Abstract
Inhaled nitric oxide (iNO) is a specific pulmonary vasodilator. By serving as a pro-oxidant or antioxidant, iNO may influence other pulmonary functions as well. This study was designed to test the hypothesis that iNO affects the alveolar lining after premature birth. Preterm rabbits (gestation 29 d, term 31 d) were nose-only exposed NO (14 ppm) and 98% O2 for 20 h. The others were exposed to either 98% O2 or air. In another experiment, premature rabbits were exposed to either NO in air or to air. After the exposure, bronchoalveolar lavage (BAL) was performed and the surfactant aggregates were isolated. The surfactant components and surface activity were analyzed. In total, 144 animals were studied. There were no significant differences in the number, distribution, or respiratory burst activity of cells recovered by BAL. Neither brief hyperoxia nor iNO increased plasma-derived proteins in BAL. Exposure to O2 decreased large surfactant aggregates, surface activity, and the content of surfactant protein B in BAL, whereas iNO prevented completely or partially these effects of acute hyperoxia on surfactant. Hyperoxia increased the content of malondialdehyde and decreased glutathione in epithelial lining fluid. iNO decreased malondialdehyde (p < 0.05) and tended to increase glutathione (p = 0.06) in animals breathing O2. Nitrotyrosine was not detectable in BAL, and NO2 was low in the breathing area. In room air, iNO had no significant effect on surfactant. According to the present results, a brief period of hyperoxia causes an oxidant stress and decreases the surface activity of alveolar surfactant in premature rabbits. In contrast, a low dosage of iNO decreased or prevented the O2-induced detrimental effects on alveolar surfactant and alleviated the oxidant stress.
Similar content being viewed by others
Main
NO from vascular endothelial cells increases cyclic GMP production in vascular smooth muscle cells, causing muscle relaxation and improving perfusion (1,2). Inhaled NO improves oxygenation in term neonates with severe hypoxemia secondary to PPHN (3–5). Recent reports suggest that a group of preterm infants with severe RDS refractory to surfacant therapy develop pulmonary hypertension any may benefit from iNO therapy (6,7). However, iNO treatment of premature infants with severe RDS is not indicated, because little is known about the beneficial and adverse effects of this therapy and there are no randomized trials demonstrating its efficacy. A modest increase in the levels of blood methemoglobin and exhaled NO2 has been reported after iNO at ≤ 20 ppm in premature infants (6). According to studies in vitro, NO acts as either a pro-oxidant or antioxidant, apparently depending on the concentration of NO and the other oxidants (8,9). NO is oxidized to toxic N2 (10). In addition, NO rapidly reacts with superoxide anions, forming peroxynitrite (ONOO-). Peroxynitrous acid and its decomposition products are highly reactive, promoting lipid peroxidation, nitration of tyrosine, and oxidation of DNA bases (9). On the other hand, NO is a free radical that detoxifies lipid radicals (chain-breaking antioxidants) in vitro (8).
Pulmonary surfactant is a complex containing characteristic phospholipids and proteins. The large surfactant aggregates rich in SP-B and SP-A (11) are surface active and capable of rapid surface adsorption. The small surfactant aggregates, which are deficient in surfactant proteins, are not surface active (11–14). The conversion of large to small surfactant aggregates is thought to be catalyzed by a serine proteinase that degrades surfactant proteins (11–12). This takes place in vitro whenever the surfactant complex is cyclically exposed to the air-liquid interface, mimicking the breathing pattern. Other factors, such as serum proteins and oxygen radicals, may affect the aggregate conversion rate also (14,15). At birth, virtually all alveolar surfactant consists or large aggregates. After the onset of air breathing, small surfactant aggregates increase at the expense of large aggregates (16).
We hypothesized that iNO influences the alveolar lining, particularly during exposure to hyperoxia shortly after premature birth. In this critical transitional stage, the pro-oxidant properties of NO may become evident, because it is metabolized to peroxynitrite or NO2 (9). Alternatively, NO has a potential of protecting the alveolar surface, because it has been shown to decrease surfactant aggregate conversion in vitro (17), and by serving as a free radical scavenger, NO may decrease lipid peroxidation in vitro (8,18). Our aim was to study whether a low dose of iNO affects the surfactant components, alveolar macrophages, and oxidation products in pulmonary alveolar lining of preterm rabbits during exposure to hyperoxia.
METHODS
Materials. The time-mated (± 1 h) pregnant rabbits were purchased from Irish Farms (Orange Country, CA). Formula (Esbilac; Pet-Ag Inc., Hampshire, IL) was supplemented with lactalbumin (4 g/100 mL). All gases used in experiments were of medical grade. Air, O2, N2, and NO were purchased from Scott Specialty Gases (Plumsteadville, PA).
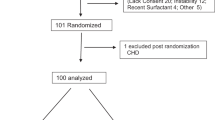
Protocol. The study was performed in an American Association for Accreditation of Laboratory Animal Care approved facility. The protocol was evaluated and approved by the Institutional Review Committee. In total, 152 premature rabbits (29 d gestation, term 31 d) from 18 litters were delivered by hysterotomy. All animals were dried and weighed immediately after birth. They were kept in room air at 28-30°C and fed 60 mL/kg formula by an oral-gastric tube.
At the age of 1 to 2 h, the surviving 114 rabbits were placed in nose-only, nonrebreathing exposure chambers. This system ensures inhalation of known quantities of a gas mixture and minimizes the potential adverse consequences of whole-body exposure to reactive gas mixtures (19). The NO and NO2 concentrations were monitored hourly during the exposure period in the rabbit breathing zone, using a chemiluminescent nitrogen oxide analyzer (Monitor Labs model 8840, Columbia Scientific Instruments, Austin, TX). Total exposures were 20 h. Ambient temperature was maintained between 28 and 30°C using a thermostated enclosure.
Three groups of animals from 14 litters were randomly assigned to be exposed to one of the following environments: group 1: 98% O2 (n = 42); group 2: NO at 14 ppm in 98% O2 (n = 41), and group 3: air (n = 38). Another group of animals from four litters were randomized to be exposed to either air (n = 11) or NO at 14 ppm in air (n = 12). All gases were humidified.
After the exposure, the rabbits were removed from the nose-only exposure chambers, weighed, and rectal temperature was measured with a probe. After anesthesia induced by an i.p. injection of pentobarbital (100 mg/kg), the animals were exsanguinated by intracardiac puncture. The thoracic cage was opened and the trachea cannulated. BAL was performed by instilling the airways with 30-35-mL/kg portions of Ca2+/Mg2+-free HBSS and recovering the lavageate by gentle suctioning. Unless otherwise indicated, the procedure was repeated six times. The volume of the combined BAL fluid was recorded. BAL was centrifuged at 300 × g for 5 min to recover the cell fraction. The cell fraction was washed by suspension in HBSS and centrifugation. The cell-free supernatant was used for surfacant studies.
Eleven animals (O2: n = 4; NO + O2: n = 4; air: n = 3) were not lavaged. Instead, the lungs were processed for histology and studied as described (20).
Study of PAMs. Because of the small number of cells obtained per animal, cells from 4-6 animals exposed to each atmosphere were pooled. An aliquot of BAL cells was prepared by cytocentrifugation and placed on slides. The slides were stained (Diff Quik; Baxter, Irvine, CA) and examined under a light microscope at 400× for differential cell counts. The viability of cells was determined by trypan blue exclusion. The PAMs were diluted to a final concentration of 106 cells/mL for the assay of respiratory burst activity. Respiratory burst activity is a measure of the capacity of phagocytes to generate a burst of superoxide. Respiratory burst activity was measured by lucigenin-amplified chemiluminescence (21). PAMs (0.5 × 106 in 500 µL HBSS) were incubated for 1 h in plastic cuvettes at 37°C, and nonadherent cells were removed with gentle washing. The medium was replaced with 1 mL of HEPES-buffered (pH 7.2) RPMI 1640, and 50 µL 40 mM lucigenin (bis-N-methylacridinium nitrate; Sigma Chemical Co., St. Louis, MO) was added. Opsonized zymosan (Zymosan A from Saccharomyces cerevisae; Sigma) was added to initiate the respiratory burst, and the production of superoxide was measured over a 15-min period using a 25-sample luminometer (model 1250; Pharmacia LKB, Uppsala, Sweden).
Isolation of surfactant aggregates and quantitation of surfactant components. The fraction of large surfactant aggregates was isolated by centrifuging the BAL supernatant at 26 000 × g for 15 min. The resulting pellet was washed once with HBSS, resedimented, and brought into suspension with HBSS. The BAL supernatant contained small surfactant aggregates. PC was quantitated in cell-free BAL, the small-aggregate fraction, and the large-aggregate fraction. The recovery of PC in the surfactant aggregate fractions was 102 ± 6%. The distribution of the large-surfactant-aggregate fraction was expressed as a percentage of total PC.
PC was quantitated using an enzymatic method (22). Briefly, phospholipase D was used to hydrolyze choline, which was oxidized to betaine and H2O2. Subsequent treatment of H2O2 with peroxidase couples 4-aminoantipyrene and 2-hydroxy-3,5-dichlorobenzene sulfonate to yield a chromogen that was quantitated at 510 mm. DPC was measured using the osmium method (23).
SP-B was quantitated buy the method of Kramer et al. (24). Briefly, samples were mixed 1:1 with propanol in polystyrene microplates. The fluid was removed by evaporation. Trifluoroethanol was added to enhance binding of SP-B to polystyrene, and the fluid was again removed by evaporation. Phospholipids were removed by washing a mixture of diisopropyl ether and butanol, followed by 0.05% Tween 20 in PBS. A monoclonal mouse anti-porcine SP-B antibody (a kind gift from Dr. Suzuki, Kyoto, Japan) was bound to the immobilized SP-B. Excess antibody was removed by washing, followed by an addition of biotinylated anti-mouse antibody and an avidin-labelled peroxidase detection system.
For SP-A, the proteins were size separated electrophoretically by the method of Laemmli (25) in an SDS-polyacrylamide gel, with a 12% acrylamide content under reducing conditions. The proteins were electrotransferred to a nitrocellulose membrane according to the method of Towbin et al. (26). After blocking nonspecific binding sites, the membrane was incubated with guinea pig anti-rabbit SP-A (a kind gift from Dr. Snyder, Iowa City, IA), followed by an alkaline phosphatase-conjugated anti-guinea pig antibody, and nitroblue tetrazolium/5-bromo-4-chloro-3-indolyl phosphate color substrate incubation. The immunoreactive spots were quantitated using video densitometry.
Other methods. Total glutathione in BAL was determined using the enzymatic method of Tietze (27). Glutathione disulfide (oxidized glutathione) was determined according to the method described by Adams et al (28) Glutathione was determined in a total of 28 rabbits randomized to be treated in hyperoxia, hyperoxia + NO, or air. At the end of the exposure, the animals were killed as described. Plasma were separated from intracardiac blood. The first BAL return was recovered and immediately centrifuged to separate cells. The cell-free BAL supernatant was used for quantitation of glutathione and TBA-reactive material. In addition, concentrations of urea in plasma and BAL were quantitated using a urea nitrogen kit (Sigma). The concentration in ELF were defined as follows: [glutathione / TBA-reactive material]BAL × [ureaplasma / urea]BAL (29). Nitrotyrosine associated with proteins was measured using immunoassays. The polyclonal nitrotyrosine antibody was from Upstate Biotechnology, Inc. (Lake Placid, NY). The quantitation took place using the ELISA and Western blot techniques. The proteins were separated under reducing conditions using PAGE (25). Total proteins were quantitated as described (30).
The cell-free BAL was analyzed for the content of TBA-reactive material, using malondialdehyde as a standard (31,32). All specimens were stored at -70°C for less than 30 d before the analysis. The content of TBA-reactive material did not increase during the storage at -70°C for 6 mo.
The surface tension was measured using a pulsating bubble surfactometer as described previously (33). The total cell-free BAL was concentrated using a Centricon microconcentrator, cutoff value 3 kD (Amicon, Beverly, MA) The large-aggregate fraction of BAL was obtained by sedimentation of total cell-free BAL at 26 000 × g for 15 min. The PC concentration in each specimen was adjusted to 1.5 µmol/mL. During the measurement of minimum surface tension, the radius of the bubble was varied between 0.40 and 0.55 mm at a frequency of 0.33 Hz and the surface tension with the minimum radius was recorded. For the surface adsorption and equilibrium surface tension measurements, the bubble with a radius of 0.40 mm was formed and the radius was maintained constant for 5 min while the surface tension was continuously monitored. The surface tensions 1 sec and 5 min after formation of bubble were reported. each specimen, representing BAL from one to three animals, was analyzed in duplicate.
Statistics. The data were analyzed by ANOVA to assess the significance of the differences between the three group means. The individual comparisons were further evaluated using the least significant difference procedure of Fisher. The two-tailed t test was used to evaluate the difference between the two group means. A value of p < 0.05 was considered to be significant. Data were analyzed both per specimen and per litter. In either case, the results were very similar. All analyses were performed using the StatView 4.1 computer program (Abacus Concepts, Inc., Berkeley, CA). Group mean ± SEM values are shown.
RESULTS
The premature animals delivered by hysterotomy on d 29 of pregnancy frequently had apnea and chest retractions during the first 1-2 h of life. They were treated with tactic stimulation and were gavage fed first when the respiratory symptoms decreased. Eight of the animals died shortly after birth, leaving 144 animals in the study.
Animals Exposed to O2 (± NO) or Air
There were no statistically significant differences between the three groups in mortality (Table 1). Lung morphology revealed only small abnormalities (localized areas of atelectasis, thick walls of air spaces), and there were no significant differences between the three groups. None of the animals studied had increased numbers of inflammatory cells in the lung. At the end of the exposure, each group of preterm animals demonstrated normal or near-normal rectal temperature. Unlike adult rats exposed to iNO at 100 ppm (33), the preterm rabbits exposed to iNO at 14 ppm showed no evidence of hypothermia. NO2 remained low (< 0.4 ppm) in the breathing area in animals exposed to NO.
Cells in BAL. In animals exposed to hyperoxia, the number of cells in BAL (0.20 ± 0.03 × 106 cells per animal) tended to be lower than in animals breathing room air (0.32 ± 0.04 × 106) or O2 containing NO at 14 ppm (0.30 ± 0.03 × 106), though these differences were not significant. In each group, more than 95% of total cells were PAMs, and less than 5% granulocytes. The respiratory burst activity of PAMs after the activation of phagocytosis by opsonized zymosan tended to be higher in the NO + O2 group compared with the O2 or air groups; these differences were not statistically significant either (data not shown).
Surfactant in BAL. The volumes of BAL returns were similar in each group (O2: 7.2 ± 0.3 mL; NO + O2: 6.9 ± 0.4 mL, air 7.4 ± 0.4 mL). There were no significant differences in the recoveries of PC or DPC in BAL. The recovery of SP-B in the BAL return was decreased in the hyperoxia group compared with the air (p < 0.01) and the NO + O2 groups (p < 0.05). There were no statistically significant differences between the NO + O2 and air groups (Table 2). There was a similar but statistically nonsignificant trend in the content of SP-A. The molecular mass distribution of SP-A under reducing conditions revealed no differences between the groups (Fig. 1).
(A) Representative Western blot depicting immunostaining of SP-A under reducing conditions. The specimens are cell-free bronchoalveolar lavages (5 µg protein), recovered from premature animals that were exposed to hyperoxia. NO and hyperoxia, or air. The molecular-weight standards are shown on the left. (B) Video densitometry analysis of molecular-weight. distribution of immunoactive SP-A: glycosylated SP-A monomer (34-38 kD), deglycosylated SP-A monomer (28 kD), dimeric SP-A (58 kD), and total SP-A. The degree of glycosylation was not analyzed.
The quantity of PC in large surfactant aggregates was highest in animals exposed to room air and lowest in animals exposed to O2: the differences between the three groups were statistically significant (Fig. 2). The distribution of surfactant aggregates was expressed as the proportion of PC present in the large-aggregate fraction as a percentage of total PC in BAL. The proportion of large surfactant aggregates in BAL was significantly decreased in animals exposed to O2 compared with animals exposed to air. There were no significant differences in the amount of large aggregates between the O2 + NO group and the other groups (Fig. 2).
Surface activity. The surface activities of the total cell-free BAL and the large-aggregate fraction of cell-free BAL were studied, as described in "Methods." The minimum surface tension of total cell-free BAL was significantly higher and the surface adsorption rate (i.e. surface tension 1 sec after formation of bubble) significantly lower in the hyperoxia group than in the air or NO + O2 groups. In contrast, in the large-aggregate fraction, there were no detectable differences in the minimum surface tension, in the surface adsorption rate, or in the equilibrium surface tension (i.e. surface tension 5 min after formation of bubble) between the three groups. The large aggregates were surface active (Table 3).
In an attempt to explain the decreased surface activity of cell-free BAL after hyperoxia, the inhibition of surface activity was studied. The cell-free BAL was centrifuged at 105 000 × g for 60 min, and the nonsedimentable supernatant was recovered. The nonsedimentable supernatant was concentrated to a constant protein concentration, and the capacity of these proteins to decrease the surface activity of normal surfactant from adult rabbits' BAL was measured. The conditions were identical to those described previously (33). The nonsedimentable protein from all three groups had a similar capacity to decrease the surface activity of surfactant (data not shown). The concentrations of protein in the nonsedimentable supernatant were similar in all three groups studied, suggesting that neither hyperoxia nor iNO + O2 increased the permeability of proteins across the alveolar epithelium under the present conditions. This observation indicates that the proteinaceous surfactant inhibitors were not affected during the present exposures (but see Ref. 33).
Oxidant stress. To find out whether the present exposures were associated with oxidant stress, some reactive molecules were analyzed in BAL. Nitrotyrosine, i.e. the reaction product between peroxynitrite and tyrosine, was not detectable among the proteins of acellular BAL in any of the groups, suggesting a lack of iNO-induced formation of peroxynitrite. In contrast, exposure to hyperoxia increased the content of TBA-reactive material in ELF (Table 4). The content of TBA-reactive material was higher in animals exposed to hyperoxia than in the air or NO + O2 groups (p < 0.05). In contrast, the content of total glutathione in ELF tended to be lower in animals exposed to O2 than in animals exposed to either air (p < 0.05) or NO + O2 (p = 0.06). Oxidized glutathione was low in ELF (O2: 6 ± 2 nmol/mL; NO ± O2: 7 ± 1 nmol/mL; air: 5 ± 2 nmol/mL).
Animals Exposed to Air
Two groups of premature rabbits were nose-only exposed to air or to 14 ppm NO in air for 20 h. There were no differences in the amount of surfactant components or TBA-reactive material in BAL (Table 5). The percentage distribution of large surfactant aggregates was similar in both groups (air: 48 ± 5% of total PC in large aggregates; NO + air: 61 ± 4% total PC in large aggregates).
DISCUSSION
Hyperoxia and nitric oxide may affect the alveolar lining by causing inactivation of surfactant proteins, peroxidation of surfactant lipids, and a decrease in surface activity. Specifically, hydroxyl radicals produced from superoxide in the Fenton reaction (32,34) and peroxynitrite produced from superoxide and nitric oxide (9) have been shown to deteriorate surface activity in vitro. Inactivation of surfactant is associated with peroxidation of surfactant lipids and with characteristically altered surfactant proteins (such as nitration tyrosine residues by peroxynitrite) (35,36). Premature lung, deficient in many antioxidants, may be prone to oxidant stress (37).
In the present study we investigated whether a brief inhalation of O2 or NO (14 ppm) after premature birth leads to changes in the surfactant system. Prolonged inhalation that would increase mortality or cause histologic evidence of lung injury was not attempted. Exposure of preterm rabbits to hyperoxia (98% O2 for 20 h) decreased the large-surfactant-aggregate fraction of BAL. There was a parallel decrease in SP-B and a decrease in surface activity of the total cell-free BAL. The surfactant abnormality after hyperoxia was not severe enough to cause significant atelectasis or fatal respiratory failure. Surprisingly, inhaled NO at low concentration prevented or decreased these hyperoxia-induced changes in the surfactant, which was shown by the fact that iNO protected against the hyperoxia-induced decrease in SP-B, decreased the conversion of large to small surfactant aggregates, and prevented the decrease in the surface activity. In premature animals breathing room air, a brief exposure to iNO at 14 ppm had no detectable effect on the alveolar lining.
Hyperoxia has a biphasic effect on alveolar surfactant in adults: an early decrease in the surfactant pool is followed by an increase in lavageable surfactant and increase in proteinaceous surfactant inhibitors (38,39). In preterm rabbits, there was no detectable increase in alveolar surfactant phospholipid and a modest increase in surfactant inhibitors during hyperoxia for 4 d (20). In the present study, a brief hyperoxia decreased SP-B, decreased the large surfactant aggregates at the expense of small surfactant aggregates, and decreased surface activity without a significant increase in proteinaceous surfactant inhibitors. This finding is in agreement with previous observations in adult animals showing a decrease in large surfactant aggregates during oxidant injury (14,40). The fact that in premature lung, TBA-reactive material increased and glutathione decreased in ELF in parallel with the decrease in surface activity indicates that oxidant stress was associated with surfactant dysfunction.
According to some animal studies, NO (endogenous or inhaled) enhances the detrimental effects of hyperoxia (33,41,42). In one study, newborn piglets were exposed to 100 ppm iNO for 48 h (41). This procedure caused a significant surfactant dysfunction and evidence of pulmonary inflammation, including accumulation of neutrophils. Furthermore, exposure of adult rats to a low concentration of NO (1-2 ppm) for 9 wk (43) was associated with alveolar and interstitial emphysematous changes. Either the concentration (41) or duration of iNO (43) was one order of magnitude more extensive than in the present study, showing no change in inflammatory cells. In contrast, in another study, a brief exposure to iNO (20 ppm for 4 h) decreased neutrophil accumulation into ventilated ovine lung in severe RDS (44).
Nitric oxide can be harmful or protective, depending on the concentration and duration of exposure and on the presence of other molecules (9). Several mechanisms may explain the protective effects of iNO against oxidant stress. First, NO as a weak radical acts as a scavenger of lipid radicals in vitro (8) and may thus terminate the cascade leading to lipid peroxidation. NO as a lipophilic agent is likely to concentrate within surfactant aggregates. In contrast, superoxide required for the formation of peroxynitrite is notably hydrophilic. Inhibition of superoxide production by neutrophils (45) and reactions of NO inhibiting the function of ferrous iron as a transient metal (46) are some other potential protective mechanisms against free oxygen radicals. The hypothesis that iNO during hyperoxia served as an antioxidant is supported by the iNO-induced decrease in TBA-reactive material in ELF. Although the formation of peroxynitrite in the presence of iNO may be anticipated in the premature lung, we did not detect nitrotyrosine in BAL, and there was only a modest increase of NO2 in the breathing area during iNO.
NO and NO donors have been shown to increase reduced glutathione in the rat lung fibroblast cell line (RFL6 cells), in bovine pulmonary arterial smooth muscle cells, and in endothelial cells (47). In the present study, acute hyperoxia decreased total and reduced glutathione in ELF, whereas iNO prevented the hyperoxia-induced decrease in glutathione. Apart from intracellular synthesis, the concentrations of glutathione in ELF may be determined by the release of glutathione from alveolar cells, by the intracellular uptake, and by the metabolism (including oxidation) of glutathione. The exceptionally slow uptake of reduced glutathione from ELF by lung cells has been postulated to be a mechanism of the remarkably high concentration of glutathione in ELF (48). The pathways that alter the concentrations of glutathione in ELF during hyperoxia and during iNO remain to be identified.
A decrease of capillary leak (49,50) and a decrease of neutrophil and platelet aggregation (49) by NO are other potential mechanisms protecting against lung injury. Neither the nonsurfactant protein content in BAL nor its capacity to decrease surface activity was affected by iNO in the present study. In contrast, we found differences in the alveolar surfactant that were associated with iNO and hyperoxia.
The mechanism of iNO in protecting against hyperoxia-induced depletion of SP-B and large surfactant aggregates is currently unknown. SP-B is essential for surfactant function. Together with SP-B, SP-A is indispensable for the integrity of large surfactant aggregates, particularly tubular myelin (11,13,51). According to one possibility, the protection of NO against alveolar surfactant inactivation in situ is due to NO-induced inhibition of surfactant aggregate conversion, found during surface cycling (17). The finding of a simultaneous decrease in TBA-reactive material suggests that the surfactant protection and the antioxidant effect by iNO are linked. Other possible pathways whereby iNO protects against surfactant inactivation remain to be studied.
Hyperoxia is known to prevent the neonatal increase in PAMs (52). In the present study, iNO prevented the hyperoxia-induced trend toward a decrease in the number of PAMs. In addition, iNO tended to increase the respiratory burst activity in vitro. None of these effects were statistically significant. Nitric oxide is known to decrease macrophage NO synthase activity. Suppression of endogenous NO synthesis would prolong the half-life of superoxide generated in vitro, artificially increasing superoxide and respiratory burst activity. The apparent increase in respiratory burst activity by PAMs after iNO may therefore be due to NO-induced prolongation of the half-life of superoxide. Abnormalities in inflammatory cells caused by suppression of NO synthase are likely to affect both the microbicidal and endotoxic properties of inflammatory cells (9).
The present finding that iNO shortly after premature birth protects against oxidant stress and surfactant inactivation does not justify the use of NO in treatment of RDS. The dose responsiveness of iNO and the dependence of iNO effect on the degree of immaturity remain to be studied further (53). A high concentration of or prolonged exposure to iNO in hyperoxia is likely to be detrimental, as a result of the toxicity (peroxynitrite, NO2, methemoglobin) (10,33,41) or other mechanisms (prolongation in bleeding time, inhibition of endogenous NO synthesis, induction of symptomatic ductus arteriosus). Despite these reservations, the present findings support the proposal to study the efficacy and safety of iNO to premature infants in PPHN (6,7) and in severe RDS (53).
Abbreviations
- NO:
-
nitric oxide
- iNO:
-
inhaled NO
- BAL:
-
bronchoalveolar lavage
- SP:
-
surfactant protein
- PPHN:
-
persistent pulmonary hypertension of newborn
- RDS:
-
respiratory distress syndrome
- HBSS:
-
Hanks' balanced salt solution
- PAM:
-
pulmonary alveolar macrophage
- PC:
-
phosphatidylcholine
- DPC:
-
disaturated PC
- ELF:
-
epithelial lining fluid
- TBA:
-
thiobarbituric acid
References
Ignarro LJ, Buga GM, Wood KS, Byrns RE, Chaudhuri G 1987 Endothelium-derived relaxing factor produced and released from artery is nitric oxide. Proc Natl Acad Sci U S A 84: 9265–9269
Palmer RMJ, Ferrige AG, Moncada S 1987 Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor. Nature 327: 524–526
Roberts JD, Polander DM, Lang P, Zapol WM 1992 Inhaled nitric oxide in persistent pulmonary hypertension of the newborn. Lancet 340: 818–819
Kinsella JP, Neish SR, Schaffer E, Abman SH 1992 Low-dose inhalational nitric oxide in persistent pulmonary hypertension of the newborn. Lancet 340: 819–820
Finer NN, Etches PC, Kamstra B, Tierney AJ, Peliowski A, Ryan CA 1994 Inhaled nitric oxide in infants referred for extracorporeal membrane oxygenation: dose response. J Pediatr 124: 302–308
Peliowski A, Finer N, Etches PC, Tierney AJ, Ryan CA 1995 Inhaled nitric oxide for premature infants after prolonged rupture of the membranes. J Pediatr 126: 450–453
Abman S, Kinsella J, Schaffer M, Wilkening R 1993 Inhaled nitric oxide in the management of a premature newborn with severe respiratory distress and pulmonary hypertension. Pediatrics 92: 606–609
Rubbo H, Radi R, Trujillo M, Telleri R, Kalyanaraman B, Barnes S, Kirk M, Freeman B 1994 Nitric oxide regulation of superoxide and peroxynitrite-dependent lipid peroxidation. J Biol Chem 269: 26066–26075
Crow JP, Beckman JS 1995 The role of peroxynitrite in NO-mediated toxicity. Curr Top Microbiol Immunol 196: 57–73
Gaston B, Drazen JM, Loscalzo J, Stamler JS 1994 The biology of nitrogen oxides in the airways. Am J Respir Crit Care Med 149: 538–551
Veldhuizen RAW, Hearn SA, Lewis JF, Possmayer F 1994 Surface-area cycling of different surfactant preparations: SP-A and SP-B are essential for large-aggregate integrity. Biochem J 300: 519–524
Gross NJ, Schultz RM 1990 Serine proteinase requirement for the extra-cellular metabolism of pulmonary surfactant. Biochim Biophys Acta 1044: 222–230
Gross NJ, Narine KR 1989 Surfactant subtype in mice: characterization and quantitation. J Appl Physiol 66: 342–349
Ueda T, Ikegami M, Jobe A 1994 Surfactant subtypes, in vitro conversion, in vivo function, and effects of serum proteins. Am J Respir Crit Care Med 149: 1254–1259
Ryan SF, Ghassibi Y, Liau DF 1991 Effects of activated polymorphonuclear leukocytes upon pulmonary surfactant in vitro. Am J Respir Cell Mol Biol 4: 33–41
Baritussio A, Alberti A, Quaglino D, Pettenazzo A, Dalzoppo D, Sartori L, Pasquali-Ronchetti I 1994 SP-A, SP-B, and SP-C in surfactant subtypes around birth: reexamination of alveolar life cycle of surfactant. Am J Physiol 266: L436–L447
Hallman M, Bry K, Lappalainen U 1996 A mechanism of nitric oxide-induced surfactant dysfunction. J Appl Physiol 80: 2035–2043
Wink DA, Cook JA, Krishna MC, Hanbauer I, DeGraff W, Gamson J, Mitchell JB 1995 Nitric oxide protects against alkyl peroxide-mediated cytotoxicity: further insights into the role nitric oxide plays in oxidative stress. Arch Biochem Biophys 319: 402–407
Kleinman M, Bhalla D, Ziegler B, Bucher-Evans S, McClure T 1993 Effects of inhaled fine particles of ozone on pulmonary macrophages and epithelia. Inhal Toxicol 5: 371–388
Bany-Mohammed FM, Slivka S, Hallman M 1996 Recombinant human erythropoietin: possible role as an antioxidant in premature rabbits. Pediatr Res 40: 381–387
Nadziejko C, Nansen L, Mannix R, Kleinman M, Phalen R 1992 Effect of nitric acid vapor on the response to inhaled ozone. Inhal Toxicol 4: 343–358
McGowan MW, Artiss JD, Zak B 1982 A procedure for the determination of high-density lipoprotein choline-containing phospholipids. J Clin Chem Clin Biochem 20: 807–812
Mason RJ, Nellenbogen J, Clements JA 1976 Isolation of disaturated phosphatidyl-choline with osmium tetroxide. J Lipid Res 17: 281–284
Kramer HJ, Shmidt R, Gunther A, Becker G, Suzuki Y, Seeger W 1995 ELISA technique for quantification of surfactant protein B (SP-B) in bronchoalveolar lavage fluid. Am J Respir Crit Care Med 152: 1540–1544
Laemmli UK 1970 Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature 227: 680–685
Towbin H, Staehelin T, Gordon J 1979 Electrophoretic transfer of proteins from polyacrylamide gels to nitrocellulose sheets: procedures and some applications. Proc Natl Acad Sci U S A 76: 4350–4354
Tietze F 1969 Enzymic method for quantitative determination of nanogram amounts of total and oxidized glutathione: applications to mammalian blood and other tissues. Anal Biochem 27: 502–522
Adams JD Jr, Lautenburg BH, Mitchell JR 1983 Plasma glutathione disulfide in the rat: regulation and response to oxidative stress. J Pharmacol Exp Ther 227: 749–754
Hallman M, Merritt TA, Akino T, Bry K 1991 Surfactant protein A, phosphatidylcholine, and inhibitors in epithelial lining fluid: correlation with surface activity, severity of RDS and outcome of small premature infants. Am Rev Respir Dis 144: 1376–1384
Smith PK, Krohn RI, Hermanson GT, Mallia AK, Gartner FH, Provenzano MD, Fujimoto EK, Goeke NM, Olson BJ, Klenk DC 1985 Measurement of protein using bicinchoninic acid. Anal Biochem 150: 76–85
Rowley D, Gutteridge C, Blake D, Farr M, Halliwell B 1984 Lipid peroxidation in rheumatoid arthritis: thiobarbituric acid-reactive material and catalytic iron salts in synovial fluid from rheumatoid patients. Clin Sci (Colch) 66: 691–695
Hallman M, Sarnesto A, Bry K 1994 Interaction of transferrin saturated with iron with lung surfactant in respiratory failure. J Appl Physiol 77: 757–766
Hallman M, Waffarn F, Bry K, Turbow R, Kleinman MT, Mautz WJ, Rasmussen RE, Bhalla DK, Phalen RF 1996 Surfactant dysfunction after inhalation of nitric oxide. J Appl Physiol 80: 2026–2032
Gilliard N, Heldt GP, Loredo J, Gasser H, Redl H, Merritt TA, Spragg RG 1994 Exposure of the hydrophobic components of porcine lung surfactant to oxidant stress alters surface tension properties. J Clin Invest 93: 2608–2615
Haddad IY, Ischiropoulos H, Holm BA, Beckman JS, Baker JR, Matalon S 1993 Mechanisms of peroxynitrite-induced injury to pulmonary surfactants. Am J Physiol 265: L555–L564
Haddad IY, Crow JP, Hu P, Ye Y, Beckman J, Matalon S 1994 Concurrent generation of nitric oxide and superoxide damages surfactant protein A. Am J Physiol 267: L242–L249
Frank L, Sosenko IR 1991 Failure of premature rabbits to increase antioxidant enzymes during hyperoxic exposure: increased susceptibility to pulmonary oxygen toxicity compared with term rabbits. Pediatr Res 29: 292–296
Holm BA, Notter RH, Leary JF, Natalon S 1987 Alveolar epithelial changes in rabbits after 21-day exposure to 60% O2 . J Appl Physiol 62: 2230–2236
Nogee LM, Wispé JR, Claris JC, Whitsett JA 1989 Increased synthesis and mRNA of surfactant protein A in oxygen-exposed rats. Am J Respir Cell Mol Biol 1: 119–125
Higuchi R, Lewis J, Ikegami M 1992 In vitro conversion of surfactant subtypes is altered in alveolar surfactant isolated from injured lungs. Am Rev Respir Dis 145: 1416–1420
Robbins CG, Davis JM, Merritt TA, Amirkhanian JD, Sahgal N, Morin FC III, Horowitz S 1995 Combined effects of nitric oxide and hyperoxia on surfactant function and pulmonary inflammation. Am J Physiol 269: L545–L550
Nozik ES, Huang Y-CT, Piantadosi CA 1995 L-Arginine enhances injury in the isolated rabbit lung during hyperoxia. Respir Physiol 100: 63–74
Mercer RR, Costa DL, Crapo JD 1995 Effects of prolonged exposure to low doses of nitric oxide or nitrogen dioxide on the alveolar septa of the adult rat lung. Lab Invest 73: 20–28
Kinsella JP, Parker TA, Galan H, Sheridan BC, Halbower AC, Abman SH 1997 Effects of inhaled nitric oxide on pulmonary edema and lung neutrophil accumulation in severe experimental hyaline membrane disease. Pediatr Res 41: 457–463
Clancy RM, Leszzynska-Piziak J, Abramson SB 1992 Nitric oxide, an endothelial cell relaxation factor, inhibits neutrophil superoxide anion production via a direct action on the NADPH oxidase. J Clin Invest 90: 1116–1121
Kanner J, Harel S, Granit R 1991 Nitric oxide as an antioxidant. Arch Biochem Biophys 289: 130–136
White AC, Maloney EK, Boustani MR, Hassoun PM, Fanburg BL 1995 Nitric oxide increases cellular glutathione levels in rat lung fibroblasts. Am J Respir Cell Mol Biol 13: 442–448
Cantin AM, North SL, Hubbard RC, Crystal RG 1987 Normal alveolar epithelial lining contains high levels of glutathione. J Appl Physiol 63: 152–157
Benzing A, Brautigam P, Geiger K, Loop T, Beyer U, Moser E 1995 Inhaled nitric oxide reduces pulmonary transvascular albumin flux in patients with acute lung injury. Anesthesiology 83: 1153–1161
Poss WB, Timmons OD, Farrukh IS, Hoidal JR, Michael JR 1995 Inhaled nitric oxide prevents the increase in pulmonary vascular permeability caused by hydrogen peroxide. J Appl Physiol 79: 886–891
Hawgood S, Benson BJ, Schilling J, Damm D, Clements JA, White RT 1987 Nucleotide and amino acid sequences of pulmonary surfactant protein SP 18 and evidence for cooperation between SP 18 and SP 28:36 in surfactant lipid adsorption. Proc Natl Acad Sci U S A 84: 66–70
Sherman MP, Evans MJ, Campbell LA 1988 Prevention of pulmonary alveolar macrophage proliferation in newborn rabbits by hyperoxia. J Pediatr 112: 782–786
Kinsella JP, Ivy DD, Abman SH 1994 Inhaled nitric oxide lowers pulmonary vascular resistance and improves gas exchange in severe experimental hyaline membrane disease. Pediatr Res 36: 402–408
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Issa, A., Lappalainen, U., Kleinman, M. et al. Inhaled Nitric Oxide Decreases Hyperoxia-Induced Surfactant Abnormality in Preterm Rabbits. Pediatr Res 45, 247–254 (1999). https://doi.org/10.1203/00006450-199902000-00016
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199902000-00016
This article is cited by
-
Early use of combined exogenous surfactant and inhaled nitric oxide reduces treatment failure in persistent pulmonary hypertension of the newborn: a randomized controlled trial
Journal of Perinatology (2021)
-
Inhaled nitric oxide alleviates hyperoxia suppressed phosphatidylcholine synthesis in endotoxin-induced injury in mature rat lungs
Respiratory Research (2006)
-
Activation of macrophage nuclear factor-κB and induction of inducible nitric oxide synthase by LPS
Respiratory Research (2002)