumab had no significant effect on vascular permeability in pathogen-free rats. ★★★p < 0.001 = significantly different from RSV-infected rats pretreated with vehicle.
DISCUSSION
These data show that the exaggerated neurogenic-mediated inflammatory reaction occurring in the respiratory tract of rats infected by RSV can be reduced by the prophylactic administration of RSVIG when the virus is inoculated in the nose but not when the virus is delivered directly into the lower airways. Palivizumab not only showed a much stronger inhibitory effect when given before intranasal inoculation, but it was also able to inhibit neurogenic inflammation after endotracheal inoculation of RSV. Furthermore, palivizumab inhibited neurogenic inflammation in RSV-infected airways when administered 72 h after intranasal inoculation of the virus. Finally, palivizumab had no direct effect on neurogenic inflammation in pathogen-free rats, confirming that its antiinflammatory effect is due to inhibition of viral entry into the airway epithelium.
RSVIG, polyclonal immune globulin enriched approximately 6-fold for RSV-specific neutralizing antibodies, was licensed in 1996 by the U.S. Food and Drug Administration for the prevention of serious lower respiratory tract infections caused by RSV. A large randomized double-blind placebo-controlled trial (PREVENT) showed a significant reduction (−41%, p = 0.047) in the rate of hospitalizations for RSV disease in premature infants and infants with bronchopulmonary dysplasia receiving monthly infusions of high-dose (750 mg/kg) RSVIG (9). This protective effect was dose-dependent, and low-dose RSVIG (150 mg/kg) was ineffective (22). In addition, RSVIG was ineffective when used alone in the treatment of children with confirmed RSV infection (23).
Palivizumab is a humanized IgG-1 MAb against the surface F glycoprotein of the virus, which mediates viral penetration into airway epithelial cells (19). In the cotton rat model, this antibody was shown to have inhibitory potency 50–100 times higher than RSVIG (19). The U.S. Food and Drug Administration licensed the product in 1998 after the pivotal IMpact-RSV trial revealed that the protective effect of palivizumab against RSV hospitalizations (−55%, p < 0.001) was greater than that previously observed with RSVIG (10). It is unclear whether this antibody can be effective for patients with established RSV infection (24).
Our data suggest that RSVIG attenuates RSV-induced inflammation by preventing the spread of the virus from the upper to the lower airways, but its protective effect is limited once significant viral titers are present in the lower airways. Palivizumab provides a much stronger protection against RSV-induced inflammation and may also have therapeutic activity when administered in high-risk patients early after the upper respiratory tract infection and before a widespread infection is established in the lungs. The difference between RSVIG and palivizumab may be related to the specific targeting of the viral F protein, determining a higher efficiency of the latter in opposing viral penetration into the airway epithelium. It is unlikely, however, that palivizumab can provide adequate protection once the virus has diffusely infected the lower airways and caused extensive epithelial damage with release of cytokines and other proinflammatory agents. This window between inoculum and established lower respiratory tract infection during which RSV antibodies are still protective may be affected by many species-specific variables, such as airway anatomy, specific and nonspecific immunologic response, and efficiency of viral replication.
The protective effect of RSV antibodies suggests that if the RSV infection remains limited to the upper airways or if viral penetration is inhibited in the early phase of lower airway infection, it is not associated with abnormal neurogenic inflammatory responses in the lower airways. Because neurogenic inflammation has been proposed as playing a role in the pathophysiology of airway obstruction (6), we speculate that palivizumab given before or in the early phase of RSV infection may reduce the risk of recurrent wheezing during the first decade of life associated with this infection (3). Randomized clinical trials looking at long-term respiratory morbidity in high-risk infants after palivizumab prophylaxis are necessary to investigate this hypothesis.
In summary, we have found that palivizumab, a humanized MAb against the F protein of RSV, inhibits the virus-induced potentiation of neurogenic-mediated inflammation in the airways of rats when administered 24 h before or 72 h after the virus. The prophylactic effect of RSVIG in this model is statistically significant, but its magnitude is much smaller than that with palivizumab. The administration of palivizumab to high-risk infants may limit the severity of the acute airway inflammation and may protect against subsequent lower respiratory tract illness.
Abbreviations
- MEM:
-
Eagle's minimum essential medium
- RSV:
-
respiratory syncytial virus
- TCID50:
-
50% tissue culture infective dose
- RSVIG:
-
polyclonal immune globulin enriched for RSV-neutralizing antibodies
References
Hall CB 1998 Respiratory syncytial virus. In: Feigin RD, Cherry JD (eds) Textbook of Pediatric Infectious Diseases. WB Saunders, Philadelphia, pp 2084–2111
Eigen H 1999 The RSV-asthma link: the emerging story. J Pediatr 135: S1–S50
Stein RT, Sherril D, Morgan WJ, Holberg CJ, Halonen M, Taussig LM, Wright AL, Martinez FD 1999 Respiratory syncytial virus in early life and risk of wheeze and allergy by age 13 years. Lancet 354: 541–545
Piedimonte G 1995 Tachykinin peptides, receptors, and peptidases in airway disease. Exp Lung Res 21: 809–834
Piedimonte G, Nadel JA 1996 Role of peptidases in airway defense mechanisms. In: Chretien J, Dusser D (eds) Airways and Environment: From Injury to Repair. Marcel Dekker, New York, pp 123–153
Barnes PJ 1992 Neurogenic inflammation and asthma. J Asthma 29: 165–180
Piedimonte G, Rodriguez MM, King KA, McLean S, Jiang X 1999 Respiratory syncytial virus upregulates expression of the substance P receptor in rat lungs. Am J Physiol 277: L831–L840
Piedimonte G, King KA, Perez Z, Jiang X 1999 Respiratory syncytial virus (RSV) causes long-term potentiation of neurogenic inflammation in rat airways. Am J Respir Crit Care Med 159: A245 abstr
The PREVENT Study Group. 1997 Reduction of respiratory syncytial virus hospitalization among premature infants and infants with bronchopulmonary dysplasia using respiratory syncytial virus immune globulin prophylaxis. Pediatrics 99: 93–99
The IMpact-RSV Study Group 1998 Palivizumab, a humanized respiratory syncytial virus monoclonal antibody, reduces hospitalization from respiratory syncytial virus infection in high-risk infants. Pediatrics 102: 531–537
Piedimonte G, Pickles RJ, Lehmann JR, McCarty D, Costa DL, Boucher RC 1997 Replication-deficient adenoviral vector for gene transfer potentiates airway neurogenic inflammation. Am J Respir Cell Mol Biol 16: 250–258
Routledge EG, McQuillin J, Samson ACR, Toms GL 1985 The development of monoclonal antibodies to respiratory syncytial virus and their use in diagnosis by indirect immunofluorescence. J Med Virol 15: 305–320
Piedimonte G, Nadel JA, Umeno E, McDonald DM 1990 Sendai virus infection potentiates neurogenic inflammation in the rat trachea. J Appl Physiol 68: 754–760
Piedimonte G, McDonald DM, Nadel JA 1990 Glucocorticoids inhibit neurogenic plasma extravasation and prevent virus-potentiated extravasation in the rat trachea. J Clin Invest 86: 1409–1415
Prince GA, Jenson AB, Horswood RL 1978 The pathogenesis of respiratory syncytial virus infection in cotton rats. Am J Pathol 93: 771–792
Saria A, Lundberg JM, Skofitsch G, Lembeck F 1983 Vascular protein leakage in various tissues induced by substance P, capsaicin, bradykinin, serotonin, histamine, and by antigen challenge. Naunyn Schmiedebergs Arch Pharmacol 324: 212–218
Holzer P 1991 Capsaicin: cellular targets, mechanisms of action, and selectivity for thin sensory neurons. Pharmacol Rev 43: 143–201
Siber GR, Leombruno D, Leszczynski J, McIver J, Bodkin D, Gonin R, Thompson CM, Walsh EE, Piedra PA, Hemming VG, Prince GA 1994 Comparison of antibody concentrations and protective activity of respiratory syncytial virus immune globulin and conventional immune globulin. J Infect Dis 169: 1368–1373
Johnson S, Oliver C, Prince GA, Hemming VG, Pfarr DS, Wang SC, Dormitzer M, O'Grady J, Koenig S, Tamura JK, Woods R, Bansal G, Couchenour D, Tsao E, Hall WC, Young JF 1997 Development of a humanized monoclonal antibody (MEDI-493) with potent in vitro and in vivo activity against respiratory syncytial virus (RSV). J Infect Dis 176: 1215–1224
Zar JH 1984 Two-Factor Analysis of Variance. Biostatistical Analysis. Prentice-Hall Inc, Englewood Cliffs NJ, pp 206–235
Wallenstein S, Zucker CL, Fleiss JL 1980 Some statistical methods useful in circulation research. Circ Res 47: 1–9
Groothuis JR, Simoes EAF, Levin MJ, Hall CB, Long CE, Rodriguez WJ, Arrobio J, Meissner HC, Fulton DR, Welliver RC, Tristram DA, Siber GR, Prince GA, Van Raden M, Hemming VG 1993 Prophylactic administration of respiratory syncytial virus immune globulin to high-risk infants and young children. N Engl J Med 329: 1524–1530
Rodriguez WJ, Gruber WC, Welliver RC, Groothuis JR, Simoes EAF, Meissner HC, Hemming VG, Levin MJ, Hall CB, Lepow ML, Rosas AJ, Robertsen C, Kramer AA 1997 Respiratory syncytial virus (RSV) immune globulin intravenous therapy for RSV lower respiratory tract infection in infants and young children at risk for severe RSV infections. Pediatrics 99: 454–461
Malley R, DeVincenzo J, Ramilo O, Dennehy PH, Meissner HC, Gruber WC, Sanchez PJ, Jafri H, Balsley J, Carlin D, Buckingham S, Vernacchio L, Ambrosino DM 1998 Reduction of respiratory syncytial virus (RSV) in tracheal aspirates in intubated infants by use of humanized monoclonal antibody to RSV F protein. J Infect Dis 178: 1555–1561
Acknowledgements
The authors thank Dr. Xiaobo Jiang for technical assistance.
Author information
Authors and Affiliations
Additional information
Supported in part by a grant from the National Institutes of Health (NHLBI HL-61007), the 1997 Career Investigator Award of the American Lung Association of Florida, and a research grant from MedImmune, Inc. to Dr. Giovanni Piedimonte.
Presented in part at the 1999 Annual Meeting, Pediatric Academic Societies, San Francisco, CA.
Rights and permissions
About this article
Cite this article
Piedimonte, G., King, K., Holmgren, N. et al. A Humanized Monoclonal Antibody against Respiratory Syncytial Virus (Palivizumab) Inhibits RSV-Induced Neurogenic-Mediated Inflammation in Rat Airways. Pediatr Res 47, 351–356 (2000). https://doi.org/10.1203/00006450-200003000-00011
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200003000-00011
This article is cited by
-
One-domain CD4 Fused to Human Anti-CD16 Antibody Domain Mediates Effective Killing of HIV-1-Infected Cells
Scientific Reports (2017)
-
Pathophysiological mechanisms for the respiratory syncytial virus-reactive airway disease link
Respiratory Research (2002)
-
An epidemiological study of respiratory syncytial virus associated hospitalizations in Denmark
Respiratory Research (2002)