Abstract
Obesity in adults is associated with an increased mortality rate from various diseases. Childhood overweight or obesity may persist into adulthood, and for this reason it is important to identify such children at risk. The data were taken from a larger longitudinal growth study of 3650 full-term and healthy Swedish babies followed from birth to 18 y of age. Body mass index (BMI) was used to estimate (during the pediatric years) the risk of obesity at 18 y of age. A probability chart for becoming overweight (>25 kg/m2) by 18 y of age was constructed, For example, in girls, a BMI of 16 kg/m2 at 4 y of age is associated with a 20% risk of attaining a BMI value over 25 kg/m2 at 18 y, and in boys at 4 y of age, a BMI of 19 kg/m2 leads to a 60% risk that they will have a BMI value over 25 kg/m2 at 18 y. The probability risk charts for adult overweight developed here is the first one presented. They provide an easy and novel instrument to use to identify those children who are at high risk of becoming obese adults, so that they may have clinical intervention at younger ages.
Similar content being viewed by others
Main
Obesity or overweight is related to many diseases in adults, such as cardiovascular diseases, hypertension, gallbladder disease, diabetes mellitus, atherosclerosis, gout, arthritis, and certain cancers (1, 2). Evidence can be provided from many previous studies that indicate that childhood obesity often persists into adulthood (3–5). It may thus be worthwhile to identify those children who are at high risk of becoming obese in adulthood, for clinical intervention as early as possible. To our knowledge, only one previous study has made efforts to estimate the likelihood curves of being overweight in adulthood, here at 35 y of age, using the body mass index (BMI) centile value in childhood (6). In their study, the 75th, 85th, and 95th BMI centile curves from 2 to 18 y of age were shaded differentially to indicate age ranges during which the probability of overweight at 35 y of age was either below 20%, 20–29.9%, 30–39.9%, or 40–80%. However, no precise probability curve was presented in their work for the full range of individual BMI values.
The aim of this study was to produce the probability charts for adult overweight for the pediatric ages. The series came from a large Swedish population-based longitudinal growth study of 3650 full-term babies followed from birth to 18 y of age (7).
METHODS
Subjects.
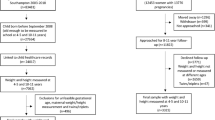
The study population was selected from 5111 final grade school children who were born in Gothenburg, or in the area surrounding that city, in Sweden. Because of the relatively unique school system in Sweden, more than 98% of children between the ages of 17 and 19 y remain within the school system, including those with mild or moderate problems in mental development. We believe that there is no important selection bias in the study population and that almost the whole cohort of children was involved. No information was obtained on 319 girls and 304 boys; some of them were not willing to provide such information, or they failed to attend the last investigation at school. Of the remaining children (n= 4488), 76.8% were born in 1974, 16.7% in 1973, 3.0% before 1973, and 3.5% in 1975. The exclusion criteria, such as multiple births, prematurity, growth disorders, and lack of information at birth were applied in the selection of subject (7). The data in analysis therefore represent 3650 full-term (37–42 wk of gestation), healthy Swedish children with growth information from birth to 18 y of age (7). The sample size for each gender varied between 582 and 1857 for the various ages; at 18 y of age, 1849 boys and 1801 girls remained.
Data collection.
The data were collected from April to November 1992. Four trained investigators from the International Pediatric Growth Research Centre, Department of Pediatrics, University of Gothenburg, and two school nurses comprised the study group. Weight and height of all of the children were measured in a standardized way with a calibrated Harpenden stadiometer. The information with regard to each child at birth and throughout the prenatal period, such as size at birth, length of gestation, and any health problems, was obtained from the Swedish Birth Register at the Swedish National Board for Health and Welfare. The other health records of children from birth to 18 y were taken from the notes made by doctors and nurses at the Child Health Centres or at schools. Among our study population, 99.2% had reached final height at 18 y of age when the study team visited the schools (7).
Quality of the data.
All growth data were computerized, and quality control analysis was performed. For the study group, 52,078 height-and-weight measurements were available from birth to the last examination, and the average number of measurements for each child was 14.4.
Ethical approval.
This study was approved by the Ethical Committee of the Medical Faculty, the University of Gothenburg, Sweden, and the Swedish Data Authorities. Written informed consent was received from the children and from the parents of those children who were less than 16 y old.
Data analysis.
The classification of BMI for adults from the International Obesity Task Force was chosen as one of the references in this study [underweight = BMI below 18.5 kg/m2; normal range = 18.5–24.9 kg/m2; overweight = 25.0–29.9 kg/m2; obese class I = 30.0–34.9 kg/m2; obese class II = 35.0–39.9 kg/m2; and obese class III = 40.0 kg/m2 or higher] (8). An international workshop on childhood obesity also established percentile cut-off points for obesity in childhood and adolescence that corresponded to the BMI of 25 and 30 in young adults (8). In this work, when the prediction model was made, a BMI value over 25 kg/m2 was defined as the cut-off point of overweight or obesity at 18 y of age.
The sensitivity and specificity of the probability charts were assessed by the raw BMI value of the whole study population.
To compute all statistics, we used Statistic Analysis System (SAS) software, 1996 SAS series, Version 6.10 (SAS Institute, Inc., Cary, NC) (9).
RESULTS
Spearman correlation coefficient for BMI at younger ages and BMI at18 y.
Figure 1 gives the correlation coefficient between BMI at all ages from birth to 17 y of age and BMI at 18 y of age. The values are similar for the two sexes and increase over the ages. The r2 over 0.50 is reached at about 10 y of age.
Prediction of adult overweight during the pediatric years:probability charts.
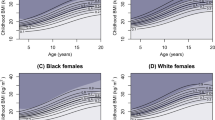
Figure 2, a and b, shows the probability charts for the prediction of subjects overweight at 18 y of age from 3 y of age. Those subjects overweight at 18 y of age are defined here as having a BMI value over 25 kg/m2 in both sexes. This means that some are not just overweight but are also obese, with a BMI over 30 kg/m2. With this kind of chart, we can, for example, estimate that a BMI of 16 kg/m2 at 4 y of age is associated with 0.2 probability or a 20% risk of attaining a BMI value over 25 kg/m2 at 18 y in girls (Fig. 2b). Another example is given in boys with a BMI of 19 kg/m2 at 4 y of age and who are at 60% risk of having a BMI value over 25 kg/m2 at 18 y (Fig. 2a).
(A) Probability chart for obtaining a BMI >25 kg/m2 for boys at 18 y of age. The five curves drawn from 3 to 17 y of age represent such a probability (or risk) of various magnitudes: 0.2 (20%), 0.3 (30%), 0.4 (40%), 0.5 (50%), and 0.6 (60%). (B) Probability chart for obtaining a BMI >25 kg/m2 for girls at 18 y of age. The five curves drawn from 3 to 17 y of age represent such a probability (or risk) of various magnitudes: 0.2 (20%), 0.3 (30%), 0.4 (40%), 0.5 (50%), and 0.6 (60%).
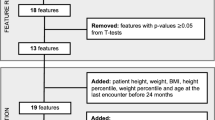
Construction of the probability charts.
The first step in producing the probability charts shown in Figure 2, a and b, is illustrated in Tables 1 and 2. For example, among boys with a BMI value over 6 kg/m2 at 4 y of age, 11% had reached a BMI value over 25 kg/m2 at 18 y of age. However, among the boys with a BMI over 19 kg/m2 at 4 y of age, 68.4% reached a BMI value over 25 kg/m2 at 18 y (Table 1). Note that the percentage represents the number of children who were overweight at 18 y of age for certain childhood BMI cut-off point value. For instance, in Table 1, at age 11 and a BMI cut-off value of >6, the corresponding percentage is 11.8. None of the boys of that age has a BMI value <6, so 11.8% represents all who were overweight at 18 y of age. It is not until we apply a cut-off point of >13 at 11 y that any boy will fall below the BMI cut-off point.
As a second step in the probability chart development, we fitted a fourth-degree polynomial function to the percentage values to represent the various cut-off points for certain gender and age, i.e., the values given in columns in Tables 1 and 2. An illustration of the curve fitting is shown in Figure 3 for girls at 4 y of age. Note that the increase in the percentage values for adult overweight increases rapidly over the BMI cut-off values at 4 y of age. From these age- and gender-specific polynomial functions, we could determine the pediatric BMI value associated with 20%, 30%, 40%, 50%, and 60% risk for adult overweight or obesity (Fig. 3). As noted in Tables 1 and 2, we could not undertake this curve fitting for values below 3 y of age, inasmuch as most of the risk values were below 20%.
An illustration of curve-fitting procedure of the risk (%, y axis) of adult overweight for certain BMI cut-off points (x axis) in girls at 4 y of age. The dots are the corresponding raw values given in Table 2. A fourth-degree polynomial function was fitted to the raw values, and this curve is given as the continuous line. From this function, the 20%, 30%, 40%, 50% and 60% risk-associated values for adult overweight were computed.
The last step in the construction of the probability charts was to fit a third-degree polynomial function to the values derived in step 2. For instance, the function was fitted to the BMI values associated with a 20% risk of adult obesity for boys from 3 to 17 y of age. The same procedure was also used for the 30%, 40%, 50%, and 60% BMI-related values for boys and girls, separately. Table 3 gives the parameters of the fitted function with the corresponding R2 values. These functions were used in the final construction of the probability charts as shown in Figure 2, a and b.
The RR for overweight at 18 y of age.
Results of a further analysis based on the risk functional curves for overweight at 18 y of age (Fig. 2, a and b) are given in Table 4. The analysis was made for subjects at 5 and 8 y only. For both ages, the children were divided into two groups according to the current BMI value in relation to a certain risk functional value (20–60%) for adult overweight. Within each of these two groups, we estimated the true percentage of overweight adult, i.e., where the BMI value is over 25 kg/m2 at 18 y of age. For instance, at 5 y of age, 18.52% of the children with a 20% or higher risk for adult overweight turned out to be overweight at 18 y of age. This is in contrast to 4.37% for adult overweight in the group with a BMI below the 20% risk functional value at 5 y of age. The RR for overweight at 18 y of age could also be computed. For example, a BMI value lying on or above the 20% risk curve at 5 y of age is associated with a RR of 4.24 of adults overweight, compared with a BMI below this risk curve. Because the correlation between BMI value at 8 and 18 y is higher than the correlation between 5 and 18 y, the relative risk (at 8 y of age) for overweight at 18 y of age (6.13–7.79) is higher than the risk at 5 y of age (4.11–5.76). The RR values keep fairly constant within the ages, although the risk functional values increased from 20% to 60%. Table 4 also serves as a feedback of the accuracy of the risk functional curves; the sensitivity value of the diagnostic instrument for adults overweight should equal the risk functional values (20–60%).
Figure 4 illustrates that the risk function for adult overweight are not necessarily similar for the two sexes. This is especially true for the higher risk functional values, such as 50% and 60%. Girls need higher BMI values in childhood than boys for similar risk value estimates for adult overweight.
DISCUSSION
A set of practical, simple, and novel probability charts for overweight at 18 y of age is the main result of our study. Such charts are presented here for the first time, and they are based on the largest current longitudinal growth study worldwide, consisting of 3650 full-term babies followed from birth to 18 y (7). These charts will provide a useful tool for pediatricians who want to identify those children who are at a high risk of becoming obese in adulthood, for clinical intervention as early as possible.
During the pediatric years, the prediction of adulthood obesity is a thorny problem, no matter which variables and methods are chosen. The precision of such a prediction method is very low until late childhood and becomes somewhat better during adolescence (6, 10). Some studies suggest that there is no optimal age during childhood for the prediction of overweight in adult life and that excessive weight gain may begin at any time (11). However, the urgent need for good predictors of adult obesity was put forward recently because of the dramatic increasing prevalence (12) and relatively unsuccessful treatment of obese adults. Furthermore, the scarce resources should be allocated to those children who are at high risk of adult obesity, because the long-term treatment programs developed for obese children are relatively expensive and time-consuming (13).
A set of prediction charts for obtaining a BMI value over 25 kg/m2 at 18 y of age was produced for boys and girls separately in our study. These charts provide a novel and easy way to estimate the risk of young adults (18 y old) becoming overweight, on the basis of the individual BMI value from 3 y of age onward. Using this kind of chart we can, for example, estimate that in girls, a BMI of 16 kg/m2 at 4 y of age is associated with a 0.2 probability or a 20% risk of attaining a BMI value over 25 kg/m2 at 18 y. Another example is given with a BMI of 19 kg/m2 at 4 y of age which leads to a 60% risk of having a BMI value over 25 kg/m2 at 18 y in boys.
We found a sex difference in the probability charts for adults overweight, especially for the higher risk functional values such as 50% and 60% (Fig. 4). Girls had a one-unit-higher BMI value during childhood than boys, for the same risk value estimates for adult overweight. It is difficult to find a good explanation for this difference. A plausible reason may be that girls are earlier in pubertal maturity and they obtain a relatively larger muscle mass than boys at 18 y of age.
The data used in our study came from a large longitudinal population-based growth study of Swedish children followed from birth to 18 y of age. This study represents the largest current longitudinal growth study worldwide; 87.7% of the total target population participated in the study. Although it is impossible to compare the background characteristics between the participants and nonparticipants according to the regulations of the Swedish Data Authority, there is little reason to believe that the main results presented in our study will be significantly influenced by the relatively low dropout rate. Details of the excluded children were given in a previous publication (7). Two hundred eighteen children were excluded as a result of multiple births or less than full-term pregnancies; 529 did not have data at birth because they were non-Swedish. The remaining 91 children were excluded because of chronic disease or because the mother had some major health problem during pregnancy.
The application of our probability charts for the prediction of adult overweight in other pediatric populations may be considered. Our charts were constructed on one of the leanest European populations, i.e., the Swedish, with the lowest obesity rate during last 2 decades (13). It may be that other populations with a higher prevalence of obesity show the same probability estimate for adult overweight presented here, but this remains to be tested.
There has been a report of only one previous study that estimated the risk of adult obesity, using BMI centile values in childhood (6). However, there are two limitations to comparing their risk charts with our prediction charts. First, it is obvious that the shape of their BMI centiles curves, especially 85th centiles for boys and girls, were different from the normal pattern. This might be due to the large variation caused by a relatively longer data collection period (from 1929 to 1991) or to the technical drawback of curve smoothing. Second, their probability chart of overweight at 35 y of age can be applied only to the certain groups (75th, 85th, and 95th BMI centile groups) to which the child belongs—not to the individual child. In addition, the probability might be different if the charts were to be applied to other ethnic groups in the United States, except for the white children included in the study.
A set of practical, simple, and novel probability charts for overweight at 18 y of age, based on the largest current longitudinal growth study world-wide, is reported for the first time in our study. These charts will provide a useful tool for pediatricians to use to identify those children who are at high risk of becoming overweight or obese adults, so that they may receive clinical intervention as early as possible.
Abbreviations
- BMI:
-
body mass index
- RR:
-
relative risk
- CI:
-
confidence interval
References
Van Itallie TB 1979 Obesity: adverse effects on health and longevity. Am J Clin Nutr 32: 2723–2733
Lew EA, Garfinkel L 1979 Variations in mortality by weight among 750,000 men and women. J Chronic Dis 32: 563–576
Abraham S, Nordseick M 1960 Relationship of excess weight in children and adults. Public Health Rep 75: 263–273
Lloyd JK, Wolff OH, Whelen WS 1961 Childhood obesity: a long-term study of height and weight. BMJ 2: 145–148
Charney E, Goodman HC, McBride M, Lyon B, Pratt R 1976 Childhood antecedents of adult obesity: do chubby infants become obese adults?. N Engl J Med 295: 6–9
Guo SS, Roche AF, Chumlea WC, Gardner JD, Siervogel RM 1994 The predictive value of childhood body mass index values for overweight at age 35 y. Am J Clin Nutr 59: 810–819
Karlberg J, Albertsson-Wikland K 1995 Growth in full-term small-for-gestational-age infants: from birth to final height. Pediatr Res 38: 1–7
Bouchard C 1997 Obesity in adulthood - The importance of childhood and parental obesity: editorials. N Engl J Med 337: 926–927
SAS Institute Inc., SAS User's Guide: Statistics, Version 6.10 Edition. Cary, NC: SAS Institute Inc., 1996
Gasser T, Ziegler P, Seifert B, Molinari L, Largo RH, Prader A 1995 Prediction of adult skinfolds and body mass from infancy through adolescence. Ann Hum Biol 22: 217–233
Stark O, Atkins E, Wolff OH, Douglas JWB 1981 Longitudinal study of obesity in the National Survey of Health and Development. BMJ 283: 13–17
Kuczmarski RJ, Flegal KM, Campbell SM, Johnson CL 1994 Increasing prevalence of overweight among US adults: the National Health and Nutrition Examination Surveys, 1960 to 1991. JAMA 272: 205–211
Rossner S 1998 Childhood obesity and adulthood consequences. Acta Pediatr 87: 1–5
Author information
Authors and Affiliations
Additional information
Supported by grants from the Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, and Pharmacia Upjohn, Inc., Stockholm, Sweden.
Rights and permissions
About this article
Cite this article
He, Q., Karlberg, J. Prediction of Adult Overweight during the Pediatric Years. Pediatr Res 46, 697 (1999). https://doi.org/10.1203/00006450-199912000-00012
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199912000-00012
This article is cited by
-
Longitudinal effects of parental, child and neighborhood factors on moderate-vigorous physical activity and sedentary time in Latino children
International Journal of Behavioral Nutrition and Physical Activity (2014)
-
Growth around puberty as predictor of adult obesity
European Journal of Clinical Nutrition (2008)
-
Tracking of body mass index during childhood: a 15-year prospective population-based family study in eastern Finland
International Journal of Obesity (2003)
-
The contribution of fat and fat-free tissue to body mass index in contemporary children and the reference child
International Journal of Obesity (2002)
-
Probability of Adult Overweight and Risk Change during the BMI Rebound Period
Obesity Research (2002)