Abstract
Viral respiratory infections cause acute bronchiolitis and physiologic dysfunction in human infants and in animals. It is possible that the pulmonary dysfunction is a consequence of the inflammatory cells that are recruited during viral illness. We hypothesized that blockade of intercellular adhesion molecule-1 (ICAM-1), a major cell adhesion molecule, would impede the ingress of leukocytes during viral infection and attenuate virus-induced pulmonary dysfunction. Adult male rats were inoculated with parainfluenza type 1 (Sendai) virus or sterile vehicle, and treated with blocking or nonblocking MAb specific for rat ICAM-1. Respiratory system resistance, oxygenation (Pao2), methacholine responsiveness, and bronchoalveolar lavage (BAL) leukocyte counts were measured in anesthetized, paralyzed, ventilated rats. Treatment with the blocking ICAM-1 antibody reduced virus-induced increases in BAL neutrophils and lymphocytes by 70% (p < 0.001), but did not affect BAL monocytes/macrophages. Peripheral blood leukocyte counts were elevated in anti-ICAM-1 blocking antibody-treated rats (p = 0.0003). Although virus-induced increases in resistance and decreases in Pao2 were not affected by anti-ICAM-1 treatment, there was a small but significant attenuation of virus-induced methacholine hyperresponsiveness (p = 0.02). We conclude that ICAM-1 has an important role in neutrophil and lymphocyte infiltration during respiratory viral illness, and that virus-induced changes in pulmonary physiology are not related directly to the numbers of neutrophils and lymphocytes that migrate to the air spaces during infection.
Similar content being viewed by others
Main
Viral bronchiolitis in human infants is caused most commonly by respiratory syncytial virus and parainfluenza viruses, is associated with neutrophilic leukocytosis in the air spaces, and is manifested clinically as airway obstruction, patchy interstitial pneumonia, hyperinflation, and hypoxia (1–3). Rats infected with parainfluenza type 1 (Sendai) virus exhibit analogous pathology of erosive bronchiolitis and patchy interstitial pneumonia with neutrophilic leukocyte infiltration, and also exhibit airway obstruction, elevated residual lung volume, altered pulmonary gas exchange, and airway hyperresponsiveness (4–6). This animal model therefore is of value for investigations of the mechanisms of virus-induced inflammation and the resulting alterations in pulmonary physiology.
It is not known to what extent that intercellular adhesion molecule (ICAM)-1 mediates inflammatory cell migration during the multiple days of acute respiratory viral illness, but several models of acute lung injury have demonstrated that in the hours following an insult, blockade of ICAM-1 reduces both the neutrophil migration and the severity of lung injury (7–10). Rats treated with dexamethasone or with the immune modulator imiquimod during Sendai virus infection have reduced bronchoalveolar inflammatory cell numbers and attenuated virus-induced pulmonary dysfunction (11, 12), consistent with the notion that the pulmonary dysfunction is related to the inflammatory process. Because high levels of ICAM-1 are expressed on the basal layers of tracheal epithelium during the inflammatory cell influx in rats acutely infected with Sendai virus (13), we hypothesized that ICAM-1 may also have a prominent role in the inflammation associated with viral bronchiolitis.
The purposes of this study were first, to determine the extent to which leukocyte migration during respiratory viral illness is dependent on ICAM-1, and second, to determine whether reducing leukocyte migration via adhesion molecule blockade can attenuate virus-induced pulmonary dysfunction.
METHODS
Animals.
All methods and procedures were approved by the Animal Care and Use Committee of the University of Wisconsin. Adult male specific-pathogen-free Sprague-Dawley-derived rats (CD strain; Charles River Breeding Laboratories, Raleigh, NC, U.S.A.), weighing 230–310 g, were used for these experiments. All animals were allowed food and water ad libitum.
Viral procedures.
Rats were inoculated with parainfluenza type 1 (Sendai) virus strain P3193 using an aerosol exposure apparatus (Glas-Col, Terre Haute, IN, U.S.A.) as described previously (11, 14). Control rats were sham-inoculated with sterile chorioallantoic fluid in a similar manner. Animals were housed in filter-top cages after inoculation, and virus and control groups were studied at different times to ensure that the control group was not exposed to the pathogen.
Pulmonary physiology.
Cannulae were placed in the trachea, femoral vein and femoral artery of each rat after anesthesia was induced with urethane (1.2 g/kg i.p.; Sigma Chemical Co., St. Louis, MO, U.S.A.). Rats were placed in a constant-pressure rodent plethysmograph, treated with propranolol (2 mg/kg i.v.; Sigma Chemical Co., St. Louis, MO, U.S.A.) to inhibit adrenergic effects during methacholine challenges, and then paralyzed with succinylcholine chloride (4 mg/kg i.v. initially and 2 mg/kg thereafter as needed; Sigma Chemical Co., St. Louis, MO, U.S.A.). Rats were ventilated mechanically at 80 breaths/min and positive end-expiratory pressure of 0.25 kPa, with the tidal volume adjusted to maintain a normal arterial Pco2 of 4.7–6.0 kPa. Lungs were inflated to 2.9 kPa pressure each minute to prevent atelectasis, and accumulated secretions were removed from the airways by suctioning as necessary. Arterial blood was sampled after 10 min of mechanical ventilation and measured (model 1306 automated blood gas analyzer, Instrumentation Laboratory, Lexington, MA, U.S.A.) at 37°C on a O.5 mL sample collected anaerobically into a syringe containing dried heparin and placed in ice pending analysis. An equal volume of saline was injected back into the rat. Blood gas values were adjusted as necessary if the rat's rectal temperature was different from 37°C. For data analysis, Pao2 measurements were excluded if the Paco2 was outside of the 4.7–6.0 kPa range.
Resistance was measured by the isovolume method at 50% tidal volume (Model 6 Pulmonary Mechanics Analyzer, Buxco Electronics, Sharon, CT, U.S.A.), using inflation pressure measured at the tracheal cannula, and flow and volume obtained from the plethysmograph transducer signal. Pressure and flow signals were in phase to at least 7 Hz under test conditions. Adiabatic/isothermal transients were negligible in the range of flow rates encountered in these studies. Respiratory system resistance was obtained from the computed resistance by subtracting the resistance of the tracheal cannula and its connector.
For evaluation of airway responsiveness, methacholine Cl (Sigma Chemical Co., St. Louis, MO, U.S.A.) was injected as 1 mL/kg of increasing concentrations of the agent, followed by a flush of 0.3 mL saline, both completed in 5 s. Responses to i.v. methacholine were recorded as the change in resistance after administration of the agent. Sensitivity to methacholine was determined as the log dose (nmol/kg) required to increase resistance by 20 Pa mL−1 s by interpolation of the dose-response curve.
Leukocyte counts.
Following physiology measurements, rats were killed by exsanguination and air embolus. The thoracic cavity was then exposed, and the lungs were inflated to total lung capacity with cold Hanks balanced salt solution (without calcium and magnesium); the lavage fluid was drained by gravity, and the process was repeated a total of 5 times. The bronchoalveolar lavage (BAL) fluid was centrifuged and the cell pellet was resuspended in 1 mL of buffer. Blood samples for the peripheral leukocyte counts were obtained from the arterial cannula at the same time as the blood gas sample, and placed into EDTA polyethylene tubes. Total cell counts were determined with a Hemo-W cell counter (Coulter Electronics, Hialeah, FL, U.S.A.). Cytocentrifuge (Cytospin, Shandon Lipshaw Inc., Pittsburgh, PA, U.S.A.) slides were prepared and stained with Diff-Quik (Baxter Healthcare Corp., Miami, FL, U.S.A.); the differential leukocyte counts were determined from 200 stained BAL cells and from 100 peripheral blood leukocytes. Total neutrophils, macrophages/monocytes and lymphocytes were computed from the total leukocyte count and the percentage of each cell type from the differential cell count for each sample.
Monoclonal antibodies.
MAb specific for rat ICAM-1 were obtained from murine hybridoma clones 1A29 and 10A57. The 1A29 MAb blocks interaction between ICAM-1 and its ligand, while MAb 10A57 binds to ICAM-1 at a nonblocking site (15). BALB/c mice were injected with 2 × 106 viable hybridoma cells intraperitoneally, and ascites fluid was harvested after 8 to 20 d. Anti-ICAM-1 IgG antibody was then purified from ascites fluid using an ImmunoPure (A/G) IgG purification column (Pierce Chemical Co., Rockford, IL, U.S.A.).
Study design.
Rats were inoculated with virus or sham inoculated with sterile vehicle. Mouse hybridoma anti-rat ICAM-1 antibody (5 mg/kg) or saline was injected i.p. daily, starting the day before inoculation. Pulmonary physiology, peripheral blood leukocyte counts, and BAL leukocytes were evaluated at postinoculation d 5, 6 or 7; injections of antibodies were not administered on the day of the terminal study. The experiment consisted of 5 study groups: viral inoculation, saline treatment (V-Sal); viral inoculation, anti-ICAM-1 blocking antibody treatment (V-BA); viral inoculation, anti-ICAM-1 nonblocking antibody treatment (V-NB); sham control inoculation, saline treatment (C-Sal); and sham inoculation, anti-ICAM-1 blocking antibody treatment (C-BA).
Data analysis.
Systat statistical software (v 7.0; SPSS, Inc., Chicago, IL, U.S.A.) was used for data analysis. For peripheral leukocyte counts, 2-way ANOVA was used, using inoculation and treatment variables as main effects. For other variables 2-way ANOVA had a significant interactive effect between the inoculation and treatment variables, and data were analyzed instead using one-way ANOVA of the 5 study groups. For significant ANOVA, planned post hoc comparisons were conducted with contrasts of the groups of interest. The groups of virus-infected rats treated with saline or with nonblocking anti-ICAM-1 antibody were identical for all variables, and thus were contrasted together with the virus/blocking anti-ICAM-1 antibody group to test for treatment effect. For comparisons of groups with unequal variances, log-transformed data or a separate-variance ANOVA model was used. Data obtained on d 5, 6, or 7 post-inoculation were pooled for all variables except BAL lymphocytes, which increased progressively in infected rats over those study days; the other variables exhibited no significant day-related differences. For BAL lymphocytes a randomized block ANOVA model was used to allow for the time-related changes in lymphocyte migration.
RESULTS
Leukocytes.
Rats infected with Sendai virus had significant increases in numbers of macrophages/monocytes, neutrophils, and lymphocytes in their BAL compared with noninfected rats (p < 0.0001;Fig. 1). Eosinophils were rare in the BAL of all the study groups. Compared with virus-infected rats that were treated with saline or with nonblocking antibody, the virus-infected rats that were treated with blocking antibody to ICAM-1 had marked reductions in the numbers of BAL neutrophils (p = 0.0001) and also in the numbers of BAL lymphocytes (p = 0.0004), but no significant difference in the number of BAL macrophages/monocytes (Fig. 1). Overall, the blocking anti-ICAM-1 antibody reduced both neutrophils and lymphocytes in the BAL by about 70% in virus-infected rats. Numbers of BAL leukocytes were not altered significantly by the nonblocking anti-ICAM-1 antibody in infected rats nor by the blocking anti-ICAM-1 antibody in noninfected rats (Fig. 1). Peripheral blood leukocyte counts were elevated significantly (p = 0.0003) in rats treated with the blocking anti-ICAM-1 antibody, but were not significantly changed by either viral infection or by the nonblocking antibody (Fig. 2). Both neutrophils and mononuclear cells contributed to the increase in peripheral blood leukocyte counts in rats treated with the blocking anti-ICAM-1 antibody (p < 0.0001).
Leukocytes obtained via bronchoalveolar lavage of rats 5–7 d after viral inoculation (V) and of noninfected controls (C). Each symbol represents one rat, and bars indicate group medians for pooled time points. Treatments: saline (Sal), blocking anti-ICAM-1 antibody (BA), nonblocking anti-ICAM-1 antibody (NB). *Significantly different from infected rats treated with saline or nonblocking antibody.
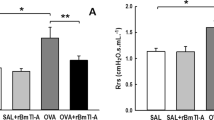
Total leukocyte counts in peripheral blood of rats 5–7 d after viral inoculation (V) and in noninfected controls (C). Each symbol represents one rat, and bars indicate group medians. The insert shows ANOVA least squares mean ± SE for the main effects of the three treatments. Treatments: saline (Sal), blocking anti-ICAM-1 antibody (BA), nonblocking anti-ICAM-1 antibody (NB). *Leukocyte counts were significantly elevated in rats treated with blocking anti-ICAM-1 antibody compared with those receiving nonblocking antibody or saline.
Physiology.
Viral illness produced changes in respiratory system resistance (p < 0.0001;Fig. 3) and in eucapnic Pao2 (p < 0.0001;Fig. 4) that were consistent with airway obstruction and alterations in gas exchange. These virus-induced changes in pulmonary physiology were not affected by treatment with anti-ICAM-1 antibody (Figs. 3 and 4). Airway responsiveness to methacholine was increased in virus-infected rats compared with noninfected rats (p = 0.001;Fig. 5). Treatment with the blocking anti-ICAM-1 antibody resulted in a small but significant attenuation of virus-induced hyperresponsiveness (p = 0.02, Fig. 5).
Pulmonary resistance in rats 5–7 d after viral inoculation (V) and in noninfected controls (C). Each symbol represents one rat, and bars indicate group medians. Treatments: saline (Sal), blocking anti-ICAM-1 antibody (BA), nonblocking anti-ICAM-1 antibody (NB). Resistance was significantly higher in V vs C, but there were no significant differences due to antibody treatments.
Eucapnic arterial Po2 in rats 5–7 d after viral inoculation (V) and in noninfected controls (C). Each symbol represents one rat, and bars indicate group medians. Treatments: saline (Sal), blocking anti-ICAM-1 antibody (BA), nonblocking anti-ICAM-1 antibody (NB). Arterial Po2 was significantly lower in V vs C, but there were no significant differences due to antibody treatments.
Responsiveness to i.v. methacholine, expressed as the log dose associated with an increase in pulmonary resistance of 20 Pa mL−1 s (PD20) in rats 5–7 d after viral inoculation (V) and in noninfected controls (C). Each symbol represents one rat, and bars indicate group medians. Treatments: saline (Sal), blocking anti-ICAM-1 antibody (BA), nonblocking anti-ICAM-1 antibody (NB). Virus-infected rats were significantly more responsive to methacholine compared with noninfected rats; *significantly different from infected rats treated with saline or nonblocking antibody.
DISCUSSION
ICAM-1 expression is induced on pulmonary epithelium and vascular endothelium during infections with viruses, bacteria, yeasts, or Pneumocystis carinii, predominantly as a result of local production of IFN-γ, TNFα or IL-1(13, 16–24). That β2-integrin-mediated endothelial adhesion is important for neutrophil and monocyte emigration from the circulation during infections was illustrated definitively by observations in patients having a genetic deficiency in β2-integrin expression (25). It would seem logical that ICAM-1/β2-integrin interactions might therefore play a prominent role in leukocyte trafficking during infections. Animal models of Pseudomonas aeruginosa pneumonia have confirmed that reduced function of ICAM-1 or β2-integrin (CD18) impairs neutrophil emigration at 4–6 h after infection (26–28). However, when P. aeruginosa is reintroduced to the same site a week later, a greater proportion of neutrophil emigration occurs via pathways independent of β2-integrins (26); similarly, ICAM-1/β2-integrin interactions are not important for neutrophil emigration during the first 6 h of pneumonia due to Streptococcus pneumoniae (27). Thus, the role of ICAM-1 in neutrophil trafficking may vary with both the nature of the infectious agent and the time frame of the host response to the infection.
In addition to its role in neutrophil emigration, ICAM-1 also may be involved in the effector function of neutrophils. Adherence to pulmonary endothelial ICAM-1 is associated with a respiratory burst in neutrophils during endotoxin infusion (29). Neutrophils are capable of injuring epithelial cells, most effectively during firm adherence (30). Pulmonary epithelial cells infected with virus exhibit increased neutrophil adherence that is due in part to ICAM-1 interactions (21, 31), and the presence of neutrophils enhances virus-induced epithelial damage and detachment (31). Thus it is plausible that neutrophil interactions with ICAM-1 during respiratory viral infections could contribute to neutrophil activation and tissue injury as well as to neutrophil emigration, and that interfering with these interactions might attenuate the pulmonary physiologic dysfunction that accompanies bronchiolitis.
The current study was designed to address the potential role of ICAM-1 during acute viral bronchiolitis. The rats were evaluated at 5–7 d after inoculation, when physiologic dysfunction is present, numbers of neutrophils are peaking, lymphocytes are beginning to increase in the airspaces, and lung viral titers are decreasing. The results of this study indicate that ICAM-1-dependent processes are involved prominently in virus-induced recruitment of neutrophils and lymphocytes to the airways and alveoli. Peripheral blood leukocyte counts were concomitantly elevated, confirming that leukopenia was not the reason for reduced leukocyte migration to the airspace. The leukocytosis is consistent with previous observations that the MAb used is able to block cell adhesion via ICAM-1-dependent ligand interactions (15, 32), as well as with the observation of peripheral leukocytosis in mice having an ICAM-1 deficiency (33). Despite these significant reductions in inflammatory cell recruitment into the lungs, virus-induced alterations in pulmonary physiology developed unimpeded, except for a small attenuation of airway hyperresponsiveness.
The absence of a protective effect on pulmonary dysfunction despite a substantial reduction in the numbers of neutrophils in the airspace suggests that factors other than neutrophilic inflammation must have been responsible for the functional changes. We observed previously in this rat model that systemic glucocorticoid treatment during acute bronchiolitis attenuated both inflammation and airway dysfunction, but also caused an elevation of lung viral titers, suggesting that the inflammatory response, and not direct viral injury, is responsible for the functional changes (11). Although it is possible that the reduced numbers of neutrophils and lymphocytes in the BAL were not accompanied by parallel decreases in parenchymal leukocytes, we think it unlikely that the anti-ICAM-1 treatment caused a marked dissociation between parenchymal and air space leukocyte numbers. Observations of spacial associations between allergen-induced ICAM-1 expression and subepithelial accumulation of leukocytes (34) suggest that ICAM-1/β2-integrin interactions may serve to retain leukocytes in the parenchyma; if true, ICAM-1 blockade should have reduced, not increased, parenchymal leukocytes in the current study. Parenchymal sequestering of a large number of cells, or extensive consolidation of airspaces, likely would have been apparent as worsening lung mechanics and gas exchange. Also, the lack of an effect of anti-ICAM-1 treatment on numbers of macrophage/monocytes in BAL makes it unlikely that the reduced numbers of neutrophils and lymphocytes could be explained by increased areas of consolidation that could not be reached by the lavage fluid. Because the numbers of pulmonary macrophages and monocytes were increased more than other cell types during viral illness, and were not reduced significantly by anti-ICAM-1 treatment, a possible explanation of the study results is that macrophages and/or monocytes are the effector cells with respect to the physiologic dysfunction that develops during the 1st week of parainfluenza-1 bronchiolitis in this model.
These experimental results comprise one of four sets of observations in this model that have examined the relationship between virus-induced pulmonary inflammation and physiology. In previous experiments, dexamethasone treatment in virus infected rats produced a significant reduction in BAL neutrophils, macrophages/monocytes, and lymphocytes, and the virus-induced changes in pulmonary physiology were attenuated markedly, although not prevented entirely (11). Similarly, treatment with imiquimod, an immunomodulator that enhances host antiviral responses, attenuated peak viral titers, and reduced virus-induced BAL leukocytes, airway obstruction, and hypoxia (12). Treatment with a more selective inhibitor of granulocyte chemotaxis and oxygen radical formation (a 21-aminosteroid) had no effect on the ingress of any of these cell types nor on virus-induced alterations in pulmonary resistance or compliance; however, airway hyperresponsiveness was significantly attenuated (35), consistent with the concept that oxidative inflammatory cell products may affect airway responsiveness. In the current study, reductions in the numbers of neutrophils and lymphocytes had a similar effect on virus-induced airway hyperresponsiveness, consistent with the dexamethasone and 21-amino steroid studies, and further supporting a potential link between inflammatory cells and airway hyperresponsiveness. Hyperresponsiveness during viral illness arises from a number of neural and nonneural mechanisms (6, 36), and a partial protection from hyperresponsiveness could be explained by a treatment effect on one component but not others. The relatively greater protective effect of dexamethasone compared with anti-ICAM-1 or aminosteroid treatments in this model may relate to the marked reduction in numbers of all types of inflammatory cells, as well as glucocorticoid effects on edema formation.
In summary, viral bronchiolitis in rats is characterized by an acute cellular inflammatory response in which ICAM-1-dependent processes are important for neutrophil and lymphocyte migration, but are not necessary for macrophage/monocyte trafficking. Selective inhibition of neutrophil and lymphocyte migration during acute viral illness attenuates slightly the virus-induced airway hyperresponsiveness, but does not alter the development of airway obstruction and hypoxia associated with viral bronchiolitis in this animal model.
Abbreviations
- ICAM-1:
-
intercellular adhesion molecule-1
- BAL:
-
bronchoalveolar lavage
References
Wohl ME, Chernick V 1978 State of the art: bronchiolitis. Am Rev Respir Dis 118: 759–781
Everard ML, Swarbrick A, Wrightham M, McIntyre J, Dunkley C, James PD, Sewell HF, Milner AD 1994 Analysis of cells obtained by bronchial lavage of infants with respiratory syncytial virus infection. Arch Dis Child 71: 428–432
Panitch HB, Callahan CWJ, Schidlow DV 1993 Bronchiolitis in children. Clin Chest Med 14: 715–731
Castleman WL 1983 Respiratory tract lesions in weanling outbred rats infected with Sendai virus. Am J Vet Res 44: 1024–1031
Castleman WL, Brundage-Anguish LJ, Kreitzer L, Neuenschwander SB 1987 Pathogenesis of bronchiolitis and pneumonia induced in neonatal and weanling rats by parainfluenza (Sendai) virus. Am J Pathol 129: 277–286
Sorkness R, Clough JJ, Castleman WL, Lemanske RF Jr 1994 Virus-induced airway obstruction and parasympathetic hyperresponsiveness in adult rats. Am J Respir Crit Care Med 150: 28–34
Mulligan MS, Wilson GP, Todd RF, Smith CW, Anderson DC, Varani J, Issekutz TB, Miyasaka M, Tamatani T 1993 Role of beta 1, beta 2 integrins and ICAM-1 in lung injury after deposition of IgG and IgA immune complexes. J Immunol 150: 2407–2417
Barton RW, Rothlein R, Ksiazek J, Kennedy C 1989 The effect of anti-intercellular adhesion molecule-1 on phorbol-ester-induced rabbit lung inflammation. J Immunol 143: 1278–1282
Nagase T, Ohga E, Sudo E, Katayama H, Uejima Y, Matsuse, Fukuchi Y 1996 Intercellular adhesion molecule-1 mediates acid aspiration-induced lung injury. Am J Respir Crit Care Med 154: 504–510
Doerschuk CM, Quinlan WM, Doyle NA, Bullard DC, Vestweber D, Jones ML, Takei F, Ward PA, Beaudet AL 1996 The role of P-selectin and ICAM-1 in acute lung injury as determined using blocking antibodies and mutant mice. J Immunol 157: 4609–4614
Mehta H, Sorkness R, Kaplan MR, Castleman WL, Lemanske RF Jr 1997 Effects of dexamethasone on acute virus-induced airway dysfunction in adult rats. Pediatr Res 41: 872–877
Stokes JR, Sorkness RL, Kaplan MR, Castleman WL, Tomai MA, Miller RL, Lemanske RF Jr 1998 Attenuation of virus-induced airway dysfunction in rats treated with imiquimod. Eur Respir J 11: 324–329
McWilliam AS, Marsh AM, Holt PG 1997 Inflammatory infiltration of the upper airway epithelium during Sendai virus infection: involvement of epithelial dendritic cells. J Virol 71: 226–236
Sorkness R, Clough J, Lemanske RF Jr 1994 Effects of airway parasympathetic tone on responses to intravenous agonists in rats. J Appl Physiol 77: 2698–2702
Tamatani T, Miyasaka M 1990 Identification of monoclonal antibodies reactive with the rat homolog of ICAM-1, and evidence for a differential involvement of ICAM-1 in the adherence of resting versus activated lymphocytes to high endothelial cells. Int Immunol 2: 165–171
Stark JM, Amin RS, Trapnell BC 1996 Infection of A549 cells with a recombinant adenovirus vector induces ICAM-1 expression and increased CD-18-dependent adhesion of activated neutrophils. Hum Gene Ther 7: 1669–1681
Stark JM, Godding V, Sedgwick JB, Busse WW 1996 Respiratory syncytial virus infection enhances neutrophil and eosinophil adhesion to cultured respiratory epithelial cells. J Immunol 156: 4774–4782
Izzo AA, Lovchik JA, Lipscomb MF 1998 T and B cell independence of endothelial cell adhesion molecule expression in pulmonary granulomatous inflammation. Am J Respir Cell Mol Biol 19: 588–597
Yu ML, Limper AH 1997 Pneumocystis carinii induces ICAM-1 expression in lung epithelial cells through a TNF-alpha-mediated mechanism. Am J Physiol 273: L1103–L1111
Ibrahim L, Dominguez M, Yacoub M 1993 Primary human adult lung epithelial cells in vitro: response to interferon-gamma and cytomegalovirus. Immunology 79: 119–124
Tosi MF, Stark JM, Hamedani A, Smith CW, Gruenert DC, Huang YT 1992 Intercellular adhesion molecule-1 (ICAM-1)-dependent and ICAM-1-independent adhesive interactions between polymorphonuclear leukocytes and human airway epithelial cells infected with parainfluenza virus type 2. J Immunol 149: 3345–3349
Mulligan MS, Vaporciyan AA, Miyasaka M, Tamatani T, Ward PA 1993 Tumor necrosis factor alpha regulates in vivo intrapulmonary expression of ICAM-1. Am J Pathol 142: 1739–1749
Beck-Schimmer B, Schimmer RC, Warner RL, Schmal H, Nordblom G, Flory CM, Lesch ME, Friedl HP, Schrier DJ, Ward PA 1997 Expression of lung vascular and airway ICAM-1 after exposure to bacterial lipopolysaccharide. Am J Respir Cell Mol Biol 17: 344–352
Patel JA, Kunimoto M, Sim TC, Garofalo R, Eliott T, Baron S, Ruuskanen O, Chonmaitree T, Ogra PL, Schmalstieg F 1995 Interleukin-1 alpha mediates the enhanced expression of intercellular adhesion molecule-1 in pulmonary epithelial cells infected with respiratory syncytial virus. Am J Respir Cell Mol Biol 13: 602–609
Anderson DC, Springer TA 1987 Leukocyte adhesion deficiency: an inherited defect in the Mac-1, LFA-1, and p 150:95 glycoproteins. Ann Rev Med 38: 175–194
Kumasaka T, Doyle NA, Quinlan WM, Graham L, Doerschuk CM 1996 Role of CD 11/CD 18 in neutrophil emigration during acute and recurrent Pseudomonas aeruginosa-induced pneumonia in rabbits. Am J Pathol 148: 1297–1305
Mizgerd JP, Horwitz BH, Quillen HC, Scott ML, Doerschuk CM 1999 Effects of CD18 deficiency on the emigration of murine neutrophils during pneumonia. J Immunol 163: 995–999
Qin L, Quinlan WM, Doyle NA, Graham L, Sligh JE, Takei F, Beaudet AL, Doerschuk CM 1996 The roles of CD11/CD18 and ICAM-1 in acute Pseudomonas aeruginosa-induced pneumonia in mice. J Immunol 157: 5016–5021
Minamiya Y, Motoyama S, Kitamura M, Saito S, Terada K, Ogawa J 1998 The requirement of intercellular adhesion molecule-1 for neutrophil respiratory burst in the pulmonary circulation of rats infused with endotoxin. Am J Respir Crit Care Med 158: 635–642
Simon RH, DeHart PD, Todd RF 1986 Neutrophil-induced injury of rat pulmonary alveolar epithelial cells. J Clin Invest 78: 1375–1386
Wang SZ, Xu H, Wraith A, Bowden JJ, Alpers JH, Forsyth KD 1998 Neutrophils induce damage to respiratory epithelial cells infected with respiratory syncytial virus. Eur Respir J 12: 612–618
Nishio K, Suzuki Y, Aoki T, Suzuki K, Miyata A, Sato N, Naoki K, Kudo H, Tsumura H, Serizawa H, Morooka S, Ishimura Y, Suematsu, Yamaguchi K 1998 Differential contribution of various adhesion molecules to leukocyte kinetics in pulmonary microvessels of hyperoxia-exposed rat lungs. Am J Respir Crit Care Med 157: 599–609
Sligh JEJ, Ballantyne CM, Rich SS, Hawkins HK, Smith CW, Bradley A, Beaudet AL 1993 Inflammatory and immune responses are impaired in mice deficient in intercellular adhesion molecule 1. Proc Nat Acad Sci USA 90: 8529–8533
Wegner CD, Gundel RH, Reilly P, Haynes N, Letts LG, Rothlein R 1990 Intercellular adhesion molecule-1 (ICAM-1) in the pathogenesis of asthma. Science 247: 456–459
Sorkness R, Lemanske RF Jr 1996 Attenuation of airway hyperresponsiveness during acute viral infection using the 21-aminosteroid U-83836E in rats. Pulm Pharmacol 9: 219–222
Folkerts G, Busse WW, Nijkamp FP, Sorkness R, Gern JE 1998 State of the art. Am J Respir Crit Care Med 157: 1708–1720
Acknowledgements
The authors thank Dr. William Castleman for preparing the virus used for these studies, and the Pulmonary Diagnostic Services laboratory at University of Wisconsin Hospitals and Clinics for blood gas measurements.
Author information
Authors and Affiliations
Additional information
Supported by National Institutes of Health AI-34891; Allen & Hanburys Respiratory Institute Allergy Fellowship Award (H. Mehta).
Rights and permissions
About this article
Cite this article
Sorkness, R., Mehta, H., Kaplan, M. et al. Effect of ICAM-1 Blockade on Lung Inflammation and Physiology During Acute Viral Bronchiolitis in Rats. Pediatr Res 47, 819–824 (2000). https://doi.org/10.1203/00006450-200006000-00023
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200006000-00023
This article is cited by
-
The role of the endothelium in asthma and chronic obstructive pulmonary disease (COPD)
Respiratory Research (2017)