Abstract
Inflammatory mediators are implicated in the pathogenesis of ischemic injury in immature brain. The phosphodiesterase inhibitor pentoxifylline inhibits production of tumor necrosis factor-α and platelet-activating factor. We hypothesized that pentoxifylline treatment would attenuate hypoxic-ischemic brain injury in immature rats. Seven-day-old rats (n = 79) underwent right carotid ligation, followed by hypoxia (FiO2 = 0.08). Rats received pentoxifylline immediately before and again after hypoxia (two doses, 25–150 mg/kg/dose, n = 34), or vehicle (n = 27). In separate experiments, rats received pentoxifylline treatment (40 mg/kg/dose, n = 8), or vehicle (n = 10) immediately and again 3 h after hypoxia-ischemia. Severity of injury was assessed 5 d later by visual evaluation of ipsilateral hemisphere infarction and by measurement of bilateral hemispheric cross-sectional areas. Pentoxifylline pretreatment reduced the incidence of liquefactive cerebral infarction, from 75% in controls to 10% with pentoxifylline, 40 mg/kg/dose (p < 0.001, χ2 trend test). Quantification of hemispheric areas confirmed these findings. In contrast, posthypoxic-ischemic treatment with pentoxifylline resulted in only a modest reduction in cortical damage, without an overall reduction in incidence of infarction. Phosphodiesterase inhibition may be an effective strategy to use to decrease the severity of neonatal hypoxic-ischemic brain injury. Pretreatment regimens could be clinically relevant in settings in which an increased risk of cerebral ischemia can be anticipated, such as in infants undergoing surgery to correct congenital heart disease.
Similar content being viewed by others
Main
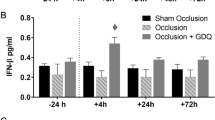
The pathogenesis of perinatal cerebral hypoxic-ischemic injury has been extensively examined by using models of carotid ligation and subsequent exposure to moderate hypoxia in immature rats. Many interrelated mechanisms—including excessive stimulation of excitatory amino acid receptors, intracellular calcium accumulation, lipid peroxidation, and free radical generation—may play a role in the evolution of hypoxic-ischemic injury (1, 2). Recent evidence implicates inflammatory cells, cytokines (e.g., TNF-α and IL-1β), and the lipid mediator platelet-activating factor as mediators of hypoxic-ischemic injury in immature brain. Neutrophils (3) and activated macrophages and microglia accumulate (4, 5), and TNF-α and IL-1β protein and gene expression increase within 6 h after a cerebral hypoxic-ischemic insult in rats at postnatal d 7 (P7) (6, 7). Systemic administration of either a pharmacologic antagonist of the IL-1 receptor (8) or a platelet-activating factor receptor antagonist (9) attenuates neonatal cerebral hypoxic-ischemic injury in P7 rats.
The alkylxanthine phosphodiesterase inhibitor pentoxifylline [3,7-dimethyl-1-(5-oxohexyl)-xanthine]—which improves red cell deformability, decreases platelet and red cell aggregation and lowers fibrinogen levels and plasma viscosity (10)—is already used clinically for treatment of intermittent claudication (11, 12). Recently, attention has focused on the influence of pentoxifylline on mononuclear phagocyte, neutrophil, and endothelial activation and production of inflammatory and thrombogenic mediators. In vitro, pentoxifylline inhibits gene transcription and production of TNF-α by mononuclear phagocytes (13) and microglia (14), and inhibits tissue factor gene transcription and production by activated endothelium (15, 16). In addition, pentoxifylline inhibits production of platelet-activating factor in experimental ischemia-reperfusion injury (17) and inhibits activation of neutrophils by inflammatory mediators such as TNF-α (18–20). Pentoxifylline penetrates the blood-brain barrier rapidly and efficiently after systemic administration (21). In vivo, systemically administered pentoxifylline attenuates brain TNF-α production after closed head injury in rats (22) or brain irradiation in mice (23), and it attenuates experimental allergic encephalomyelitis in rats (24).
The multiple potentially beneficial vascular and anti-inflammatory activities of pentoxifylline led several investigators to test the neuroprotective efficacy of pentoxifylline in mature animal models of cerebral ischemia; results were inconsistent (25–29). None of those reports addressed the efficacy of pentoxifylline in an immature animal model of cerebral ischemic injury. Reports of enhanced effects of pentoxifylline on neonatal neutrophil function in vitro (30, 31), as well as demonstration of neuroprotective efficacy of other anti-inflammatory strategies in immature brain (8, 9, 32), prompted us to test the hypothesis that pentoxifylline would attenuate neonatal hypoxic-ischemic brain damage. We used an in vivo model of neonatal cerebral hypoxia-ischemia with subsequent reperfusion, elicited by unilateral carotid ligation followed by timed exposure to moderate hypoxia in P7 rats. Precise correlations with human brain development are difficult; however, brains of P7 rats are similar to third-trimester human fetuses (and thus premature or full-term human newborns) in terms of cellular proliferation, cortical organization, synapse number, neurotransmitter synthetic enzymes, and electrophysiology (33–35).
We evaluated the neuroprotective efficacy of pentoxifylline by comparing the incidence of liquefactive necrosis and by measuring regional cross-sectional areas in drug-treated and control animals. Clinically, neuroprotective drugs might be used either prophylactically, in patients at known risk of hypoxic-ischemic brain injury (i.e., infants undergoing cardiopulmonary bypass for treatment of congenital heart disease) or as post-insult “rescue” therapy (e.g., after acute perinatal asphyxia). In these experiments, we tested the neuroprotective efficacy of pentoxifylline in both prophylactic and rescue regimens. Our results demonstrated that pentoxifylline treatment initiated either before or immediately after cerebral hypoxia-ischemia attenuated brain damage in P7 rats.
METHODS
Hypoxia-ischemia.
In methoxyflurane-anesthetized P7 Sprague-Dawley rats (Charles River Laboratories), the right carotid artery was isolated and double-ligated (<5 min procedure); 1–2 h later, animals were exposed to 8% oxygen (balance nitrogen) for either 3.25 h (first three experiments) or 2.75 h (subsequent two experiments) in glass chambers, partially submerged in a water bath (temperature maintained at 38°C). The hypoxia duration was shortened in two experiments, because in both litters, the mean animal weight was significantly higher than the first three litters [mean (±SD) weight on P7: first three litters 11.8 (±1.2) g; subsequent two litters 15.2 (±1.3) g;p = 0.0001, t test]. Our strategy to compensate for increased animal weight was to reduce the duration of hypoxia exposure, to attempt to maintain a comparable severity of injury in control animals. This approach was based on a report that the severity of hypoxic-ischemic brain injury among P7 rats varies in direct proportion to weight;i.e., the higher the body weight, the greater the severity of brain injury (36). Experiments that used different hypoxia durations were analyzed separately (Data Analysis and Results). In two separate experiments, to test the efficacy of posthypoxic-ischemic pentoxifylline treatment, rats underwent right carotid ligation followed by 2.75 h hypoxia (8% O2) exposure. For 1 h after the end of hypoxia, animals were housed in a warm air incubator (ambient temperature: 35–36°C), before they were returned to the dam.
At higher doses (200 mg/kg), pentoxifylline can induce mild hypothermia (about 2°C core temperature reduction) in mice (37). Because hypothermia can attenuate cerebral ischemic injury, intrahypoxic skin temperature was measured in a subset of pretreated rats, and esophageal temperature was monitored for 8 h after hypoxia in rats from four experiments (40 or 75 mg/kg/dose) (YSI thermometer 43TA with probe 554, Yellow Spring Instruments, Yellow Spring, OH).
For evaluation of histopathologic outcome, rats were decapitated and brains rapidly dissected and frozen under powdered dry ice on P12. All efforts were made to minimize animal suffering and minimize the number of animals used. Experimental protocols were approved by the University of Michigan Committee on Use and Care of Animals.
Drug treatment.
In five independent experiments to test the efficacy of prehypoxic-ischemic treatment, P7 rats received intraperitoneal injections of pentoxifylline (Research Biochemicals International, Natick, MA) immediately before and again immediately after hypoxia. In the first three experiments, with 3.25 h hypoxia duration, P7 rats received pentoxifylline 25, 75, or 150 mg/kg/dose (n = 5, 11, and 5, respectively), or an equal volume of PBS (PBS) vehicle (n = 17), immediately before and again immediately after hypoxia exposure. This initial dose range, derived from previous reports, was chosen to evaluate both safety and efficacy. In the subsequent two experiments, with 2.75-h hypoxia duration, P7 rats received pentoxifylline 40 mg/kg/dose (n = 13), or an equal volume of vehicle (PBS, n = 10), immediately before and again immediately after hypoxia exposure. In the prophylactic treatment regimens, we administered two doses of pentoxifylline, because the drug has a half-life of ≤1 h in rats (21, 38). By giving a dose immediately before the onset of hypoxia-ischemia and again immediately after the end of hypoxia exposure, we expected to have the drug in the circulation and in the CNS both during the episode of cerebral ischemia and during the early postischemic reperfusion phase, which begins immediately after the end of the hypoxia exposure. To test the efficacy of posthypoxic-ischemic treatment, we administered pentoxifylline to the animals (40 mg/kg/dose, n = 8) or vehicle (n = 10) immediately after the end of hypoxia exposure (2.75 h), and again 3 h later.
Neuropathology.
On P12, when brains were removed, ipsilateral liquefactive cerebral infarction was evaluated by an observer unaware of treatment identity (J.D.E.B.). In this model, marked hemispheric atrophy evolves rapidly and is apparent on gross inspection 5 d later (39). All brains were frozen under powered dry ice, and 20-μm coronal frozen brain sections, postfixed over paraformaldehyde vapors, were stained with cresyl violet for assessment of histopathology and morphometry.
Quantitative analysis of injury.
For initial quantification of the severity of brain injury on P12, bilateral hemispheric cross-sectional areas were measured from coronal sections at the level of the anterior commissure and mid-dorsal hippocampus (Fig. 1), using a computerized video camera-based image analysis system (with NIH Image software). A more detailed additional quantification of injury was performed on animals that had undergone posthypoxic-ischemic rescue treatment, to determine whether neuroprotection was regionally selective. For the latter analysis, bilateral striatal, neocortical, and dorsal hippocampal areas were measured in regularly spaced coronal sections, beginning at the level of the anterior genu of the corpus callosum and continuing to the level of the posterior genu of the corpus callosum. Unilateral cerebral atrophy evolves after unilateral cerebral hypoxia-ischemia in immature rats: thus, inter-hemispheric differences in areas or volumes provide a sensitive measure for quantification of injury or neuroprotection (40, 41).
Neuroprotective efficacy of pentoxifylline administration. These four cresyl violet-stained sections are from two concurrently lesioned, littermate P12 rats, evaluated 5 d after right carotid ligation, followed by 2.75 h in 8% O2. A and B are from a vehicle-treated control. C and D are from a rat treated with pentoxifylline (40 mg/kg/dose) immediately before and again after hypoxia. In A and B, note right cortical infarction (arrowhead), striatal atrophy (asterisk), and hippocampal atrophy and pyramidal cell loss (arrow). In C and D, note preservation of tissue integrity in the right cerebral hemisphere. cort = cortex;str = striatum;hip = hippocampus (scale bar = 1 mm).
Data analysis.
Microcomputer-based statistical programs [Statview (ABACUS, Berkeley, CA) and Systat (Systat Inc., Evanston, IL)] were used. Mean percent right-sided damage, compared with intact left side {i.e., mean % left-right (L-R) difference in hemispheric or regional areas or volumes [100 · (L-R)/L]} was compared among treatment groups and control rats by parametric and nonparametric tests. Hemisphere area measurements from pretreated animals exposed to either 3.25 or 2.75 h of hypoxia were analyzed separately. As a measure of neuroprotective efficacy, percent protection by pentoxifylline was calculated, based on comparison of the severity of injury in drug- and vehicle-treated animals, using the formula {100*[1-(% damage, drug-treated/% damage, vehicle-treated)]}. As a measure of the range of neuroprotection values observed, the SEM for percent protection was calculated as [100*(SEM, drug-treated/% damage vehicle-treated)], as previously described (9).
RESULTS
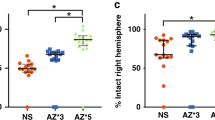
Right carotid ligation followed by 2.75–3.25 h of exposure to 8% oxygen resulted in a 75% incidence of ipsilateral liquefactive cerebral infarction in vehicle-treated controls. Histopathologic findings ipsilateral to carotid ligation included pallor, atrophy, and tissue loss in striatum, hippocampus, cortex, and thalamus (Fig. 1). Our first three experiments encompassed a broad dosage range, for evaluation of both safety and efficacy. Pretreatment with 150 mg/kg pentoxifylline resulted in 100% mortality; treatment with 75 mg/kg/dose resulted in approximately 20% mortality but marked neuroprotection in survivors, and there was similar mortality but no apparent neuroprotection at 25 mg/kg/dose (Table 1). These results influenced our subsequent study design, in which the intermediate dose level of 40 mg/kg was added, to evaluate dose-dependence of neuroprotective efficacy. Pretreatment with pentoxifylline (40 or 75 mg/kg/dose) resulted in a decreased incidence of liquefactive cerebral infarction on P12, ipsilateral to carotid ligation (p < 0.001, χ2 trend test) (Table 1 and Fig. 1). Quantification of hemispheric areas at two anatomic levels in rats that had received two serial doses of pentoxifylline (25, 40, or 75 mg/kg/dose immediately before and again immediately after hypoxia) and in control rats confirmed the results of the initial evaluation of tissue infarction (Table 2).
Although hypoxic-ischemic conditions were different in the first three and the subsequent two pretreatment experiments, in both cases, pentoxifylline pretreatment markedly attenuated the resulting brain damage. As a measure of neuroprotective efficacy of pentoxifylline pretreatment, we calculated the percent protection, based on inter-hemisphere area differences. Percent protection (mean ± SEM) by pretreatment with pentoxifylline 40 mg/kg/dose ranged from 72 ± 12% (anterior hemisphere) to 77 ± 8% (posterior hemisphere). Percent protection by pentoxifylline 75 mg/kg/dose ranged from 80 ± 10% (anterior hemisphere) to 84 ± 10% (posterior hemisphere). By posthoc analysis, pentoxifylline 25 mg/kg/dose did not attenuate hypoxic-ischemic brain injury.
Posthypoxic-ischemic rescue treatment with pentoxifylline (40 mg/kg/dose) did not result in a decrease in the incidence of cerebral infarction on P12 (Table 3). Furthermore, analysis of bilateral hemisphere areas indicated no difference in mean hemisphere areas between animals treated with pentoxifylline posthypoxia-ischemia and concurrent controls (Table 4). However, review of the histopathology suggested that cortical infarctions were less extensive in pentoxifylline-treated rats than in controls. To confirm this impression, we performed a morphometric analysis of bilateral cortical, striatal, and hippocampal volumes in animals treated posthypoxia-ischemia and in concurrent controls. This analysis of regional volumes indicated that neocortical damage was less severe in animals treated with pentoxifylline beginning after hypoxia-ischemia than it was in concurrent controls (Table 5). The percent protection (mean ± SEM) of cortical tissue by posthypoxic-ischemic rescue treatment with pentoxifylline was 54 ± 17.9%. In contrast, the severity of striatal and hippocampal damage was not attenuated by pentoxifylline administration post-insult. There were no deaths among the rats that received posthypoxic-ischemic pentoxifylline treatment, or among their littermate controls.
Intrahypoxic skin temperature and posthypoxic esophageal temperature in rats from four experiments did not differ among groups.
DISCUSSION
Treatment of immature rats with the alkylxanthine phosphodiesterase inhibitor pentoxifylline before induction of cerebral hypoxia-ischemia markedly attenuated subsequent ischemic forebrain injury. In contrast, when treatment with pentoxifylline was not initiated until after the end of the hypoxic-ischemic insult, the attenuation of damage was modest and was limited to the neocortex. This probably reflects progression of the injury cascade to the point of irreversibility before drug levels reached an effective tissue concentration. Our results add to the growing body of evidence that anti-inflammatory strategies can substantially attenuate neonatal hypoxic-ischemic brain injury. Other effective anti-inflammatory neuroprotective strategies for neonatal cerebral hypoxia-ischemia include pretreatment with dexamethasone (32), pre- or posthypoxic-ischemic treatment with the platelet-activating factor receptor antagonist BN 52021 (9), pre- or posthypoxic-ischemic treatment with IL-1 receptor antagonist (8, 42), and immune-mediated iatrogenic neutropenia before induction of hypoxia-ischemia (3). A comparison of the reported neuroprotective efficacy of these different anti-inflammatory strategies is presented in Table 6. The efficacy of pentoxifylline pretreatment is similar to some other pretreatment regimens (e.g., platelet-activating factor antagonist, IL-1 receptor antagonist, neutropenia) but is less effective than dexamethasone pretreatment. The neuroprotective efficacy of posthypoxic-ischemic pentoxifylline treatment is limited, compared with platelet-activating factor antagonist or IL-1 receptor antagonist administration.
Pentoxifylline is a cAMP phosphodiesterase inhibitor. Although other phosphodiesterase inhibitors (e.g., rolipram) have been reported to share some of the anti-inflammatory activities of pentoxifylline, we evaluated pentoxifylline both because of the large body of knowledge about its activities in vitro and in vivo, and because it is already approved for clinical use. Administration of pentoxifylline leads to increased intracellular cAMP accumulation in several cell types, including mononuclear phagocytes (43), microglia (14), neutrophils (43), vascular smooth muscle, and endothelium (44). Increased intracellular cAMP affects gene transcription through several transcription factors, such as cAMP response element-binding protein (45). Multiple complementary anti-inflammatory effects of pentoxifylline could be responsible for its neuroprotective efficacy, including inhibition of neutrophil (18) or monocyte/microglial (14) activation, attenuation of inflammatory mediator production (e.g., platelet-activating factor (17) or TNF-α (13), and prevention of endothelial-leukocyte adhesion (46).
Other effects of pentoxifylline, independent of its anti-inflammatory actions, could also contribute to its neuroprotective efficacy. Cerebrovascular resistance is regulated by cAMP phosphodiesterases (47). Pentoxifylline reportedly increases cerebral blood flow in humans who have cerebrovascular disease (48). Yet, under controlled laboratory conditions in mature dogs or rats undergoing global cerebral ischemia or ischemia-reperfusion, there is no increase in intra-ischemic or post-reperfusion regional cerebral blood flow with pentoxifylline treatment (27, 49). Despite these reports, it is possible that pentoxifylline might have the opposite effect on intra-ischemic or post-reperfusion cerebral blood flow in the immature brain. We have not yet evaluated the effect of pentoxifylline administration on either intra- or posthypoxic-ischemic cerebral blood flow in P7 rats; thus we cannot rule out the possibility that pentoxifylline's beneficial effect in P7 rats is due to increased intrahypoxic cerebral blood flow. Pentoxifylline could also have beneficial CNS parenchymal effects independent of effects on cerebral blood flow, perhaps mediated by preservation of CNS cAMP levels (50).
Variable neuroprotective efficacy of pentoxifylline therapy in mature animal models of cerebral ischemia has been reported (25–29). Possible explanations for inconsistencies in neuroprotective efficacy among studies include difference in drug dosage and timing, differences in injury models, and differences in outcome measures. This neonatal stroke model includes both a period of focal cerebral hypoxia-ischemia and a subsequent period of normoxia with reperfusion (51). Anti-inflammatory strategies, such as pentoxifylline treatment, may be more neuroprotective in the setting of cerebral ischemia with reperfusion than in permanent cerebral ischemia (52).
The cause of the high intra-hypoxic mortality, noted at 150 mg/kg/dose, is unknown. In mice, single pentoxifylline doses of 200 mg/kg are well tolerated, whereas apparent neurotoxicity and death follow a 400 mg/kg dose (37). P7 rats that died became apneic, with no visible seizures preceding apnea. Assisted ventilation to prevent apnea is not feasible in P7 rats because of their small size. Alternatively, increased mortality could have resulted from hypotension; blood pressure cannot be monitored because of their small size. Similar mortality was noted in experiments to evaluate the effect of pentoxifylline on N-methyl-D-aspartate neurotoxicity in P7 rats (F. S. Silverstein, personal communication); thus these detrimental effects are unlikely to be directly related to an interaction with systemic hypoxemia. Clinical trials of pentoxifylline as an adjunctive therapy in critically ill neonates and adults have not raised concerns about adverse side effects of pentoxifylline. Results of recent clinical trials suggest that pentoxifylline treatment may decrease mortality and morbidity associated with neonatal bacterial sepsis (53) and may attenuate multi-organ failure after cardiothoracic surgery in adults (54). Thus pentoxifylline might be suitable for clinical trial as a human neuroprotective agent in carefully selected patients at high risk of cerebral hypoxic or ischemic injury.
In conclusion, our results add to the growing body of evidence supporting the hypothesis that inflammatory mediators play a pathogenetic role in hypoxic-ischemic injury to the immature brain. Several strategies to interrupt the inflammatory cascade have proven effective in decreasing the severity of neonatal hypoxic-ischemic brain injury in experimental animals. These therapies have not yet reached clinical practice. Pretreatment with pentoxifylline may offer an effective means to decrease the incidence and severity of hypoxic-ischemic injury to the immature brain. Prophylactic treatment may be feasible in infants identified as having a high risk of cerebral hypoxia-ischemia—for example, infants undergoing heart-lung bypass for surgical repair of congenital cardiac defects or extracorporeal membrane oxygenation.
Abbreviations
- TNF-α:
-
tumor necrosis factor-α
- IL-1β:
-
interleukin-1β
- P7:
-
postnatal d 7
References
Barks JD, Silverstein FS 1992 Excitatory amino acids contribute to the pathogenesis of perinatal hypoxic-ischemic brain injury. Brain Pathol 2: 235–243.
Palmer C 1995 Hypoxic-ischemic encephalopathy: therapeutic approaches against microvascular injury, and role of neutrophils, PAF and free radicals. Clin Perinatol 22: 481–517.
Hudome S, Palmer C, Roberts RL, Mauger D, Housman C, Towfighi J 1997 The role of neutrophils in the production of hypoxic-ischemic brain injury in the neonatal rat. Pediatr Res 41: 607–616.
Ivacko JA, Sun R, Silverstein FS 1996 Hypoxic-ischemic brain injury induces an acute microglial reaction in perinatal rats. Pediatr Res 39: 39–47.
Ohno M, Aotani H, Shimada M 1995 Glial responses to hypoxic/ischemic encephalopathy in neonatal rat cerebrum. Dev Brain Res 84: 294–298.
Hagan P, Poole S, Bristow AF, Tilders F, Silverstein FS 1996 Intracerebral NMDA injection stimulates production of interleukin-1 beta in perinatal rat brain. J Neurochem 67: 2215–2218.
Szaflarski J, Burtrum D, Silverstein FS 1995 Cerebral hypoxia-ischemia stimulates cytokine gene expression in perinatal rats. Stroke 26: 1093–1100.
Martin D, Chinookoswong N, Miller G 1994 The interleukin-1 receptor antagonist (rhIL-1ra) protects against cerebral infarction in a rat model of hypoxia-ischemia. Exp Neurol 130: 362–367.
Liu XH, Eun BL, Silverstein FS, Barks JDE 1996 The platelet-activating factor antagonist BN 52021 attenuates hypoxic-ischemic brain injury in the immature rat. Pediatr Res 40: 797–803.
Muller R 1981 Hemorheology and peripheral vascular diseases: a new therapeutic approach. J Med 12: 209–235.
Porter JM, Cutler BS, Lee BY, Reich T, Reichle FA, Scogin JT, Strandness DE 1982 Pentoxifylline efficacy in the treatment of intermittent claudication: multicenter controlled double-blind trial with objective assessment of chronic occlusive arterial disease patients. Am Heart J 104: 66–72.
Hood SC, Moher D, Barber CG 1996 Management of intermittent claudication with pentoxifylline: meta-analysis of randomized controlled trials. Can Med Assoc J 155: 1053–1059.
Strieter RM, Remick DG, Ward PA, Spengler RN, Lynch JP, Larrick J, Kunkel SL 1988 Cellular and molecular regulation of tumor necrosis factor-alpha production by pentoxifylline. Biochem Biophys Res Commun 155: 1230–1236.
Chao CC, Hu S, Close K, Choi CS, Molitor TW, Novick WJ, Peterson PK 1992 Cytokine release from microglia: differential inhibition by pentoxifylline and dexamethasone. J Infect Dis 166: 847–853.
Ollivier V, Ternisien C, Vu T, Hakim J, de Prost D 1993 Pentoxifylline inhibits the expression of tissue factor mRNA in endotoxin-activated human monocytes. FEBS Lett 322: 231–234.
Leclerc NE, Haan-Archipoff G, Lenoble M, Beretz A 1995 Inhibitors of phosphodiesterase (pentoxifylline, trequinsin) inhibit apical and subcellular matrix expression of tissue factor in cultured human endothelial cells. J Cardiovasc Pharmacol 25: S88–S91.
Adams JG Jr, Dhar A, Shukla SD, Silver D 1995 Effect of pentoxifylline on tissue injury and platelet-activating factor production during ischemia-reperfusion injury. J Vasc Surg 21: 742–749.
Sullivan GW, Carper HT, Novick WJ Jr, Mandell GL 1988 Inhibition of the inflammatory action of interleukin-1 and tumor necrosis factor (alpha) on neutrophil function by pentoxifylline. Infect Immun 56: 1722–1729.
Zheng H, Crowley JJ, Chan JC, Hoffmann H, Hatherill JR, Ishizaka A, Raffin TA 1990 Attenuation of tumor necrosis factor-induced endothelial cell cytotoxicity and neutrophil chemiluminescence. Am Rev Respir Dis 142: 1073–1078.
Mandell GL 1995 Cytokines, phagocytes, and pentoxifylline. J Cardiovasc Pharmacol 25: S20–S22.
Fujimoto K, Yoshida S, Moriyama Y, Sakaguchi T 1976 Absorption, distribution, excretion, and metabolism of 1-(5-oxohexyl) theobromine (BL 191) in rats. Chem Pharm Bull Tokyo 24: 1137–1145.
Shohami E, Bass R, Wallach D, Yamin A, Gallily R 1996 Inhibition of tumor necrosis factor alpha (TNFα) activity in rat brain is associated with cerebroprotection after closed head injury. J Cereb Blood Flow Metab 16: 378–384.
Hong JH, Chiang CS, Campbell IL, Sun JR, Withers HR, McBride WH 1995 Induction of acute phase gene expression by brain irradiation. Int J Radiat Oncol Biol Phys 33: 619–626.
Nataf S, Louboutin JP, Chabannes D, Feve JR, Muller JY 1993 Pentoxifylline inhibits experimental allergic encephalomyelitis. Acta Neurol Scand 88: 97–99.
Bluhm RE, Molnar J, Cohen MM 1985 The effect of pentoxifylline on the energy metabolism of ischemic gerbil brain. Clin Neuropharmacol 8: 280–285.
Hartmann JF, Becker RA, Cohen MM 1977 Effects of pentoxifylline on cerebral ultrastructure of normal and ischemic gerbils. Neurology 27: 77–84.
Toung TJ, Kirsch JR, Maruki Y, Traystman RJ 1994 Effects of pentoxifylline on cerebral blood flow, metabolism, and evoked response after total cerebral ischemia in dogs. Crit Care Med 22: 273–281.
Tanahashi N, Fukuuchi Y, Tomita M, Kobari M, Takeda H, Yokoyama M 1995 Pentoxifylline ameliorates postischemic delayed hypoperfusion of the cerebral cortex following cardiac arrest in cats. J Neurol Sci 132: 105–109.
Steen PA, Milde JH, Michenfelder JD 1982 Pentoxifylline in regional cerebral ischemia in cats. Acta Anaesthesiol Scand 26: 39–43.
Krause PJ, Maderazo EG, Contrino J, Eisenfeld L, Herson VC, Greca N, Bannon P, Kreutzer DL 1991 Modulation of neonatal neutrophil function by pentoxifylline. Pediatr Res 29: 123–127.
Newton JA, Ashwood ER, Yang KD, Augustine NH, Hill HR 1989 Effect of pentoxifylline on developmental changes in neutrophil cell surface mobility and membrane fluidity. J Cell Physiol 140: 427–431.
Barks JD, Post M, Tuor UI 1991 Dexamethasone prevents hypoxic-ischemic brain damage in the neonatal rat. Pediatr Res 29: 558–563.
Dobbing J, Sands J 1979 Comparative aspects of the brain growth spurt. Early Hum Dev 3: 79–83.
Romijn HJ, Hofman MA, Gramsbergen A 1991 At what age is the developing cerebral cortex of the rat comparable to that of the full-term human baby?. Early Hum Dev 26: 61–67.
McIlwain H, Bachelard HS 1985 Chemical and enzymatic makeup of the brain during development and ageing. In: McIlwain H, Bachelard HS (eds) Biochemistry and the Central Nervous System. Churchill Livingstone, Edinburgh, 371–412.
Trescher WH, Lehman RA, Vannucci RC 1990 The influence of growth retardation on perinatal hypoxic-ischemic brain damage. Early Hum Dev 21: 165–173.
Honess DJ, Dennis IF, Bleehen NM 1993 Pentoxifylline: its pharmacokinetics and ability to improve tumour perfusion and radiosensitivity in mice. Radiother Oncol 28: 208–218.
Rocci ML Jr, Luke DR, Saccar CL 1987 Pharmacokinetics of pentoxifylline during concomitant theophylline administration to rats. Pharm Res 4: 433–435.
Rice JE, Vannucci RC, Brierley JB 1981 The influence of immaturity on hypoxic-ischemic brain damage in the rat. Ann Neurol 9: 131–141.
McDonald JW, Roeser NF, Silverstein FS, Johnston MV 1989 Quantitative assessment of neuroprotection against NMDA-induced brain injury. Exp Neurol 106: 289–296.
Andine P, Thordstein M, Kjellmer I, Nordborg C, Thiringer K, Wennberg E, Hagberg H 1990 Evaluation of brain damage in a rat model of neonatal hypoxic-ischemia. J Neurosci Meth 35: 253–260.
Hagberg H, Gilland E, Bona E, Hanson LÅ, Hahn-Zoric M, Blennow M, Holst M, McRae A, Söder O 1996 Enhanced expression of interleukin (IL)-1 and IL-6 messenger RNA and bioactive protein after hypoxia-ischemia in neonatal rats. Pediatr Res 40: 603–609.
Bessler H, Gilgal R, Djaldetti M, Zahavi I 1986 Effect of pentoxifylline on the phagocytic activity, cAMP levels, and superoxide anion production by monocytes and polymorphonuclear cells. J Leukoc Biol 40: 747–754.
Rosenblum WI, Shimizu T, Nelson GH 1993 Interaction of endothelium with dilation produced by inhibitors of cyclic nucleotide diesterases in mouse brain arterioles in vivo. Stroke 24: 266–270.
Hakim J 1995 Pharmacologic control of intracellular signaling pathways: from research to therapy. J Cardiovasc Pharmacol 25: S106–S113.
Salyer JL, Bohnsack JF, Knape WA, Shigeoka AO, Ashwood ER, Hill HR 1990 Mechanisms of tumor necrosis factor-alpha alteration of PMN adhesion and migration. Am J Pathol 136: 831–841.
Willette RN, Shiloh AO, Sauermelch CF, Sulpizio A, Michell MP, Cieslinski LB, Torphy TJ, Ohlstein EH 1997 Identification, characterization, and functional role of phosphodiesterase type IV in cerebral vessels: effects of selective phosphodiesterase inhibitors. J Cereb Blood Flow Metab 17: 210–219.
Bowton DL, Stump DA, Prough DS, Toole JF, Lefkowitz DS, Coker L 1989 Pentoxifylline increases cerebral blood flow in patients with cerebrovascular disease. Stroke 20: 1662–1666.
Johansson BB 1986 Pentoxifylline: cerebral blood flow and glucose utilization in conscious spontaneously hypertensive rats. Stroke 17: 744–747.
Rudman D, Fleischer A, Kutner MH 1976 Concentration of 3′,5′ cyclic adenosine monophosphate in ventricular cerebrospinal fluid of patients with prolonged coma after head trauma or intracranial hemorrhage. N Engl J Med 295: 635–638.
Mujsce DJ, Christensen MA, Vannucci RC 1990 Cerebral blood flow and edema in perinatal hypoxic-ischemic brain damage. Pediatr Res 27: 450–453.
Hartl R, Schurer L, Schmid-Schonbein GW, del Zoppo GJ 1996 Experimental antileukocyte interventions in cerebral ischemia. J Cereb Blood Flow Metab 16: 1108–1119.
Lauterbach R, Pawlik D, Kowalczyk D, Ksycinski W, Helwich E, Zembala M 1999 Effect of the immunomodulating agent, pentoxifylline, in the treatment of sepsis in prematurely delivered infants: a placebo-controlled, double-blind trial. Crit Care Med 27: 807–814.
Hoffman H, Markewitz A, Kreuzer E, Reichert K, Jochum M, Faist E 1998 Pentoxifylline decreases the incidence of multiple organ failure in patients after major cardio-thoracic surgery. Shock 9: 235–240.
Acknowledgements
The authors thank Dr. F. S. Silverstein for helpful comments, and also thank Alicia Crossland, Priti Mody, and Yi-Qing Liu for valuable technical assistance.
Author information
Authors and Affiliations
Additional information
Funding support was provided by the United Cerebral Palsy Research and Education Foundation Grants R-608–94 and R-608–97, and by National Institutes of Health Grant NS 37036.
Rights and permissions
About this article
Cite this article
Eun, BL., Liu, XH. & Barks, J. Pentoxifylline Attenuates Hypoxic-Ischemic Brain Injury in Immature Rats. Pediatr Res 47, 73 (2000). https://doi.org/10.1203/00006450-200001000-00014
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200001000-00014
This article is cited by
-
Neuroprotective Effects of Theobromine in permanent bilateral common carotid artery occlusion rat model of cerebral hypoperfusion
Metabolic Brain Disease (2022)
-
Pentoxifylline Alleviates Early Brain Injury in a Rat Model of Subarachnoid Hemorrhage
Acta Neurochirurgica (2016)
-
In vitro hemorheological effects of parenteral agents used in peripheral arterial disease
Korea-Australia Rheology Journal (2014)