Abstract
The prevention of cerebral palsy and neuroprotection of the immature brain continue to be health care priorities. The pathophysiology of perinatal brain lesions associated with cerebral palsy seems to be multifactorial and includes pre- and perinatal factors such as preconceptional events, hormone and growth factors deficiencies, maternal infections with production of cytokines, and hypoxic/ischemic perfusion failures. Excitotoxic cascade could represent a common pathway that leads to neural cell death and subsequent brain damage. Brain injuries induced by ibotenate, a glutamatergic analog, which are essentially mediated through the N-methyl-D-aspartate receptor, mimic some aspects of the white matter cysts and transcortical necrosis observed in human perinatal brain damage. The purpose of the present study was to assess the protective role of several pharmacological agents, administered in conjunction with ibotenate, against induced excitotoxic lesions. We injected ibotenate in the developing mouse brain 5 d postnatally, after the full settlement of neuronal layers. Co-treatment with kynurenic acid, and antagonist of the facilitating glycine site of the N-methyl-D-asparate receptor, or with NG-nitro-L-arginine, an inhibitor of nitric oxide synthesis, induced a dose-dependent neuroprotective effect. Conversely, zinc gluconate, a blocking agent of the channel linked to the N-methyl-D-aspartate receptor, and a free radical scavenger (U74389F), were unable to protect the developing brain against excitotoxic attack. These data help to clarify some molecular mechanisms involved in excitotoxic lesions of the developing mouse brain and permit us to envision new strategies in the prevention of cerebral palsy.
Similar content being viewed by others
Main
In perinatal medicine, the protection of the developing brain of the premature or at-term newborn will prove a challenge for the coming decade. The main causes of cerebral palsy are periventricular leukomalacias in premature infants and cortico-subcortical strokes in term infants(1–3). Epidemiological studies have identified several pre- and perinatal conditions associated with cerebral palsy, including chorioamnionitis, maternal infection, growth factor and hormone deprivations, nutritional deficiencies, and hypoxic-ischemic failures(2,4–6). However, the precise molecular mechanisms leading to brain lesions associated with cerebral palsy remain largely unclear. Hypoxic-ischemic strokes are mediated, in part, by excess release of glutamate and the subsequent excitotoxic cascade(7–9). A limited number of experimental paradigms have addressed the pathophysiology of periventricular leukomalacias. For example, Gilles et al.(10) and Yoon et al.(11), who administered lipopolysaccharide to pregnant cats or Escherichia coli to pregnant rabbits, observed white matter lesions in the offspring, whereas Yoshioka et al.(12) reported the occurrence of white matter damage in Beagle pups subjected to hypoxic-ischemic insults. Furthermore, several groups have studied the toxicity of glutamate analogs on oligodendrocytes(13–15) as a mechanism that may be involved in periventricular leukomalacia.
We recently established an animal model of excitotoxic lesions in the developing mouse brain(16). Brain damages were induced by ibotenate, a glutamatergic agonist, and were highly dependent upon the stage of brain maturation. Neuronal death in cortical layers V-VI was observed when ibotenate was administered at postnatal day (P) O-P2. In contrast, ibotenate injected between P5 and P15 killed neurons in all cortical layers. Furthermore, ibotenate induced periventricular white matter lesions between P2 and P10, with a peak of intensity and frequency at P5. These white matter lesions were initially cystic and progressively evolved toward a glial scar. Although ibotenate is able to activate both NMDA and metabotropic glutamate receptors, all ibotenate-induced brain lesions in this murine model were inhibited by co-treatment with a specific NMDA antagonist (D,L-2-amino-7-phosphoheptanoic acid) but not by an antagonist of phosphoinositide-linked metabotropic glutamate receptors [L(+)-2-amino-3-phosphonopropionic acid]. Furthermore, (RS)-3,5-dihydroxyphenylglycine, a selective agonist of mGluR1 and mGluR5 metabotropic receptors, did not produce any lesions similar to those caused by the ibotenate injections(16–18).
Our model and others permitted several contributions: 1) The sensitivity of the developing rodent brain to NMDA neurotoxicity parallels the sensitivity to hypoxic-ischemic insults(7,8). 2) Agents blocking NMDA receptors are neuroprotective in several models of neonatal hypoxic-ischemic insults(8,19). 3) Ibotenate-induced white matter lesions are periventricular and cystic, and they evolve toward a glial scar. 4) The developing murine white matter exhibits a discrete ontogenic window of sensitivity to ibotenate-induced damages as observed in humans. Furthermore, the asynchronism of the ontogenic windows between the ibotenate-induced cortical plate damages (PO to adult) and the cystic white matter lesions (P2 to P10), combined with the fact that melatonin(20) and vasoactive intestinal peptide(21) protect the white matter, but not the cortical plate, against ibotenate, strongly suggest that white matter lesions are not secondary to cortical plate lesions. Our ibotenate model, applied at consecutive developmental steps, therefore represents a well-defined tool permitting approach to several pathophysiological mechanisms potentially involved in perinatal brain damages. All animal models in the field are contributive but oversimplify the problems; multiple models and critical applications are requested to reduce the oversimplifications.
The aim of the present study was to investigate with the ibotenate model the protective effects of several modulators of the NMDA-mediated excitotoxic cascade and to approach some pathways in excitotoxic lesions of developing brain.
MATERIAL AND METHODS
Model description. Pregnant NMRI mice were housed in groups after mating and were fed with laboratory chow and food ad libitum. Different litters of postnatal 5-d-old pups of both sexes were used for the experiments. Experiment protocols were approved by the institutional review committee and meet the guidelines of the Institut National de la Santé et de la Recherche Médicale.
Pups were anesthetized with ether inhalation under a warning lamp. Intracerebral injections of ibotenate (Sigma Chemical Co., St. Louis, MO), diluted in 0.02% acetic acid -0.1 M PBS or of PBS-acetic acid alone were performed at postnatal day (P) 5 with a 26-gauge needle on a 50-µl Hamilton syringe mounted on a calibrated dispenser. The needle was inserted 2 mm under the external surface of scalp skin in the fronto-parietal area of the right hemisphere 2 mm from the coronal suture in the lateral-medial plane and 3 mm from the sagittal suture in the rostrocaudal plane. Two 1-µL boluses of 5 µg each were injected at a 60-s interval, with the needle being left in place for an additional 30 s. In all of these experiments, the tip of the needle reached the white matter, confirmed by injecting some animals with toluidine blue. The pups were allowed to recover from anesthesia, and their temperature was measured orally by a thermometer both 5 min and 1 h after injection of the antagonist to ensure that any potential protective protective effect was not due to hypothermia. Five days later, the surviving pups were killed under ether anesthesia, by intracardial perfusion with 4% paraformaldehyde. The brains were removed and postfixed in the same fixative solution for an additional 24 h at 4°C.
After fixation, the brains were dehydrated in alcohol and embedded in paraffin. Coronal serial sections, 10 µm thick, were cut, and every third section was stained with cresyl-violet. The brain was completely and serially sectioned from the frontal pole to the occipital lobes(16,21). This permitted an accurate and reproducible measurement of the maximal sagittal fronto-occipital diameter (which is equal to the number of sections where the lesion was present, multiplied by 10 µm) of the ibotenate-induced cortical lesions. In subsequent sections of this paper, this maximal diameter will be referred to as the length of the lesion in the frontoparietal axis and will be used as an index of the lesion.
Experimental groups. Four types of molecules were intraperitoneally injected 10-15 min intracerebral ibotenate administration: 2, 10, or 20 mg/kg of Kyn (7-chloro-thiokynurenic acid) (Tocris Cookson, Bristol, UK), an antagonist of the facilitating glycine site of the NMDA receptor; 0.2, 1, or 2 mg/kg NG-nitro-L-arginine (NOARG) (Sigma Chemical Co., St. Louis, MO), an inhibitor of all types of NO° synthase; 1, 10, or 30 mg/kg zinc gluconate, an inhibitor of calcium influx through binding at the zinc site of the NMDA receptor complex; 0.3, 1, or 10 mg/kg 21-aminosteroid (U74389F) (compliments of UPJOHN Wellcome, Beckenham, UK), a free radical scavenger. Control animals received intraperitoneal PBS. In another set of control experiments, the effect of the highest dose of each putative neuroprotective agent was tested in animals intracerebrally injected with PBS. Each experimental groups was composed of between 9 and 16 pups which were treated in two or more successive experiments.
Statistical analysis. Statistical analysis were performed by ANOVA with Dunnet's multiple comparison of means test when appropriate. Results were expressed as mean ± SEM. Differences were considered significant when the p value was less than 0.05.
RESULTS
During the first 24 h after the sole ibotenate injection, animals generally developed clonic seizures and tonic spasms. After coinjection of ibotenate with Kyn or NOARG, pups showed a reduced frequency of abnormal motor manifestations. NO additional clinical side effect could be detected in animals coinjected with ibotenate and Kyn or NOARG. On the other hand, most pups injected with ibotenate and with zinc or 21-aminosteroids appeared to be very hypotonic for a few hours after treatment. The mortality rate was comparable in all experimental groups (Table 1), except for the group treated with 30 mg/kg zinc. In that group, all pups died within 24 h after injections. Control groups that received both intraperitoneal Kyn, zinc, lazaroid, or NOARG and intracortical PBS did not develop cerebral brain lesions (data not shown). No significant differences in temperature before and after Kyn, zinc, or lazaroid injections could be found, whereas a significant elevation of temperature was observed after the injection of NOARG (Table 2).
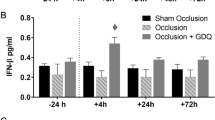
As previously described, all P5 animals co-treated with ibotenate and intraperitoneal PBS showed focal brain damage consisting of a cortical necrosis affecting all neuronal layers and an underlying periventricular white matter cyst (Fig. 1A). When Kyn or NOARG were intraperitoneally injected 10-15 min after ibotenate administration, both the cortical plate and white matter were protected against the excitotoxic lesions (Fig. 1B-D). The quantitative assessment of the length of the cortical plate lesion in the frontoparietal axis confirmed a significant dose-dependent neuroprotective effect of these two drugs (28%, 53%, and 75% decrease of the mean length of the lesion with 2, 10, and 20 mg/kg Kyn, respectively; 24%, 43%, and 78% decrease with 0.2, 1, and 2 mg/kg NOARG, respectively) (Fig. 2A-B). Co-treatment of pups with ibotenate and U74389F or zinc did not protect the developing brain against excitotoxic damages (Fig. 1E-F and 2C-D). A nonsignificant (20-25%) dose-independent decrease of the mean length of the cortical plate lesion was observed with U74389F administration (Fig. 2C).
Light-microscopic examinations of cresyl-violet-stained coronal sections of brains injected with ibotenate at P5 under different experimental conditions and studied at P10. (A) Brain injected with ibotenate alone, showing the typical neuronal loss in layers II-VI (arrow) and the white matter cystic lesion (*); (B) brain cotreated with ibotenate and 20 mg/kg kynurenic acid, showing no detectable lesion; (C) brain cotreated with ibotenate and 10 mg/kg kynurenic acid, showing a small lesion; (D) brain cotreated with ibotenate and inhibitor of 2 mg/kg NO synthase, showing a small lesion; (E) brain cotreated with ibotenate and 10 mg/kg U74389F, showing a typical brain lesion; (F) brain cotreated with ibotenate and 10 mg/kg zinc gluconate, showing a huge typical brain lesion. Bar = 200 µm.
Measurements of the ibotenate-induced brain lesions. Bar represents length of the neocortical lesion in the sagittal fronto-occipital axis (mean ± SEM). Asterisks indicate difference from control coinjected with ibotenate and PBS (control) (*p < 0.05, ***p < 0.01 in ANOVA with Dunnet's multiple comparison test). (A) Size of the lesions observed after coinjection with ibotenate and kynurenic acid; (B) size of the lesions observed after coinjection with ibotenate and inhibitor of NO synthase; (C) size of the lesions observed after coinjection with ibotenate and U74389F; (D) size of the lesions observed after coinjection with ibotenate and zinc gluconate.
DISCUSSION
The present study demonstrates that systemically injected Kyn or NOARG significantly protected the developing mouse brain from neocortical gray and white matter ibotenate-induced damage, whereas zinc and U74389F had no significant neuroprotective effect, although a trend to reduce brain damage was observed with co-administration of U74389F. Although hypothermia has been reported to protect the developing brain against hypoxic-ischemic insults(22,23), the neuroprotection induced by Kyn and NOARG was not due to such hypothermic effect. Indeed, Kyn did not affect body temperature, whereas NOARG significantly increased the body temperature of newborn mice.
In the developing brain, the excessive stimulation of the ionotropic NMDA receptor by glutamate results in a cascade of cellular events eventually leading to neural cell death. This excitotoxic cascade could, theoretically, be antagonized by pharmacological agents at different steps of this cascade. Such candidate protective molecule could target the presynaptic release of glutamate, the NMDA receptor complex linked to the ion channel located on the postsynaptic membrane, the free radical synthesis in the cell cytosol, the oxydative phosphorylation disruption in the mitochondria, or the gene apoptosis activation in the nucleus. The changing subunit composition of heteromeric NMDA receptors and the maturation of neural metabolic pathways imply, however, that the candidate molecules should not show the same efficacy at successive steps of brain development(24). The diversity of NMDA receptor properties in different neural cells is explained by the developmental regulation of NMDA receptor subunit I (NR1) splice variants and of the NR2 subunits, NR2-A to D. NR2-B subunits, which are sensitive to magnesium, zinc, and glycine, are present in P7 rat brain(25,26).
Kyn is an antagonist of the facilitating glycine site and is the only known endogenous antagonist of excitatory amino acid receptors. In rat brain, the amount of endogenous Kyn progressively increases during prenatal life before decreasing after birth(27). The ability of the immature brain to activate endogenous Kyn production could play a role in the brain response to perinatal injury(28). In a previous model of hypoxia-ischemia in 1-week-old rats, exogenous Kyn also provided neuroprotection(29). Our in vivo study confirms the importance of the glycine site of the NMDA receptor in the developing brain at P5 in a murine model.
During cerebral ischemia, inflammation, or excitotoxicity, NO° production through NMDA receptor stimulation and subsequent NO° synthase activation probably plays a pivotal role in neuronal death(30). NOARG is a nonselective inhibitor of the three isoforms of NO° synthases (endothelial, neuronal, and immunoactivated)(31). It competitively inhibits the enzymatic formation of NO° in cultured endothelial cells(32), prevents NMDA-induced toxicity in cultures of cortical neurons(30),) and crosses the blood brain barrier(31). NO° synthase expression and activity increase during gestation in guinea pigs, rats, and mice, to reach significant levels in the first postnatal days, and they exhibit adult patterns by the second postnatal week(33). Conflicting results have been published on the effects of NO° synthase inhibition during brain ischemia or hypoxic-ischemic insults. Inhibition of NO° synthase by NOARG is deleterious in adult focal cerebral ischemia(34). NOARG injected before unilateral hypoxicischemic transient challenge protects 7-d-old rats from brain injury, whereas it is ineffective if administered after the same insult(35). The level of NO° synthase inhibition could be critical, because there seems to be an optimal dose of inhibitor for neuroprotection in lambs(36). In our P5 mouse excitotoxic model, NOARG, when administered directly after excitotoxic injury, was able to decrease both gray and white matter injuries, emphasizing the toxic role of NO° at early steps of the excitotoxic cascade. As previously mentioned, this protective effect was obtained in spite of an increase in brain temperature which accentuates ischemic brain damage(37). Although the exact mechanism of this NOARG-induced body temperature is unclear, large amounts of NO° synthase activity are present in the hypothalamus, which is the center of body temperature control(38).
The lack of significant protective effect of U74389F in our model of excitotoxic brain lesions could be due to its inability to pass through the blood-brain barrier, to achieve sufficient concentration near the site of free radical generation, or to compete efficiently with endogenous targets of free radical attacks (membranes and DNA). The possibility of a hemodynamic side effect cannot be eliminated. In a neonatal rat model of cerebral hypoxia-ischemia, the same molecule had no detectable protective effect(39). In most of the reported studies, free radical scavengers have been shown to attenuate, but not to block, excitotoxic neuronal death(40–41). In this regard, carboxyfullerenes, polyhydroxylated malonic acid derivatives of C60, seem more promising as a challenge to free radical-induced brain damage, probably because of their ability to react with both superoxide and hydroxyl radicals(42).
An inhibitory zinc site is present in the calcium channel linked to the NMDA receptor complex. Zinc is also present in the synaptic vesicles of central excitatory neurons and is released with synaptic activity or membrane depolarization. A variety of studies have suggested that zinc may inhibit excitatory transmission(43). On the other hand, zinc chelating agents prevent excitotoxic neuronal death after transient global ischemia, suggesting that extracellular zinc has a toxic effect(44). A differential expression of NMDA-receptor subunits during brain development could explain the different zinc sensitivity(43). Zinc also enhances inhibitory synaptic transmission and the release of γ-aminobutyric acid(45). All of these data demonstrate the difficulty in predicting the potential effects of exogenous zinc on neural cells, which thus could explain the lack of efficacy of zinc in our animal model.
In conclusion, this study demonstrates that a glycine antagonist and an NO° synthase inhibitor prevent brain lesions that, in our view, mimic some aspects of periventricular leukomalacias and strokes observed in human premature or term newborns. These data contribute additional information to our understanding of the pathophysiological mechanisms involved in excitotoxic diseases of the developing brain, and they delineate new potential avenues in the prevention of cerebral palsy.
Abbreviations
- P :
-
postnatal day
- NMDA :
-
N-methyl-D-aspartate
- NMRI :
-
Naval Medical Research Institute
- Kyn :
-
kynurenic acid
- NR1 :
-
NMDA receptor subunit 1
- NR2-A to D :
-
NMDA receptor subunit 2, A to D
- NOARG :
-
NG-nitro-L-arginine
- NO° :
-
nitric oxide
- PBS :
-
phosphate-buffered saline
References
Banker B, Larroche JC 1962 Periventricular leukomalacia of infancy: a form of neonatal anoxic encephalopathy. Arch Neurol 7: 386–410.
Nelson KB, Ellenberg JH 1986 Antecedents of cerebral palsy: multivariate analysis of risk. N Engl J Med 315: 81–86.
Evrard P, Marret S, Gressens P 1997 Environmental and genetic determinants of neural migration and postmigratory survival. Acta Paediatr Scand Suppl 422: 20–26.
Murphy DJ, Sellers S, MacKenzie IZ, Yudkin PL, Johnson AM 1995 Case-control study of antenatal and intrapartum risk factors for cerebral palsy in very preterm singleton babies. Lancet 346: 1449–1454.
Zupan V, Gonzalez P, Lacaze-Masmonteil T, Boithias C, d'Allest AM, Dehan M, Gabilan JC 1996 Periventricular leukomalacia: risk factors revisited. Dev Med Child Neurol 38: 1061–1067.
Marin-Padilla M 1997 Developmental neuropathology and impact of perinatal brain damage: II. white matter lesions of the neocortex. J Neuropathol Exp Neurol 56: 219–235.
Ikonomidou C, Mosinger JL, Shahid Salles K, Labruyere J, Olney JW 1989 Sensitivity of the developing rat brain to hypobaric/ischemic damage parallels sensitivity to N-methyl-aspartate toxicity. J Neurosci 9: 2809–2818.
McDonald JW, Johnston MV 1990 Physiological and pathophysiological roles of excitatory amino acids during central nervous system development. Brain Res Rev 15: 41–70.
Lipton SA, Rosenberg PA 1994 Excitatory amino acids as a final common pathway for neurologic disorders. N Engl J Med 330: 613–622.
Gilles FH, Averill D, Kerre CS 1977 Neonatal endotoxin encephalopathy. Ann Neurol 2: 49–56.
Yoon BH, Kim CJ, Romero R, Jun JK, Park KH, Choi ST, Chi JG 1997 Experimentally induced intrauterine infection causes fetal brain white matter lesions in rabbits. Am J Obstet Gynecol 177: 797–802.
Yoshioka H, Goma H, Nioka S, Ochi M, Miyake M, Zaman A 1994 Bilateral carotid occlusion causes periventricular leukomalacia in neonatal dogs. Dev Brain Res 78: 273–278.
Oka A, Beliveau MJ, Rosenberg PA, Volpe JJ 1993 Vulnerability of oligodendroglia to glutamate: pharmacology, mechanisms, and prevention. J Neurosci 13: 1441–1453.
McDonald JW, Althomsons SP, Hyrc KL, Choi DW, Goldberg MP 1998 Oligodendrocytes are highly vulnerable to AMPA/kainate receptor-mediated excitotoxicity. Nature Med 4: 291–297.
Volpe JJ 1995 Neurology of the newborn. WB Saunders, Philadelphia, 279–313.
Marret S, Mukendi R, Gadisseux JF, Gressens P, Evrard P 1995 Effect of ibotenate on brain development: an excitotoxic mouse model of microgyria and posthypoxic-like lesions. J Neuropathol Exp Neurol 54: 358–370.
Marret S, Gressens P, Gadisseux JF, Evrard P 1995 Prevention by magnesium of excitotoxic neuronal death in the developing brain: an animal model for the clinical intervention studies. Dev Med Child Neurol 37: 473–484.
Marret S, Gressens P, Evrard P 1996 Arrest of neuronal migration by excitatory amino acids in hamster developing brain. Proc Natl Acad Sci USA 93: 15463–15468.
Vannucci RC, Perlman JM 1997 Interventions for perinatal hypoxic-ischemic encephalopathy. Pediatrics 100: 1004–1014.
Bac P, Maurois P, Dupont C, Pages N, Stables JP, Gressens P, Evrard P, Vamecq J 1998 Magnesium-deficiency-dependent audiogenic seizures (MDDASs) in adult mice: a nutritional model for discriminatory screening of anticonvulsant drugs and original assessment of neuroprotection properties. J Neurosci 18: 4363–4373.
Gressens P, Marret S, Hill JM, Brenneman DE, Gozes I, Fridkin M 1997 Vasoactive intestinal peptide prevents excitotoxic cell death in the murine developing brain. J Clin Invest 100: 390–397.
Gunn AJ, Gunn TR, de Haan HH, Williams CE, Gluckman PD 1997 Dramatic neuronal rescue with prolonged selective head cooling after ischemia in fetal lambs. J Clin Invest 99: 248–256.
Edwards AD, Wyatt JS, Thoresen M 1998 Treatment of hypoxic-ischemic brain damage by moderate hypothermia. Arch Dis Child 78:F85–F91.
Watanabe M, Inoue Y, Sakimura K, Mishina M 1992 Developmental changes in distribution of NMDA receptor channel subunit. Neuroreport 3: 1138–1140.
Zukin RS, Bennett MVL 1995 Alternative spliced isoforms of the NMDAR1 receptor subunit. TINS 18: 306–313.
Wenzel Fritschy JM, Mohler H, Benke D 1997 NMDA receptor heterogeneity during postnatal development of the rat brain: differential expression of the NR2A, NR2B, and NR2C subunit proteins. J Neurochem 68: 469–478.
Beal MF, Swartz KJ, Isacson O 1992 Developmental changes in brain kynurenic concentration. Dev Brain Res 68: 136–139.
Ceresoli G, Füller MS, Scwarcz R 1996 Excitotoxic lesions of the rat striatum: different responses of kynurenine pathway enzymes during ontogeny. Dev Brain Res 96: 61–69.
Andiné P, Lehman A, Ellren K, Wennberg E, Kjellmer I, Nielsen T, Hagberg H 1988 The excitatory amino acid antagonist kynurenic acid administered after hypoxicischemia in neonatal rats offers neuroprotection. Neurosci Lett 90: 208–212.
Dawson TM, Dawson V, Snyder SH 1992 A novel neuronal messenger molecule in brain: the free radical, nitric oxide. Ann Neurol 32: 297–311.
Moore PK, al-Swayeh OA, Chong NWS, Evans RA, Gibson A 1990 L-NG-nitroarginine, a novel, L-arginine-reversible inhibition of endothelium-dependent vasodilatation in vitro. Br J Pharmacol 99: 408–412.
Dwyer MA, Bredt DS, Snyder SH 1991 Nitric oxide synthase: irreversible inhibition by L-NG-nitroarginine in brain in vitro and in vivo. Biochem Biophys Res Commun 176: 1136–1141.
Lizasoain I, Weiner CP, Knowles RG, Moncada S 1996 The ontogeny of cerebral and cerebellar nitric oxide synthase in the guinea pig and rat. Pediatr Res 39: 779–783.
Buchan AM, Gertler SZ, Huang ZG, Li H, Chaundy KE, Xue D 1994 Failure to prevent selective CA1 neuronal death and reduce cortical infarction following cerebral ischemia with inhibition of nitric oxide synthase. Neuroscience 61: 1–11.
Hamada Y, Hayakawa T, Hattori H, Mikawa H 1994 Inhibitor of nitric oxide synthesis reduces hypoxic-ischemic brain damage in the neonatal rat. Pediatr Res 35: 10–14.
Dorrepaal CA, Shadid M, Steedijk P, van der Velde ET, Meinesz JH, van der Bor M, Baan J, van Bel F 1995 Prevention of postasphyxial brain injury by NG-nitro-L-arginine [Abstract]. Pediatr Res 37: 377
Wass CT, Lanier WL, Hofer RE, Scheithauer BW, Andrews PG 1995 Temperature changes of 1C alter functional neurologic outcome and histopathology in a canine model of complete cerebral ischemia. Anesthesiology 83: 325–335.
Degi R, Bari F, Beasley TC, Thrikawala N, Thore C, Louis TM, Busija DW 1998 Regional distribution of prostaglandin H synthase-type 2 and neuronal nitric oxide synthase in piglet brain. Pediatr Res 43: 683–689.
Chumas PD, Debigio MR, Drake JM, Tuor UI 1993 A comparison of the protective effect of dexamethasone to other potential prophylactic agents in a neonatal rat model of cerebral hypoxia-ischemia. J Neurosurg 79: 414–420.
Chow HS, Lynch JL, Rose K, Choï DW 1994 Trolox attenuates cortical neuronal injury induced by iron, ultraviolet light, glucose deprivation, or AMPA. Brain Res 639: 102–108.
Bagenholm R, Andiné P, Hagberg H 1996 Effects of the 21-amino steroid tirilazad mesylate (U-74006F) on brain damage and edema after perinatal hypoxia-ischemia in the rat. Pediatr Res 40: 399–403.
Dugan LL, Turetsky DM, Du C, Lobner D, Wheeler M, Almli CR, Shen CK, Luh TY, Choï DW, Lin TS 1997 Carboxyfullerenes as neuroprotective agents. Proc Natl Acad Sci USA 94: 9434–9439.
Chen N, Moshaver A, Raymond LA 1997 Differential sensitivity of recombinant N-methyl-D-aspartate receptor subtypes to zinc inhibition. Mol Pharmacol 51: 1015–1023.
Koh J-Y, Suh SW, Gwag BJ, He YY, Hsu CY, Choï DW 1996 The role of zinc in selective neuronal death after transient global cerebral ischemia. Science 272: 1013–1016.
Zhou FM, Hablitz JJ 1993 Zinc enhances GABA-ergic transmission in rat neocortical neurons. J Neurophysiol 70: 1264–1269.
Acknowledgements
The authors thank Dr. Janis Randall Simpson for critical reading of the English manuscript, and Ms. Eliane Abdelouab, Ms. Leslie Besse, and Ms. Anne-Marie Rona for their skillful technical assistance.
Author information
Authors and Affiliations
Additional information
Supported by grants from the INSERM (France) and the Fonds National pour la Recherche Scientifique (Belgium).
Rights and permissions
About this article
Cite this article
Marret, S., Bonnier, C., Raymackers, JM. et al. Glycine Antagonist and NO° Synthase Inhibitor Protect the Developing Mouse Brain against Neonatal Excitotoxic Lesions. Pediatr Res 45, 337–342 (1999). https://doi.org/10.1203/00006450-199903000-00008
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199903000-00008