Abstract
Inherited thrombocytopenias are a heterogenous group of disorders. Different criteria have been suggested to classify the forms, such as the inheritance mechanism and the platelet volume as well as the number and morphology of megakaryocytes. However, the classification is often descriptive, and the precise mechanism of thrombocytopenia still remains unknown. We describe the clinical, biologic, and molecular findings of an autosomal dominant thrombocytopenia in a large family. The 17 patients had normocellular bone marrow and normal platelet volume. Platelets also showed a normal aggregation test and normal response to ADP and thrombopoietin (TPO). In the affected subjects, the mean ± SD levels of platelet count and plasma TPO were 62 ± 25 and 258 ± 151, respectively. Comparative analysis showed that the patients with platelet count <70 000 had higher plasma TPO concentration. The data are consistent with a mild clinical form of the disease associated with only a few episodes of bleeding. To exclude the possible role of TPO and its receptor c-mpl in the etiology of this condition, linkage analysis was performed using microsatellite markers close to the TPO and c-mpl genes on chromosomes 3q26.3-q27 and 1p34, respectively. The absence of cosegregation within the affected family indicated that these genes, as well as two other candidate loci on chromosomes 11 and 21, are not responsible for this hereditary dominant form of thrombocytopenia. A genome-wide search and subsequent identification of the gene will provide new insight into the pathogenesis of this disorder.
Similar content being viewed by others
Main
Thrombocytopenias with variable clinical features and pathophysiology are both acquired and inherited disorders of children and adults. Among the genetic forms, some are characterized by the hypomegakaryocytic appearance of the bone marrow with a monolineage or multilineage involvement; others are characterized by normal megakaryocyte count (1–3). On the basis of the MPV, nonsyndrome forms could be classified as macrothrombocytopenia, microthrombocytopenia, and normothrombocytopenia (1–3). The last, inherited as an autosomal dominant trait (2–5), is usually severe enough in infants and patients that medical attention is sought because of bleeding problems. The prevalence of this condition is unknown. However, the incidence may be high because of individuals who are clinically asymptomatic. In fact, the recent widespread use of automated cell counters has led to an increase in the diagnosis of thrombocytopenia.
Many cytokines, including IL-1, -3, -6, and -11, granulocyte-macrophage colony-stimulating factor, erythropoietin, and TPO, are capable of stimulating megakaryocytopoiesis both in vivo and in vitro (6–9). TPO and its receptor c-mpl seem to play a central role in regulating platelet production (10, 11). TPO and c-mpl genes have been identified and mapped on chromosome 1p34 and 3q26.3-q27, respectively (12, 13). This knowledge facilitates further molecular investigations of the possible role of these candidate genes in hereditary thrombocytopenias.
In the present study, we describe the clinical, biologic, and molecular features of 17 patients, all members of the same family, with an autosomal dominant thrombocytopenia characterized by normocellular bone marrow, normal MPV, and normal aggregation tests. The plasma TPO levels were increased, yet they seemed lower than those shown in hypomegakaryocytic thrombocytopenias. Two candidate genes, TPO and c-mpl, as well as candidate loci on chromosomes 11 and 21 were excluded in the pathogenesis of this disorder by linkage analysis.
METHODS
Patients.
Seventeen thrombocytopenic patients were enrolled in the present study from a large four-generation Italian family of 38 subjects (Fig. 1). The great-grandparents were not available for the sampling; the great-grandfather was reported to have a history of bleeding and died from acute leukemia at the age of 69 y. After informed consent, 36 subjects were investigated (17 affected and 19 nonaffected members). Patient age ranged from 4 to 61 y, whereas the unaffected members were 8 to 63 y old. None of the affected individuals had birth defects. Two cases were diagnosed during the perinatal period. Six subjects had a clinical history of petechiae or excessive bruising and bleeding after dental surgery.
A peripheral citrate blood sample was obtained from each family member. Three subjects also had a bone marrow aspiration for diagnostic purposes. Platelet count was obtained in a Coulter Counter S-Plus. The Ivy bleeding time was normal or prolonged <2 min. Platelet-bound Ig test was performed by ELISA assay.
Ten subjects with FA served as controls; their clinical findings are described elsewhere (14). Ten healthy donors were also enrolled in this study. The present study was approved by the Institutional Ethical Committee of the University of Bari.
TPO serum levels.
TPO serum levels were measured by a quantitative sandwich enzyme immunoassay technique (R&D Systems, Minneapolis, MN). The detection limit of the assay was 5 pg/mL.
Platelet preparation and aggregation studies.
Nine volumes of blood obtained from two affected siblings (III-1 and IV-1) were withdrawn by venipuncture in 1 vol of 3.8% trisodium citrate. PRP was prepared by centrifugation for 15 min at 180 ×g. Platelet-poor plasma was obtained by centrifugation at 2000 ×g for 10 min. Platelet aggregation in PRP was performed as described by Born (15) at 37°C with a constant rate of stirring at 1000 rpm in the lumiaggregometer (Helena Laboratories, Beaumont, TX) and with platelet-poor plasma as reference. The number of platelets in PRP was adjusted to 1.5 × 10/mL. Preincubation was done directly in the lumiaggregometer with 450 mL of PRP for 5 min at 37°C under the following different conditions:1) with the TPO carrier (10 mL of PBS with 0.1% BSA/mL PRP);2) with 20 ng/mL rhTPO (Genzyme, Cambridge, MA) (20 mL of rhTPO/mL PRP, rhTPO resuspended 1 ng/mL); and 3) with 20 ng/mL rhTPO (sample unstimulated with ADP). A second agonist, 2 mM ADP, was added after 5 min in the first and second sample but not in the third (which was stimulated only by rhTPO, normally ineffective by itself on platelet aggregation) (16).
DNA extraction and linkage analysis.
High molecular mass DNA was extracted from peripheral blood leukocytes by use of an automatic DNA extractor (ABI DNA PURE) according to manufacturer's recommendations software (Applied Biosystems Inc., Foster City, CA). To examine the possible involvement of candidate genes and loci in this form of hereditary dominant thrombocytopenia, a linkage analysis was performed as described elsewhere (17, 18). Fluorochrome-labeled primers of the Linkage Mapping Set version 2 (Applied Biosystems Inc.) were used in PCR reactions according to the manufacturer's instructions. All markers located on chromosomes 1 and 3 as well as microsatellites D11S898, D11S908, D11S925, D11S4151, and D11S1320 on chromosome 11q and on chromosome 21q22 (D21S263, D21S1252) were analyzed. We also studied additional microsatellites on chromosomes 1p34 (D1S2828 and D1S2781) and 3q26.3–27 (D3S3725 and D3S3609), close to c-mpl and TPO loci, respectively. Data were collected using the GeneScan data collection program version 1.1 and analyzed using GeneScan data analysis software (Applied Biosystems Inc.). Correct allele size was assigned using the Genotyper software.
RESULTS
Patients.
Seventeen individuals from a large Italian family were affected by thrombocytopenia inherited as an autosomal dominant trait (Fig. 1). The male/female ratio was 1/1 and the age ranged from 4 to 61 y (mean 27.9 ± 17.5). Their platelet counts were from 31 to 109 (62 ± 25.7) × 109/L. Platelets in unaffected family members were 251 ± 66.5 × 109/L. No correlation between platelet count and patient age was found (r= −0.4;p= 0.11).
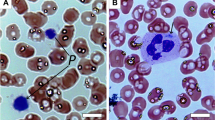
Leukocyte inclusions were not observed. Platelets had normal MPV ranging from 7.1 to 9.1 fL as well as normal morphology. No association was found between volume and count of the platelets. Further, affected and unaffected subjects showed no MPV difference. Three patients, III-3, IV-1, and IV-1's father (III-1), had a bone marrow aspiration for diagnostic purposes. They showed normal megakaryocyte number; however, the examination revealed rare but evident dysmegakaryocytopoietic phenomena such as micromegakaryocytes and megakaryocytes with a single nucleus and/or a delayed cytoplasmic maturation.
TPO serum levels and aggregation studies.
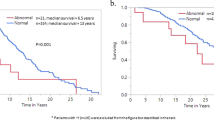
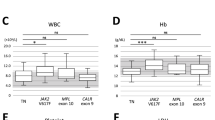
Plasma TPO could be measured in all family members with a minimum detection limit of 5 pg/mL. In the thrombocytopenic patients, TPO ranged from 63 to 572 pg/mL (mean ± SD, 258.5 ± 150.8), whereas, in the unaffected relatives, TPO ranged from 12 to 93 pg/mL (mean ± SD, 62.3 ± 29). Ten healthy donors were also tested. Values were similar to those in nonaffected family members, with TPO levels ranging from 5 to 91 (mean ± SD, 54.5 ± 12) and platelet count 198–403 × 109/L. Comparison of TPO levels between affected and unaffected members within this family showed a statistically significant difference (p< 0.001) (Fig. 2, A and C).
There was no correlation between TPO level and platelet count in thrombocytopenic patients (p= 0.1). When platelets were <70 000, a relative increase of plasma TPO concentration was observed; however, the difference was not statistically significant (mean ± SD, 293.5 ± 153 and 153 ± 85 for the patients with platelets below and above 70 × 109/L, respectively). This is probably because of the relatively low number of patients with platelet count above the threshold.
The plasma TPO in subjects with a different form of thrombocytopenia has also been reported (Fig. 2B). In FA patients, for instance, the mean value (1067 ± 812; range, 213–2769) was higher than in thrombocytopenic individuals (p< 0.03).
Platelet function.
Analysis of the platelet aggregation by standard methods failed to show any abnormality in the thrombocytopenic patients. In addition, platelet aggregation after TPO stimulation was also performed in two patients (III-1 and IV-1). In these individuals as well as in a control subject, treatment with TPO alone was unable to induce platelet aggregation (Fig 3a). Instead, it enhanced the secondary wave of platelet aggregation induced by ADP (Fig. 3b). The expected synergism of ADP with TPO was detected. The percentage of aggregation was overlapped in the two patients with thrombocytopenia.
Analysis of linkage.
Linkage analysis was performed between phenotype of the family members versus specific chromosomal regions containing the candidate genes as well as versus the entire chromosomes 1 and 3. Microsatellite markers flanking the TPO and c-mpl genes gave no evidence of linkage. At the same locus, the affected patients shared different alleles, but they shared the same alleles as unaffected relatives, showing the absence of cosegregation within the family. These negative results indicated that the regions examined do not likely contain the gene responsible for this form of thrombocytopenia. No evidence for linkage was obtained for two candidate loci on chromosomes 11q23–24 and 21q22. In fact, this chromosomal region was found to be deleted in all patients of a family with dominant thrombocytopenia (19).
DISCUSSION
Hereditary thrombocytopenias are rare and heterogeneous disorders. X-linked autosomal dominant and recessive forms are described in the literature. The increased number of reported cases, especially because of routine platelet counts in blood tests, suggests that this condition may not be so rare after all. Because the molecular disturbance remains unknown, cloning of the genes responsible for thrombocytopenias will be an important step toward understanding the pathogenesis and developing new therapeutic strategies.
In this article, we described a thrombocytopenia inherited as an autosomal dominant trait. The low platelet counts were often without symptoms. The volume and morphology of the platelets were normal. The platelet function, at least in terms of Ivy bleeding time and aggregation tests, was unremarkable in patients. These findings are consistent with a mild form of thrombocytopenia. In addition, no significant phenotypic variation was observed among patients, indicating the clinical homogeneity of the disease in the family. Moreover, the analysis of bone marrow suggested that the defect may affect the production of the platelets because of the normal megakaryocyte count.
Other autosomal dominant thrombocytopenias associated with a normal number of megakaryocytes and without thrombocytopathy have been reported in the literature (1–5, 19–22). Eight members of a family were afflicted by hemorrhagic diathesis as a result of mild thrombocytopenia (2). The platelets were morphologically normal and megakaryocytes were unremarkable in number and in appearance. Hypersegmented neutrophils and eosinophilia were present in all thrombocytopenic patients. Because MPV was not indicated, we cannot be sure this thrombocytopenia is comparable to our family. Splenectomy was reported to have been followed by improvement of the disease (5).
To increase the platelet number, two of our patients were treated with steroids, but without effects (data not shown).
A dominantly transmitted platelet disorder in another 22 members from a unique family seemed to differ from other well-defined platelet defects (22). Electron microscopy of platelets revealed normal thrombocytes. In that case, the platelet defect seemed to be associated with hematologic neoplasms such as leukemia or lymphoma. A review of 54 cases reported an MPV >10 fL (21). Acute myeloblastic leukemia preceded by a period of myelodysplasia was diagnosed in three families. Although the great-grandfather of our family died because of acute leukemia, no information on the biologic and molecular study of this leukemia has been documented.
Other hereditary dominant thrombocytopenias were described in association with macrothrombocytopenia (22), giant platelet granulation (21), or myopathy (1). In one family with dysmegakaryocytopoiesis and giant platelet α-granules, a deletion on chromosome 11q23 was described (21). Giant α-granules were not observed in our patients, and no rearrangements of chromosome 11 were detected (data not shown).
The dominant thrombocytopenia described in this article differs from others reported in the literature. It may represent a variant form of these disorders.
TPO is the major regulator of megakaryocytic cell proliferation and differentiation (23), although its action is not only restricted to this hemopoietic cell lineage (24). Its receptor c-mpl belongs to the cytokine receptor superfamily (13). It is expressed in the megakaryocytic lineages from late stem cells to platelets (25). The c-mpl receptor gene encodes for five mRNA isoforms, which are translated into four transmembrane (Mpl-P, Mpl-P-2, Mpl-K, Mpl-K-2) and one soluble (Mpl-S) proteins (26, 27). All these messengers are expressed in the platelets of patients with essential thrombocythemia and in healthy individuals (27). Distinct regions of the c-mpl receptor are involved in the signaling transduction, including Iak-STAT and Ras pathways, as well as in signals for the growth and differentiation of megakaryocytes (28, 29).
Plasma TPO seemed to be related to the peripheral platelet count when we compared the affected and nonaffected members of the present family. Interestingly, in FA patients, who have a thrombocytopenia due to a reduction of megakaryocytes, TPO values were more elevated (p= 0.03). In fact, the comparison of TPO levels between thrombocytopenic and FA individuals, both with similar platelet count, showed that the cytokine is higher in FA patients (Fig. 2, A and B). The mechanisms that regulate the production of TPO are not well known. Our results are consistent with the hypothesis that the number of both platelets (peripheral control) and megakaryocytes (central control) affects the plasma levels of the cytokine. TPO production seems to be induced by both hypomegakaryocytosis and thrombocytopenia even if the central control seems to be more relevant (30–32).
TPO serum level was found to be elevated and the platelet response to recombinant TPO and ATP was normal, suggesting that the cause of thrombocytopenia in this family is not likely to be due to a defect in the production of TPO and its receptor. However, point mutations in the TPO and c-mpl genes cannot be excluded as a cause for the platelet reduction. For this reason, linkage was examined on chromosomes 3q26.3-q27 and 1p34, the regions containing the TPO and c-mpl genes, respectively. No evidence for linkage was obtained, and the entire regions were therefore excluded. In addition, no linkage was obtained with microsatellite markers on chromosomes 11q23–24 and 21q22, in which other candidate loci were associated with genomic alterations in patients with dominant thrombocytopenia (19, 33). Segregation analysis showed that none of the four candidate loci contains the gene responsible for this condition. However, the large family allows the identification of the gene by positional cloning. The gene should be first localized by a genome-wide search and then cloned by mutation screening.
In conclusion, we described the clinical and biologic features of a hereditary dominant thrombocytopenia characterized by normocellular bone marrow and normal platelet physiology and volume. This form seems to be mild: in infancy, symptoms can be more evident, whereas, in adulthood, the disease could be asymptomatic even if platelet count continues to be low. TPO plasma level was higher in patients than in normal subjects. Because under the same platelet count, a 4-fold increase of TPO has been observed in FA patients, TPO production may be mainly regulated by both platelet and megakaryocyte number, which could be named “thrombotron,” an analogy of erythron. Linkage analysis excluded the regions containing the TPO and c-mpl genes as well as other candidate loci on chromosomes 11q23–24 and 21q22 from an involvement in this disease. Further investigations, including gene cloning, will provide insight into the molecular pathogenesis of hereditary thrombocytopenias.
Abbreviations
- TPO:
-
thrombopoietin
- c-mpl:
-
thrombopoietin receptor
- MPV:
-
mean platelet volume
- FA:
-
Fanconi's anemia
- PRP:
-
platelet-rich plasma
References
Najean Y, Lecompte T 1995 Hereditary thrombocytopenias in childhood. Semin Thromb Hemost 21: 294–304
Bithell TC, Didisheim P, Cartwright GE, Wintrobe MM 1965 Thrombocytopenia inherited as an autosomal dominant trait. Blood 25: 231–239
Bellucci S 1997 Megakaryocytes and inherited thrombocytopenias. Baillieres Clin Hematol 10: 149–162
Majado MJ, Gonzalez C, Tamayo M, Sanchez A, Moreno M 1992 Effective splenectomy in familial isolated thrombocytopenia. Am J Hematol 39: 70
Dowton SB, Beardsley D, Jamison D, Blattner S, Li FP 1985 Studies of a familial platelet disorder. Blood 65: 557–563
Hoffman R 1989 Regulation of megakaryocytopoiesis. Blood 74: 1196–1212
Gordon MS, Hoffman R 1992 Growth factors affecting human thrombocytopoiesis: potential agents for the treatment of thrombocytopenia. Blood 80: 302–307
Kishimoto T, Akira S, Taga T 1992 Interleukin-6 and its receptor: a paradigm for cytokines. Science 258: 593–597
Chang M, Suen Y, Meng G, Buzby JS, Bussel J, Shen V, Van der Ven C, Cairo MS 1996 Differential mechanisms in the regulation of endogenous levels of thrombopoietin and interleukin-11 during thrombocytopenia: insight into the regulation of platelet production. Blood 88: 3354–3362
de Sauvage F, Hass P, Specer S, Malloy B, Burney A, Spencer S, Darbonne W, Henzel W, Wonbg S, Kuang W, Oles K, Hultgren B, Solberg L, Goeddel D, Eaton D 1994 Stimulation of megakaryocytopoiesis and thrombopoiesis by the c-Mpl ligand. Nature 369: 533–538
Skoda RC, Seldin DC, Chiang MK, Peichel CL, Vogt TF, Leder P 1993 Murine c-mpl: a member of the hematopoietic growth factor receptor super family that transduces a proliferative signal. EMBO J 12: 2645–2651
Lok S, Kaushansky K, Holly R, Kuijper J, Lofton-Day C, Oort P, Grant F, Helpel M, Burkhead S, Kramer J, Bell L, Sprecher C, Blumberg H, Johnson R, Prunkard D, Ching A, Mathewes S, Bailey M, Forstrom J, Buddle M, Osborn S, Evans S, Sheppard P, Presnell S, O'Hara P, Hagen F, Roth G, Foster D 1994 Cloning and expression of murine thrombopoietin cDNA and stimulation of platelet production in vivo. Nature 369: 565–568
Vigon I, Florindo C, Fichelson S, Guenet JL, Mattei MG, Sourye M, Cosman D, Gisselbrecht S 1993 Characterization of the murine mpl proto-oncogene, a member of the hematopoietic cytokine receptor family: molecular cloning, chromosomal localization, and evidence for a function in cell growth. Oncogene 8: 2607–2615
Savoia A, Zatterale A, Del Principe D, Yoenye H 1996 Fanconi anemia in Italy: high prevalence of complementation group A in two geographic clusters. Hum Genet 97: 599–602
Born GVR 1962 Aggregation of platelets by adenosine diphosphate and its reversal. Nature 194: 927–930
Montrucchio G, Brizzi MF, Calosso G, Marengo S, Pegoraro L, Camussi G 1996 Effects of recombinant human megakaryocyte growth and development factor on platelet activation. Blood 87: 2762–2768
Carella M, Stewart G, Ajetunmobi JF, Perrotta S, Grootenboer S, Tchernia G, Delaunay J, Totaro A, Zelante L, Gasparini P, Iolascon A 1998 Genome-wide search for dehydrated hereditary stomatocytosis (hereditary xerocytosis): mapping of locus to chromosome 16 (16q23-qter). Am J Hum Genet 63: 810–816
Lathrop GM, Lalouel JM, Julier C, Ott J 1985 Multilocus linkage analysis in humans: detection of linkage and estimation of recombination. Am J Hum Genet 37: 482–498
Breton-Gorius J, Favier R, Guichard J, Cherif D, Berger R, Debili N, Vainchenker W, Douay L 1995 A new congenital dysmegakaryocytopoietic thrombocytopenia (Pris-Trousseau) associated with giant platelet alpha-granules and chromosome 11 deletion at 11q23. Blood 85: 1805–1813
Murphy S, Oski FA, Gardner FH 1969 Hereditary thrombocytopenia with an intrinsic platelet defect. N Engl J Med 281: 857–862
Najean Y, Lecompte T 1990 Genetic thrombocytopenia with autosomal dominant transmission: a review of 54 cases. Brit J Haematol 74: 203–208
Fabris F, Cordiano I, Salvan F, Ramon R, Valente M, Luzzatto G, Girolami A 1997 Chronic isolated macrothrombocytopenia with autosomal dominant transmission: a morphological and qualitative platelet disorder. Eur J Haematol 58: 40–45
Bartley TD, Bogenberger J, Hunt P, Li YS, Lu HS, Martin F, Chang MS, Samal B, Nichol JL, Swift S, Johnson MJ, Hsu RY, Parker VP, Suggs S, Skrine JD, Merewether LA, Clogston C, Hsu E, Hokom MM, Hornkohl A, Choi E, Pangelinan M, Sun Y, Mar V, McNinch J, Simonet L, Jacobsen F, Xie C, Shutter J, Chute H, Basu R, Selander L, Trollinger D, Sieu L, Padilla D, Trail G, Elliot G, Izumi R, Covey T, Crouse J, Garcia A, Xu W, del Castillo J, Biron J, Cole S, Hu MCT, Pacifici R, Ponting I, Saris C, Wen D, Yung YP, Lin H, Bosselman RA 1994 Identification and cloning of a megakaryocyte growth and development factor that is a ligand for the cytokine receptor Mpl. Cell 77: 1117–1124
Kobayashi M, Laver JH, Kato T, Miyazaki H, Ogawa M 1995 Recombinant human thrombopoietin (Mpl ligand) enhances proliferation of erythroid progenitors. Blood 86: 2494–2499
Debili N, Wendling F, Cosman D, Titeux M, Florindo C, Dusanter-Fourt I, Schooley K, Methia N, Charon M, Nador R, Bettaieb A, Vainchenker W 1995 The Mpl receptor is expressed in the megakaryocytic lineage from late progenitors to platelets. Blood 85: 391–401
Mignotte V, Vigon I, Boucher-de-Crevecoeur E, Romeo PH, Lemarchandel V, Chretien S 1994 Structure and transcription of the human c-mpl gene (MPL). Genomics 20: 5–12
Kiladjian JJ, Elkassar N, Hetet G, Briere J, Grandchamp B, Gardin C 1997 Study of the thrombopoietin receptor in essential thrombocythemia. Leukemia 11: 1821–1826
Nagata Y, Todokoro K 1995 Thrombopoietin induces activation of at least two distinct signaling pathways. FEBS Lett 377: 497–501
Takatoku M, Kametaka M, Shimizu R, Miura Y, Komatsu N 1997 Identification of functional domains of the human thrombopoietin receptor required for growth and differentiation of megakaryocytic cells. J Biol Chem 272: 7259–7263
Emmons RVB, Reid DM, Cohen RL, Meng G, Young NS, Dunbar CE, Shulman NR 1996 Human thrombopoietin levels are high when thrombocytopenia is due to megakaryocyte deficiency and low when due to increased platelet destruction. Blood 87: 4068–4071
Porcelijin L, Folman CC, Bossers B, Huiskes E, Overbeeke MA, von dem Schoot CE, de Haas M, von dem Borne AE 1998 The diagnostic value of thrombopoietin level measurements in thrombocytopenia. Thromb Haemost 79: 1101–1105
Ballmaier M, Schulze H, Straub G, Cherkaoui K, Wittner N, Lynen S, Wolters S, Bobenberger J, Welte K 1997 Thrombopoietin in patients with congenital thrombocytopenia and absent radii: elevated serum levels, normal receptor expression, but defective reactivity to thrombopoietin. Blood 90: 612–619
Ho YC, Otterud B, Legare RD, Varvil T, Saxena R, DeHart DB, Kohler SE, Aster JC, Dowton SB, Li FP, Leppert M, Gilliland G 1996 Linkage of a familial platelet disorder with propensity to develop myeloid malignancies to human chromosome 21q 22: 1–222. Blood 87: 5218–5224
Author information
Authors and Affiliations
Additional information
Supported by Associazione Italiana per la Ricerca sul Cancro (AIRC), the Italian Ministry of Health, MURST 40%, and Consiglio Nazionale delle Ricerche. The work carried out in the laboratory of A.I. has been supported in part by the Comitato Promotore Telethon (Grant E.645).
Rights and permissions
About this article
Cite this article
Iolascon, A., Perrotta, S., Amendola, G. et al. Familial Dominant Thrombocytopenia: Clinical, Biologic, and Molecular Studies. Pediatr Res 46, 548 (1999). https://doi.org/10.1203/00006450-199911000-00010
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199911000-00010
This article is cited by
-
Erblich bedingte Thrombozytopenien
Monatsschrift Kinderheilkunde (2006)