Abstract
We assessed renal and cardiovascular function in preterm newborn lambs after antenatal glucocorticoid exposure. Pregnant ewes were randomly assigned to receive betamethasone or saline via either direct fetal or maternal injection at 122 d gestation. Lambs were delivered 15 h later, and cardiovascular and renal function was assessed. Two hours after delivery, baseline urine flow, urinary sodium excretion, and urinary osmolar clearance were similar in all groups. Volume expansion (saline, 2.5% of body weight, for 10 min) increased values for urine flow (0.23 ± 0.04 to 0.58 ± 0.09 mL·min−1·kg−1), urinary sodium excretion (29.7 ± 5.8 to 76.2 ± 12.3 μEq·min−1·kg−1), and osmolar clearance (12.2 ± 1.2 to 24.3 ± 1.6 mL/100 mL GFR) in the fetal group. Increases in urine values were also observed in the maternal group, but control values did not change significantly. Mean arterial pressure was increased in both betamethasone-treated groups relative to controls. Short-term antenatal betamethasone exposure 1) augments preterm newborn kidney adaptive responses to acute volume expansion, and 2) increases postnatal blood pressure in preterm newborn lambs.
Similar content being viewed by others
Main
Antenatal glucocorticoid administration and surfactant replacement therapy have improved pulmonary outcomes in premature newborns. However, immaturity of other organ systems, including the cardiovascular and renal systems, also contribute to the long-term complications associated with prematurity. Recognizing these complications, the National Institutes of Health Consensus Conference recommended the use of antenatal glucocorticoids in cases of threatened preterm delivery and highlighted the need to better understand the effects of antenatal glucocorticoids on organ system maturation and neonatal hemodynamic stability (1).
Preterm newborns often exhibit disordered blood pressure regulation, which has been associated with intraventricular hemorrhage and periventricular leukomalacia (2, 3). However, when acute volume infusions are used in an attempt to increase blood pressure in the premature newborn (4), extravascular fluid retention may occur in part because of the inability of the immature kidney to excrete the volume load. The resulting fluid retention can contribute to lung injury through the development of pulmonary edema. In addition, the limited ability of premature newborns to regulate fluid and solute homeostasis can lead to severe electrolyte abnormalities and increased morbidity (5).
The minimum treatment-to-delivery interval and optimal route of administration to induce improvements in postnatal organ system function remain unclear. Recent studies have demonstrated marked betamethasone-induced effects on cardiovascular and renal functions in premature newborn lambs 24 h after antenatal exposure (6). The present study used a short-term volume infusion to test the hypothesis that cardiovascular and renal maturational effects could be induced after a shorter (15 h) period of intrauterine glucocorticoid exposure. Because there are differential effects on fetal lung maturation and growth resulting from fetal or maternal glucocorticoid treatments in sheep (7), we also asked whether the route of glucocorticoid administration (maternal versus direct fetal) is an important determinant of renal and cardiovascular adaptation.
METHODS
Animals.
Animal handling and study protocols were reviewed and approved by the Harbor-UCLA Animal Care and Use Review Committee. Pregnant ewes with singleton fetuses (n = 26) at 123 d gestation were randomized to one of two betamethasone treatment groups or to a saline-treated group. All maternal-fetal pairs received fetal and maternal injections with saline or betamethasone to control for possible injection-related effects. Treated fetuses received 0.5 mg/kg betamethasone (Celestone Soluspan; Schering Pharmaceutical, Kenilworth, NJ) given by intramuscular injection (8), and treated ewes (mean weight, 58 kg) received 0.5 mg/kg betamethasone. The control group received fetal and maternal saline injections. The pulmonary outcomes were presented elsewhere (9). The focus of this report will be the renal, cardiovascular, and endocrine responses of the prematurely delivered newborns.
Fifteen hours after the maternal-fetal injections, lambs were delivered by cesarean section. The delivery and postnatal care were by methods reported previously for preterm lambs (6). The ewes were sedated with 15–20 mg/kg ketamine intramuscularly and given combined spinal-epidural anesthesia with 10 mL of 2% lidocaine/0.5% bupivacaine (1:1). The fetal head and neck were exposed through a small hysterotomy. Lambs were anesthetized with ketamine (10 mg/kg) and acepromazine (0.2 mg/kg) on the basis of estimated fetal weight, and the anterior neck was infiltrated with 2% lidocaine.
The investigators delivering and managing the preterm lambs were blinded as to treatment groups. After surfactant treatment (100 mg/kg Survanta; Ross Products, Abbott Laboratories, Chicago, IL) and initiation of ventilation (1–2 min after birth), a catheter was placed in the descending aorta via the umbilical artery for blood sampling and blood pressure monitoring, and a urinary bladder catheter was placed by suprapubic cystotomy to permit timed urine collections. A single dose of [methoxy-3H]inulin (10 μCi) and 10 mL/kg of heparinized placental blood were administered within 5 min of delivery, and blood pressure and heart rate were monitored continuously. A left ventricular catheter was placed via the right carotid artery for continuous pressure measurement and injection of microspheres. Vascular catheter patency was maintained by continuous infusion of 5% dextrose in water and 0.15 M saline for a total of 4.4 mL·h−1·kg−1. Blood samples were replaced vol/vol with maternal blood that was filtered (Hemonate; Gesco International, San Antonio, TX) immediately before infusion. Body temperature was monitored with a rectal probe and maintained at 39°C (±0.5°C) by use of a radiant warmer, heating pads, and heat lamps. Blood pressure and reflex responses were carefully monitored and intramuscular anesthesia (ketamine, 10 mg/kg; acepromazine, 0.2 mg/kg) was readministered as necessary. Lambs were stabilized and studied for a total of 3 h. At the end of the study, lambs were killed with i.v. pentobarbital (100 mg/kg) and were reweighed.
Volume loading protocol.
Two hours after delivery, an i.v. volume load of 0.15 M saline (25 mL/kg body weight for 10 min) was infused into each lamb by use of a dual-channel infusion pump (Harvard Apparatus Co, South Natick, MA). Cardiac output and renal blood flow were measured by a left ventricular injection of 10 μCi 57Co-labeled and 85Sc-labeled microspheres (approximately 4 × 105 microspheres, 15.5 ± 0.1 μm diameter, mixed in 5 mL of maternal blood; New England Nuclear, Boston, MA) before and 5 min after completion of the volume infusion, respectively (10). A reference sample was simultaneously withdrawn with a Harvard pump from the descending aortic catheter at a rate of 5 mL/min for 2 min into a preweighed, heparinized syringe. The volume of blood withdrawn was determined gravimetrically, and radioactivity was quantified in an LKB Compugamma counter (Wallac, Inc., Gaithersburg, MD) equipped with automatic pulse height correction.
Arterial blood samples.
Blood samples were collected from the umbilical cord after delivery of the lamb, and via the umbilical artery catheter for measurements of arterial blood gases, pH, hematocrit, plasma osmolality, electrolyte concentrations (sodium, potassium, chloride), [3H]inulin, and hormone determinations (PRA, AII, aldosterone, norepinephrine, and epinephrine). Ventilatory status was assessed by measuring arterial blood gases (Po2, Pco2) and pH approximately every 30 min, or 5 min after ventilator adjustments.
Cardiovascular.
Aortic blood pressure and heart rate were monitored continuously via pressure transducers connected to a Beckman R-612 polygraph (Beckman Instruments, San Ramon, CA). Heart rate was computed from the arterial pulse. In addition to the continuous paper hardcopy, acquired data were continuously streamed (20 Hz per channel) to an AT microcomputer by use of Codas acquisition software (DATAQ Instruments, Akron, OH). Mean blood pressure and heart rate values were derived by post hoc analysis of the acquired data.
Urine samples.
Serial urine samples collected at 30, 60, 90, 120, 150, and 180 min provided data on urine flow, osmolality, electrolyte concentrations, and inulin specific activity for all lambs. The values obtained at times before 150 min were combined to give a single preinfusion value (PRE). Values at 150 min represent the infusion time (INFUSION) and at 180 min, the recovery period time (RECOVERY).
Analytical methods.
Blood samples were transferred immediately into chilled tubes for determination of plasma aldosterone, PRA, osmolality, electrolytes, catecholamine concentrations, and [3H]inulin (lithium heparin; 40 μg/mL blood), and AII (K2EDTA, 1 mg/mL; aprotinin, 500 KIU/mL blood). All tubes were mixed by a vortex and centrifuged immediately at 4°C. Plasma samples for hormone analysis were separated and frozen (−20°C) for extraction within 1–2 wk. Plasma sodium, potassium, and chloride concentrations were determined on a NOVA electrolyte analyzer (NOVA Biomedicals, Waltham, MA), and osmolalities were determined by freezing point depression (Advanced Digimatic osmometer, model MO; Advanced Instruments, Needham Heights, MA). Plasma and urine inulin concentrations were assessed by counting aliquots (0.1 mL) in hydrofluor (National Diagnostics, Somerville, NJ) in a Beckman LS-335 liquid scintillation counter (Beckman Instruments). Blood pH, Po2, and Pco2 values were determined on a NOVA Stat Profile Plus 3 blood analyzer (Nova Biomedical).
Plasma AII concentrations were determined by use of RIA kits obtained from Peninsula Laboratories (Belmont, CA) with intra-assay and interassay coefficients of variation of 6% and 9%, respectively. PRA was measured indirectly using the RIANEN Angiotensin I (125I) RIA kit (Dupont Medical Products, Boston, MA). Plasma aldosterone concentrations were determined by RIA with kits provided by ICN Biomedicals (Costa Mesa, CA). Plasma catecholamine concentrations were determined by radioenzymatic assay sensitive to 10–20 pg/mL.
Data analysis.
All values are expressed as the mean ± SEM. Differences as a function of time and differences between saline- and betamethasone-treated groups were assessed by two-way ANOVA. Student-Newman-Keuls analysis was performed on all variables found to be significant by ANOVA. Statistical significance for all analyses was accepted at p < 0.05.
RESULTS
Mean body weights at delivery were comparable in the control (2.4 ± 0.1 kg;n = 9), fetal (2.3 ± 0.1 kg;n = 8), and maternal (2.4 ± 0.1 kg;n = 9) treatment groups. In the control group, the hematocrit decreased in response to volume loading (43 ± 1% to 36 ± 1%) with return to baseline values after the volume infusion (41 ± 1%). The betamethasone-treated groups had comparable values to the control group at baseline (43 ± 1% in both groups) and immediately after the infusion (37 ± 1% for both groups). In contrast to the control group, however, hematocrit remained lower throughout the remainder of the study (maternal, 38 ± 1%; fetal, 37 ± 1%) in the betamethasone-treated groups. There were no differences in arterial pH and Po2 values among the groups (Table 1). Arterial Pco2 values were maintained within the target values.
Before the volume infusion, all groups had comparable plasma electrolyte values, whereas plasma osmolality values were higher in the maternal treatment group (Table 1). After the saline infusion, all groups had comparable plasma electrolytes except for lower potassium values in the maternal treated group.
Renal.
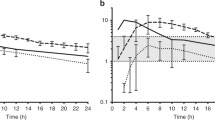
Urine chloride concentrations and GFR values were higher in the fetal betamethasone-treated animals throughout the study (Table 2). All other renal values were comparable among the groups during the preinfusion period. After the 25 mL/kg saline infusion and at the end of the recovery period, urine sodium concentration increased and urine potassium concentration decreased in betamethasone-treated animals without changes in urine osmolality or free water clearance. Urine flow, UNaV, and urinary osmolar clearance are shown in Figure 1. For all figures, PRE represents the time before the fluid bolus, 150 min represent the INFUSION time, and 180 min the RECOVERY time. Volume infusion increased urine flow, UNaV, and osmolar clearance in both glucocorticoid-treated groups. Despite trends toward increased urine flow and UNaV with volume infusion, no significant changes were noted in the control group. Osmolar clearance remained elevated in the fetal betamethasone-treatment group through the recovery period.
Cardiovascular.
Mean arterial pressure was significantly higher after antenatal glucocorticoid exposure throughout the study (Fig. 2). Before the volume challenge, newborn heart rates were lower in the maternal betamethasone-treated lambs (Table 3) relative to the control group. In response to saline infusion, end-diastolic pressure increased in the control group, but no other changes in measured cardiovascular variables were noted. After the volume infusion, fetal-treated renal blood flow values were approximately twice control values. However, renal blood flow and renal plasma flow values did not change within the groups in response to the saline infusion.
Endocrine.
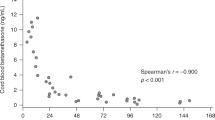
Plasma umbilical cord blood values for aldosterone were comparable in all groups (Fig. 3). After delivery, PRA, AII, and aldosterone concentrations (Fig. 3), as well as plasma norepinephrine and epinephrine concentrations (Fig. 4), were markedly suppressed in both betamethasone-treated groups relative to the control group. Plasma aldosterone concentrations in the control group were much higher after delivery than AII and aldosterone concentrations, suggesting a disassociation of the renin-angiotensin system in this group. Although PRA, aldosterone, and AII concentrations increased during the recovery period in control animals, no changes in hormone concentrations were noted in the glucocorticoid-exposed animals.
PRA, AII, and aldosterone in umbilical cord blood (Cord) and before (Pre), during (Infusion), and after (Post) a 25 mL/kg volume infusion in preterm newborn lambs following placebo (control) or betamethasone (via maternal or fetal administration) 15 h before delivery. Values are mean ± SEM. *p < 0.05 vs maternal and fetal values.
DISCUSSION
Antenatal glucocorticoid administration is recommended for most cases of threatened preterm delivery to improve subsequent outcome (1). Despite the widespread clinical use of antenatal glucocorticoids, many questions remain, including the optimal route of administration and minimum treatment-to-delivery interval required to induce maturation. In this investigation, premature newborn lambs were exposed to glucocorticoids for only 15 h before delivery. We observed that a large (25 mL/kg) fluid bolus administered at 2 h of life was effectively excreted by the glucocorticoid-exposed animals, whereas fluid retention was observed in the control group. In addition, we confirmed previous findings that short-term prenatal exposure to glucocorticoids increases mean arterial pressure relative to the control group. Of importance, these glucocorticoid-induced renal and cardiovascular effects were observed after only 15 h of antenatal exposure, regardless of the route of administration. Our findings support the National Institutes of Health Consensus Conference recommendation to administer antenatal glucocorticoids (unless immediate delivery is anticipated) even if 24 h of antenatal exposure is unlikely.
Fluid infusions are often used to treat hypotension in the preterm newborn (4). However, volume infusions in these infants can result in inappropriate fluid retention secondary to an inability to excrete the volume load. Because pulmonary edema is strongly implicated in the development of chronic lung disease, aggressive fluid management of hypotension may predispose preterm infants to unintentional pulmonary morbidity (11). The saline infusion in this study was large enough to reduce hematocrit values, but did not change blood pressure or cardiac output in any group. However, the betamethasone-treated lambs responded to the volume load by appropriately excreting the fluid load. In contrast, hematocrit values in the control group returned to preinfusion values consistent with extravascular fluid retention. These findings suggest antenatal glucocorticoid exposure may decrease capillary permeability caused by endothelial effects as well as improve the ability of the kidney to excrete a volume load.
The mechanism by which the betamethasone-exposed groups increased urine flow and UNaV in response to the saline infusion is unclear. Although renal blood flow and renal plasma flow tended to be higher, it is unlikely these increases are the sole contributors to the enhanced excretion in the steroid-exposed groups. Glucocorticoid-induced suppression of the renin-angiotensin system may have contributed to the renal excretion of the volume load. Suppression of the renin-angiotensin system, including both renal renin gene expression (12) and PRA (13), has been observed after glucocorticoid exposure. Given that PRA is suppressed in the absence of renal nerve activity, it is also possible that the reduced sympathetic activity secondary to glucocorticoid treatment contributed to the lower PRA observed in the treated groups (14). The apparent uncoupling of the renin-angiotensin system in the control animals may reflect the cessation of placental clearance of aldosterone with immature compensatory mechanisms. Regardless of the mechanism, elevated concentrations of PRA, aldosterone, and AII (which are likely required for cardiovascular stability in the control animals) result in fluid retention.
Disordered blood pressure regulation has been linked to the development of intraventricular hemorrhage and periventricular leukomalacia (2, 3). Consistent with previous studies in the ovine model, we observed increased baseline blood pressure values in the steroid-exposed groups (6). These findings are also consistent with data from preterm human newborns exposed to antenatal glucocorticoids who have reduced vasopressor requirements to maintain normal blood pressure values (15). The mechanism(s) for the increased blood pressure values in the betamethasone-treated groups is unclear. Despite the importance of the sympathetic nervous system (16) and AII (17) in blood pressure regulation at preterm gestation, the betamethasone-treated groups had markedly decreased plasma catecholamine and AII values relative to the control lambs. Regardless of the exact mechanism for blood pressure increases with glucocorticoid treatment, the unchanged cardiac output in the lambs suggests these blood pressure increases are likely related to increases in peripheral vascular resistance.
We compared the importance of the route of administration of betamethasone with induced functional changes in the renal and cardiovascular systems of preterm newborns. Because the antenatal exposure period was short, we anticipated direct fetal injection would induce maturational changes and transplacental betamethasone would not. With the exception of higher GFR values noted in the fetal betamethasone-treatment group, the maternal and fetal treatment groups demonstrated comparable effects in renal and cardiovascular function. It is unclear whether a shorter treatment-to-delivery interval might favor the effects of fetal treatment.
In summary, we compared preterm fetal lambs treated with one dose of betamethasone 15 h before delivery with saline-treated controls for evaluation of cardiovascular, renal, and endocrine changes after birth. We found an enhanced ability to excrete a volume infusion in the betamethasone-treated animals without changes in baseline blood pressure values. In addition, increased basal blood pressure values were observed in the glucocorticoid-treated lambs throughout the study. These results indicate that short-term antenatal glucocorticoid exposure increases blood pressure and the responsiveness of these newborns to excrete a volume challenge. We speculate that fetal glucocorticoid-induced cardiovascular and renal improvements may contribute to the improvements in long-term outcome in the premature newborn.
Abbreviations
- UNaV:
-
urinary sodium excretion
- AII:
-
angiotensin II
- PRA:
-
plasma renin activity
References
National Institutes of Health Consensus Development Panel 1995 Effect of corticosteroids for fetal maturation on perinatal outcomes. JAMA 273: 413–418.
Iida K, Takashima S, Takeuchi Y 1992 Etiologies and distribution of neonatal leukomalacia. Pediatr Neurol 8: 205–209.
Watkins AM, West CR, Cooke RW 1989 Blood pressure and cerebral hemorrhage and ischaemia in very low birthweight infants. Early Hum Dev 19: 103–110.
So KW, Fok TF, Ng PC, Wong WW, Cheung KL 1997 Randomised controlled trial of colloid or crystalloid in hypotensive preterm infants. Arch Dis Child Fetal Neonatal Ed 76: F43–F46.
Vanpee M, Herin P, Zetterstrom R, Aperia A 1988 Postnatal development of renal function in very low birthweight infants. Acta Paediatr Scand 77: 191–197.
Berry LM, Polk DH, Ikegami M, Jobe AH, Padbury JF, Ervin MG 1997 Preterm newborn lamb renal and cardiovascular responses after fetal or maternal antenatal betamethasone. Am J Physiol 272: R1972–R1979.
Jobe AH, Newnham J, Willet K, Sly P, Ikegami M 1998 Fetal versus maternal and gestational age effects of repetitive antenatal glucocorticoids. Pediatrics 102: 1116–1125.
Jobe AH, Polk D, Ikegami M, Newnham J, Sly P, Kohen R, Kelly R 1993 Lung responses to ultrasound guided fetal treatments with corticosteroids in preterm lambs. J Appl Physiol 75: 2099–2105.
Rebello CM, Ikegami M, Ervin MG, Polk DH, Jobe AH 1997 Postnatal lung function and protein permeability after fetal or maternal corticosteroids in preterm lambs. J Appl Physiol 83: 213–218.
Heymann MA, Payne DB, Hoffman JE, Rudolph AM 1977 Blood flow measurements with radionuclide-labeled particles. Prog Cardiovasc Dis 20: 55–79.
Hallman M 1989 The severity of RDS during the first two neonatal days in relationship to fluid intake. Acta Paediatr Scand Suppl 360: 93–100.
Segar JL, Bedell K, Page WV, Mazursky JE, Nuyt AM, Robillard JE 1995 Effect of cortisol on gene expression of the renin-angiotensin system in fetal sheep. Pediatr Res 37: 741–746.
Wood CE, Keil LC, Rudolph AM 1987 Physiological inhibition of ovine fetal plasma renin activity by cortisol infusion. Am J Physiol 253: R904–R909.
Smith FG, Smith BA, Guillery EN, Robillard JE 1991 Role of renal sympathetic nerves in lambs during the transition from fetal to newborn life. J Clin Invest 88: 1988–1994.
Moïse AA, Wearden ME, Kozinetz CA, Gest AL, Welty SE, Hansen TN 1995 Antenatal steroids are associated with less need for blood pressure support in extremely premature infants. Pediatrics 95: 845–850.
Padbury JF, Agata Y, Ludlow J, Ikegami M, Baylen B, Humme J 1987 Effect of fetal adrenalectomy on catecholamine release and physiologic adaptation at birth in sheep. J Clin Invest 80: 1096–1103.
Iwamoto HS, Rudolph AM 1979 Effects of endogenous angiotensin II on the fetal circulation. J Dev Physiol 1: 283–293.
Author information
Authors and Affiliations
Additional information
Supported in part by Grant HD-29713 from the National Institute of Child Health and Human Development, National Institutes of Health, an Established Investigatorship Award (M.G.E.) from the American Heart Association, and Grant 3 M01 RR00425–2754 from National Institutes of Health (L.M.S.).
Rights and permissions
About this article
Cite this article
Smith, L., Ervin, M., Wada, N. et al. Antenatal Glucocorticoids Alter Postnatal Preterm Lamb Renal and Cardiovascular Responses to Intravascular Volume Expansion. Pediatr Res 47, 622–627 (2000). https://doi.org/10.1203/00006450-200005000-00011
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200005000-00011